Rehabilitation of Peripheral Nerve Injuries in Disasters and Conflicts: Difference between revisions
No edit summary |
No edit summary |
||
| Line 108: | Line 108: | ||
== Assessment of Peripheral Nerve Injury == | == Assessment of Peripheral Nerve Injury == | ||
The assessment of a patient with a peripheral nerve injury following a sudden onset disaster should follow the same format as a standard [[Assessment Considerations in Disasters and Conflicts|rehabilitation assessment]], with a focus on neural to determine whether a muscle or area of skin is neurally intact. You can review assessment considerations in disaster and conflicts [[Assessment Considerations in Disasters and Conflicts|here]]. | The assessment of a patient with a peripheral nerve injury following a sudden onset disaster should follow the same format as a standard [[Assessment Considerations in Disasters and Conflicts|rehabilitation assessment]], with a focus on neural to determine whether a muscle or area of skin is neurally intact. You can review assessment considerations in disaster and conflicts [[Assessment Considerations in Disasters and Conflicts|here]]. | ||
* Function: | Specific considerations during assessment for patients with known or suspected peripheral nerve injury should include the following during the subjective and objective exam. <ref name=":2" /> | ||
=== Subjective === | |||
Questioning around function, sleep and sensation; | |||
* '''Function:''' | |||
** Determine what function is affected, e.g. dressing, washing, working and caring for dependents. Hand dominance is important in hand and arm injuries and will influence the impact of any upper limb injury | ** Determine what function is affected, e.g. dressing, washing, working and caring for dependents. Hand dominance is important in hand and arm injuries and will influence the impact of any upper limb injury | ||
* Sleep: | * '''Sleep:''' | ||
** Determine if sleep is affected by pain or their ability to get into a comfortable position at night. If sleep is impacted, finding a comfortable sleeping position should be an early treatment goal. | ** Determine if sleep is affected by pain or their ability to get into a comfortable position at night. If sleep is impacted, finding a comfortable sleeping position should be an early treatment goal. | ||
* Sensation: | * '''Sensation:''' | ||
** Determine the presence of pins and needles, numbness and reduced sensation/feeling. <ref name=":2" /> | ** Determine the presence of pins and needles, numbness and reduced sensation/feeling. <ref name=":2" /> | ||
=== Objective === | |||
* '''Sensory Testing:''' | |||
** A sensory test can serve as a quick check for nerve damage, in a setting where a full examination is difficult, e.g. in the presence of multiple fractures and an external fixator. | |||
* '''Motor Testing:''' | |||
** Major peripheral nerve injuries usually lead to severe muscle weakness and consequential atrophy, which can start 72 hours after injury. The neuromuscular junction undergoes significant changes after nerve injury and is the most critical point for functional recovery, even after proper nerve regeneration. Beside the manual muscle testing examination, there are motor nerve function tests that can detect muscle weakness of upper and lower limb peripheral nerve injuries. Pick one muscle for each peripheral nerve to check for nerve function and record strength. Choose at least one functional movement for the affected area. | |||
* '''Peripheral Pulses''' | |||
** Peripheral pulses can be used as a valuable clinical tool for a suspected peripheral nerve injury. | |||
=== Common Peripheral Nerve Injuries === | === Common Peripheral Nerve Injuries === | ||
| Line 391: | Line 406: | ||
| Gluteal Nerve | | Gluteal Nerve | ||
| | | | ||
* Hip Dislocation | |||
* | * | ||
| | | | ||
* [[Gluteus Medius]] | * [[Gluteus Medius]] | ||
| | | | ||
* Hip Abduction | * Impaired Hip Abduction | ||
| | | | ||
| | | | ||
| Line 401: | Line 418: | ||
|- | |- | ||
|[[Femoral Nerve]] | |[[Femoral Nerve]] | ||
L2 - L4 Nerve Root | |||
| | | | ||
* Fracture Pelvis | |||
* Fracture Hip | * Fracture Hip | ||
* Acetabular Fracture | * Acetabular Fracture | ||
* Stab Wounds | * Stab Wounds | ||
| Line 411: | Line 429: | ||
* [[Quadriceps Muscle|Quadriceps]] | * [[Quadriceps Muscle|Quadriceps]] | ||
| | | | ||
* Flexion Hip | * Impaired Flexion Hip | ||
* Extension Knee | * Impaired Extension Knee | ||
* Decreased Patellar Tendon Reflex | |||
| | | | ||
* Anterior Thigh | * Anterior Thigh | ||
| Line 421: | Line 440: | ||
|- | |- | ||
|[[Tibial Nerve]] | |[[Tibial Nerve]] | ||
L4 - S3 Nerve Root | |||
| | | | ||
* Dislocation Knee | * Dislocation Knee | ||
| Line 427: | Line 447: | ||
* Laceration Injury | * Laceration Injury | ||
| | | | ||
* [[Popliteus]] | * [[Biceps Femoris]] - Long Head[[Popliteus]] | ||
* [[Gastrocnemius]] | * [[Gastrocnemius]] | ||
* [[Soleus]] | * [[Soleus]] | ||
| Line 434: | Line 454: | ||
* Flexor Hallucis Longus | * Flexor Hallucis Longus | ||
| | | | ||
* Impaired Plantarflexion | |||
* Impaired Inversion | |||
* Unable to Curl Toes | |||
| | | | ||
* Bottom of the foot and toes, | |||
| | | | ||
* Unable to walk on toes | * Unable to walk on toes | ||
|- | |- | ||
|[[Common Peroneal Nerve|Peroneal Nerve]] | |[[Common Peroneal Nerve|Peroneal Nerve]] | ||
L4 - S2 Nerve Root | |||
| | | | ||
* Dislocation Knee | * Dislocation Knee | ||
| Line 447: | Line 472: | ||
* [[Tibialis Anterior]] | * [[Tibialis Anterior]] | ||
| | | | ||
* Impaired Dorsiflexion | |||
* Impaired Eversion | |||
* Footdrop | |||
* Steppage Gait | |||
| | | | ||
* Lateral surface of the lower leg, | |||
* Dorsum of the feet and toes, except for the space between the first and second toe | |||
| | | | ||
* Unable to walk on heels | * Unable to walk on heels | ||
Revision as of 22:49, 24 April 2022
Original Editors - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Tarina van der Stockt, Kim Jackson and Jess Bell
Introduction[edit | edit source]
Peripheral nerves can sustain injury from numerous causes including traumatic thermal, chemical, or mechanical injury, inherited causes, infections, collagen or metabolic diseases (diabetes mellitus being one of the most common), exposure to endogenous or exogenous toxins; malignancies and iatrogenic causes[1], which manifest with neurological deficits distal to the level of the lesion. In disaster and conflict situations there can be a significant increase in the number of traumatic peripheral nerve injuries, but all of these other causes of nerve injury will continue to be seen by patients in these situations. [2] In disaster and conflict situations patients with peripheral nerve injuries tend to present with other injuries, often complex and most frequently associated with limb fractures. In many cases these associated injuries need stabilised prior to the peripheral nerve injury being treated, which can often result in a delay in identification and treatment of the peripheral nerve injury.
Disasters including earthquakes and storms can lead to large numbers of peripheral nerve injuries, as a result of complex limb trauma and crush injuries, or those which incur deep soft tissue injuries from flying debris, while in conflict situations, peripheral nerve injuries are also associated with complex injuries as a result of explosives devices, gunshot wounds, and penetrating injuries. Primary injury to the nerve is generally a result of the same trauma that injures the bone or joint, but can also occur as a result of moving the patient or stretching, or manipulation of the limb while treating the injury, rather than by the initial force. Infection, scar, callus, or vascular complications including haematoma, arteriovenous fistula, ischemia, or aneurysm can also result in secondary injury to the nerve. [3]
In traumatic nerve injuries upper limb radial nerve injuries are most the common with 14% associated with humeral shaft fractures, 3% associated with fracture of the middle third of the humerus; 50%, with fracture of the distal third of the humerus; 7%, with supracondylar fracture of the humerus; and 7%, with dislocation of the radial head, while in shoulder dislocations it is the axillary nerve that may be injured as a result of stretch injuries, although this is rare and only occurs in about 5% of shoulder dislocations. Ulnar injuries account for 30% of patients with combined skeletal and neural injuries to the upper limb, and are generally associated with fractures of the medial humeral epicondyle, but often as a result of callus formation around the elbow. While elbow dislocations tend to result in median nerve injury in about 15% of combined skeletal and neural injuries of the upper limb, or after injury to the distal forearm of wrist. [4] In the lower limb it is the peroneal nerve that is most commonly injured at the fibular neck, as a result of fracture of the tibia and fibula or dislocation of the knee, while the tibial nerve is injured more in distal fractures of the tibia or ankle. Lumbosacral plexus branches are injured in in less than 3% of pelvic fractures; and in 10% to 13% of posterior dislocations of the hip. [4]
In conflict situations nerve injuries are generally distributed evenly between the upper and lower limbs, with explosions (63%) the main cause of peripheral nerve injury with 82% nerve injuries associated with open injuries, and a portion of patients presenting with injury to two or more nerves. [5] Associated injuries included fractures (31.1%), multiple multiple peripheral nerve injuries (76.8%), vascular injury (30.4%), and traumatic brain injury (34.1%), [6] with the lower extremity the most common site of the single most significant injury.[5] Neurapraxia (45%) is the most common type of injury to the nerve, followed by axonotmesis (35%) and neurotmesis (20%). The ulnar, common peroneal and tibial nerves were most commonly injured, and in a large portion of these injuries was associated with a vascular injury, fracture, or both at the level of the nerve lesion, which is a small number of situation s result in amputation secondary to major tissue loss and the level of nerve damage.[7] In conflict situations research suggests that there was no association between Sunderland Classification and time to evaluation, mechanism of injury, or nerve injured, but the Sunderland Classification was correlated with final motor and final sensory scores highlighting that those with with more severe initial injuries having worse final outcomes. [8]
In disaster and conflict situations peripheral nerve injuries are generally associated with multiple injuries, and can be missed when medical or surgical team prioritise working to save limb or life, and rehabilitation professionals are often the first member of the team to identify possible nerve injury during their assessment. As such rehabilitation professionals should always ensure that every patient who has injured a limb or limb girdle should be evaluated and monitored for any possible peripheral nerve damage, in particular post surgery, manipulation, casting, and recovery from any limb injury to detect any possible primary or secondary neural injury.[3] While timely referral for most peripheral nerve injuries does not always occur in disaster and conflict situations, research does suggest that a shorter time to presentation does led to improved sensory recovery. As such rehabilitation professionals involved in early rehabilitation play a key role in both identification and management of peripheral nerve injuries to ensure optimal recovery. [6]
Peripheral Nerve Injury Overview[edit | edit source]
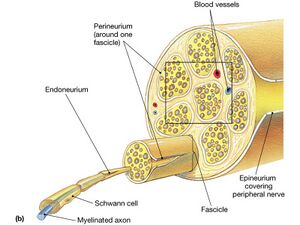
The peripheral nervous system consists of the nerves that branch out from the brain and spinal cord. These nerves form the communication network between the central nervous system and the body parts. A nerve contains bundles of nerve fibers, either axons or dendrites, surrounded by connective tissue. Sensory nerves contain only afferent fibers, long dendrites of sensory neurons, providing an area of skin with sensation. Motor nerves have only efferent fibers, long axons of motor neurons supplying the muscles. Mixed nerves contain both types of fibers and are involved in both sensory and motor function. [9][10] A connective tissue sheath called the epineurium surrounds each nerve. Each bundle of nerve fibers is called a fasciculus and is surrounded by a layer of connective tissue called the perineurium. Within the fasciculus, each individual nerve fiber, with its myelin and neurilemma, is surrounded by connective tissue called the endoneurium. A nerve may also have blood vessels enclosed in its connective tissue wrappings.[9]
A peripheral nerve injury can result in a minor injury up to a full transection of the nerve. Based on the type and amount of damage, nerve regeneration may or may not be possible. Peripheral nerve injury treatment will depend on the type of injury, amount of nerve injury sustained and symptoms which can include pain (ranging from a tingling to intense burning pain), numbness or altered sensations, muscle weakness in the affected body part, loss of function (eg. a hand or leg being difficult to use whilst performing tasks), loss of active movement (eg. wrist drop and foot drop), joint stiffness and emotional stress. [9]
Mechanisms of Injury[edit | edit source]
Nerve injury can occur as a result of from traction/stretch, laceration, compression, or ischemia. The nerve dysfunction results primarily from the direct mechanical forces applied to it and secondarily from the vascular compromise that follows, with consequent ischemic nerve damage.
Laceration[edit | edit source]
A nerve can be lacerated or completely transected as a consequence of a traumatic injury. This is more likely to occur as a result of a penetrating injury mechanism (eg, knife wound, gunshot, flying debris), rather than a blunt injury mechanism. Laceration to the nerves may also be accidentally cut during surgery, e.g. a misplaced fixator pin cutting the peroneal nerve.[11]
Traction / Stretch[edit | edit source]
Peripheral nerves allow for a significant degree of tension or stretch before developing internal/external structural damage, in part due to length redundancy that allows the nerve to adapt to stretching during normal movements of the limb (eg, the ulnar nerve at the elbow), allowing for stretching up to 10 percent with minimal traumatic consequences. However, when the nerve peripheral nerve is stretched beyond these limits both internal and external damage to the nerve can occurs.[12] Rapid-stretch nerve injuries are among the most devastating lesions to peripheral nerves, often resulting in poor functional outcomes. Specific nerves are more susceptible than others to trauma from stretch due to their location and level of resting tension, including nerves around the brachial plexus, in particular the axillary nerve.[11] Peripheral nerves may be injured by being stretched beyond its limit if a person is pulled by the limb through rubble or a narrow space after a building collapse.
Compression[edit | edit source]
External pressure can injure the nerve through compressive forces, which can either be continuously applied for hours at a time, such as occurs with compressive radial neuropathy ("Saturday Night Palsy") or following a crush injury, or repeatedly applied with cumulative effect, such as in habitual leaning on the elbow. More commonly, the nerves can be chronically compressed by abnormal neighboring structures, or while passing through fibro-osseous spaces such as with carpal tunnel syndrome or in situations with swelling such as compartment syndrome. [11][13] Compression injury may occur to the nerve when a person or a limb is crushed, e.g. trapped under debris in a collapsed building, or in compartment syndrome (see Fractures chapter), e.g. compression of the radial nerve with crushed/swollen arm.[13] It is worth noting that sensory information is transported in the outer layer of the nerve tissue, and so in compression injuries sensation is often more impacted than power or motor function.[3]
Combined Mechanisms[edit | edit source]
In disaster and conflict situations in many cases peripheral nerve injuries are a result of a combination of the above mechanisms. Vehicle-related injuries are predominantly stretch/traction injuries, although both contusion and laceration may also occur, missile-related injuries (eg, gunshot wounds) more commonly cause nerve contusions or transection, while laceration injuries occur most commonly as a result of sharp objects (eg, knife wound, gunshot, flying debris). Compression injuries often occur following building collapse or tend to relate to body positioning during anesthesia or surgeries; which are usually a result of a combination of contusion, compression and ischemia. Any injury with significant soft tissue damage that can also cause swelling may also cause subsequent compression.[11]
Classification of Peripheral Nerve Injuries[edit | edit source]
Classification systems provides a common language for medical and rehabilitation professionals to effectively discuss nerve pathophysiology based upon the severity and extent of injury to the structural components of the peripheral nerve. Classification systems also play an important role in prognosis prediction and treatment strategy determination. [9]
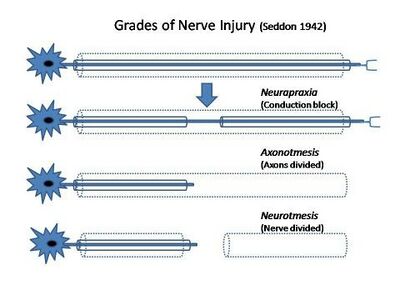
There are two commonly used classification systems in use for peripheral nerve injury; the Seddon Classification developed in 1942 and the Sunderland Classification first proposed in 1990. [2][11][14] Seddon was the first to classify nerve injuries into three categories; neurapraxia, axonotmesis, and neurotmesis, based on the presence of demyelination and the extent of damage to the axons and the connective tissues of the nerve. Sunderland later expanded on this initial classification to distinguish the extent of damage in the connective tissues. McKennon and Dellon introduced a further classification to denote combinations of Grade III-V injuries along the route of the damaged nerve, although it is not as widely accepted in use.[11][15][16]
| Seddon Classification | Sunderland Classification | Mechanism of Injury | Level of Injury | Potential for Recovery & Timeline | |
|---|---|---|---|---|---|
| Neuropraxia | Grade I | Usually caused by a mild injury |
|
| |
| Axonotmesis | Grade II | Typically occurs as a result of crush injuries, nerve stretch injuries (eg, motor vehicle accidents, falls), or percussion injuries (eg, gunshot wounds). |
|
Good likelihood of full recovery but slower recovery. |
|
| Grade III |
|
Potential for partial recovery. Surgery often required. | |||
| Grade IV |
|
Potential for partial recovery, with less than 100% recovery. Surgery generally required. | |||
| Neurotmesis | Grade V | Most often occurs in association with severe lesions, such as sharp injuries, traction injuries, percussion, or exposure to neurotoxic substances. |
|
| |
In disaster and conflict situations with traumatic peripheral nerve injuries most lesions are mixed and a single traumatic event can cause a combination of neurapraxia, axonotmesis, and neurotmesis in various degrees. As such the final prognosis and functional outcome depends on the ratio between the individual components of the injury, which may be difficult to assess clinically.[11]
Observation and conservative treatment (e.g., activity modification, splinting, electrical stimulation) are indicated in most closed injuries, which have a high rate of spontaneous recovery, while open injuries typically require surgical treatment, which is highly specialised and may not be available in conflicts and disasters, or the available, limited surgical resources may be prioritised for life saving interventions. Surgical interventions where available can include primary repair (end to end), which connects the two ends of a severed nerve and is the ideal surgical option; however, this should be completed within the first few days of injury and without any stretch or tension through the repair site, which requires the injury to be identified early. Nerve grafting (to bridge gaps in nerves) is the other approach that can be used that can occur at a later date than primary repair, but must still take place within two years of the initial injury. The grafts can either be an autograft, whereby healthy nerve tissue is transplanted from elsewhere in the patient’s own body or an allograft, where a commercially processed scaffold is used. [3]
Assessment of Peripheral Nerve Injury[edit | edit source]
The assessment of a patient with a peripheral nerve injury following a sudden onset disaster should follow the same format as a standard rehabilitation assessment, with a focus on neural to determine whether a muscle or area of skin is neurally intact. You can review assessment considerations in disaster and conflicts here.
Specific considerations during assessment for patients with known or suspected peripheral nerve injury should include the following during the subjective and objective exam. [3]
Subjective[edit | edit source]
Questioning around function, sleep and sensation;
- Function:
- Determine what function is affected, e.g. dressing, washing, working and caring for dependents. Hand dominance is important in hand and arm injuries and will influence the impact of any upper limb injury
- Sleep:
- Determine if sleep is affected by pain or their ability to get into a comfortable position at night. If sleep is impacted, finding a comfortable sleeping position should be an early treatment goal.
- Sensation:
- Determine the presence of pins and needles, numbness and reduced sensation/feeling. [3]
Objective[edit | edit source]
- Sensory Testing:
- A sensory test can serve as a quick check for nerve damage, in a setting where a full examination is difficult, e.g. in the presence of multiple fractures and an external fixator.
- Motor Testing:
- Major peripheral nerve injuries usually lead to severe muscle weakness and consequential atrophy, which can start 72 hours after injury. The neuromuscular junction undergoes significant changes after nerve injury and is the most critical point for functional recovery, even after proper nerve regeneration. Beside the manual muscle testing examination, there are motor nerve function tests that can detect muscle weakness of upper and lower limb peripheral nerve injuries. Pick one muscle for each peripheral nerve to check for nerve function and record strength. Choose at least one functional movement for the affected area.
- Peripheral Pulses
- Peripheral pulses can be used as a valuable clinical tool for a suspected peripheral nerve injury.
Common Peripheral Nerve Injuries[edit | edit source]
Upper Limb[edit | edit source]
- Proximal nerve lesions, are more likely to cause hand distortions (e.g. hand of benediction), which are only visible when the patient tries to flex the fingers or make a fist.
- Distal nerve lesions are more likely to cause claw deformities (e.g. ulnar claw or median claw) as a result in a loss of function with intact extrinsic flexors [17]
| Nerve | Related Injuries | Muscle Affected | Motor Function | Sensation | Test |
|---|---|---|---|---|---|
| Spinal Accessory Nerve |
|
|
Posture
Test
| ||
| Long Thoracic Nerve
C5 - C7 Nerve Root |
|
|
| ||
| Axillary Nerve
C5-C6 Nerve Root |
|
|
|
| |
| Suprascapular Nerve
C4 - C6 Nerve Root |
|
|
| ||
| Musculocutaneous Nerve
C5 - C7 Nerve Root |
|
|
|
| |
| Ulnar Nerve
C8 - T1 Nerve Root |
|
Forearm: | High Lesion - Ulnar Paradox;
|
|
|
| Hand
Hypothenar Eminence; Thenar Eminence; Short Muscles; |
Low Lesion - Partial Claw / Ulnar Claw;
|
| |||
| Radial Nerve
C5 - T1 Nerve Root |
|
Arm | High Lesion;
|
|
|
| Forearm; | Middle & Low Lesion;
| ||||
| Median Nerve
C5 - T1 Nerve Root |
|
Forearm; | High Lesion;
|
|
|
Low Lesion;
| |||||
| Hand; LOAF | Carpal Tunnel;
|
Lower Limb[edit | edit source]
| Nerve | Related Injuries | Muscle Affected | Motor Function | Sensation | Test |
|---|---|---|---|---|---|
| Gluteal Nerve |
|
|
|||
| Femoral Nerve
L2 - L4 Nerve Root |
|
|
|
| |
| Tibial Nerve
L4 - S3 Nerve Root |
|
|
|
|
|
| Peroneal Nerve
L4 - S2 Nerve Root |
|
|
|
|
Resources[edit | edit source]
Early Rehabilitation in Conflict and Disasters, Humanity and Inclusion
Rehabilitation in Sudden Onset Disasters, Humanity and Inclusion
References [edit | edit source]
- ↑ Mayo Clinic. Peripheral Neuropathy. Available from: https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061 (Last Accessed 24/03/2019)
- ↑ 2.0 2.1 2.2 Campbell WW. Evaluation and Management of Peripheral Nerve Injury. Clinical Neurophysiology. 2008 Sep 30;119(9):1951-65.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Lathia C, Skelton P, Clift Z. Early Rehabilitation in Conflicts and Disasters. Handicap International: London, UK. 2020.
- ↑ 4.0 4.1 Azar FM, Canale ST, Beaty JH. Campbell's Operative Orthopaedics, E-Book. Elsevier Health Sciences; 2020 Dec 23.
- ↑ 5.0 5.1 Birch R, Misra P, Stewart MP, Eardley WG, Ramasamy A, Brown K, Shenoy R, Anand P, Clasper J, Dunn R, Etherington J. Nerve injuries sustained during warfare: part I–epidemiology. The Journal of Bone and Joint Surgery. British volume. 2012 Apr;94(4):523-8.
- ↑ 6.0 6.1 Dunn JC, Eckhoff MD, Nicholson TC, Campbell W, Kenney K, Smith J, Landau M, Miller M, Souza J, Nesti LJ. Combat-sustained peripheral nerve injuries in the United States Military. The Journal of hand surgery. 2021 Feb 1;46(2):148-e1.
- ↑ Birch R, Misra P, Stewart MP, Eardley WG, Ramasamy A, Brown K, Shenoy R, Anand P, Clasper J, Dunn R, Etherington J. Nerve injuries sustained during warfare: part II: Outcomes. The Journal of Bone and Joint Surgery. British volume. 2012 Apr;94(4):529-35.
- ↑ Eckhoff MD, Craft MR, Nicholson TC, Nesti LJ, Dunn JC. Lower extremity combat sustained peripheral nerve injury in US military personnel. Plastic and Reconstructive Surgery Global Open. 2021 Mar;9(3).
- ↑ 9.0 9.1 9.2 9.3 Reza Salman Roghani and Seyed Mansoor Rayegani (2012). Basics of Peripheral Nerve Injury Rehabilitation, Basic Principles of Peripheral Nerve Disorders, Dr. Seyed Mansoor Rayegani (Ed.), ISBN: 978-953-51-0407-0, InTech, Available from: http://www.intechopen.com/books/basic-principles-of-peripheral-nervedisorders/basics-of-peripheral-nerve-injury-rehabilitation (Last Accessed 24 April 2022)
- ↑ Hubbard J, editor. The peripheral nervous system. Springer Science & Business Media; 2012 Dec 6.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 Simionescu L, Elkwood AL, and Kaufman MR. Traumatic Peripheral Neuropathies. Mar 2022 [Accessed 24 April 2022]. Available from; https://www.uptodate.com/contents/traumatic-peripheral-neuropathies#H5465753
- ↑ Sunderland S. The Anatomy and Physiology of Nerve Injury. Muscle Nerve 1990; 13:771.
- ↑ 13.0 13.1 Burnett MG, Zager EL. Pathophysiology of Peripheral Nerve Injury: A Brief Review. Neurosurgical focus. 2004 May;16(5):1-7.
- ↑ Lee SK, Wolfe SW. Peripheral Nerve Injury and Repair. Journal of the American Academy of Orthopaedic Surgeons. 2000 Jul 1;8(4):243-52.
- ↑ Cruz AJ, De Jesus O. Neurotmesis. InStatPearls [Internet] 2021 Feb 7. StatPearls Publishing.
- ↑ 16.0 16.1 Menorca RM, Fussell TS, Elfar JC. Peripheral Nerve Trauma: Mechanisms of Injury and Recovery. Hand Clinics. 2013 Aug;29(3):317.
- ↑ AMBOSS. Peripheral Nerve Injuries. Available from https://www.amboss.com/us/knowledge/Peripheral_nerve_injuries/ [Access on 24 April 2022