Rehabilitation of Acquired Brain Injury in Disasters and Conflicts
Original Editors - Add your name/s here if you are the original editor/s of this page. User Name
Top Contributors - Naomi O'Reilly, Wendy Walker, Kim Jackson, Tarina van der Stockt and Jess Bell
Introduction[edit | edit source]
While accurate data is scarce, traumatic brain injury remains a common neurological consequence of disasters, natural and man made. A wide range of mild, moderate, and severe traumatic brain injury occur secondary to overpressure, penetrating wounds, and crush injuries following the huge kinetic energy released by rapid-onset natural disasters. Disaster preparedness planners and emergency medical personnel face a major challenge in preventing and managing neurotrauma within this context. As with any traumatic brian injury, management is complex and individuals often have long-term physical, cognitive and behavioural impairments with residual neurological deficits, medical complications all resulting in lifestyle consequences, which necessitate comprehensive interdisciplinary management, including medical, surgical and rehabilitation. [1] Key recommendations from a rehabilitation perspective for traumatic brain injury survivors in disaster and conflict settings included patient/carer education, general physiotherapy, practice in daily living activities and safe equipment use, direct cognitive/behavioural feedback, basic compensatory memory/visual strategies, basic swallowing/communication, and psychological input. More advanced interventions are generally not applicable following disasters due to limited access to services, trained staff/resources, equipment, funding, and operational issues.
Immediate Emergency Care[edit | edit source]
Early diagnosis and treatment of traumatic brain injuries can be challenging under normal circumstances, but are further exacerbated in the aftermath of disaster due to to the chaotic environment including damaged infrastructure, poor communication and shortages of relevant health and rehabilitation workers, particularly neurotrauma specialists. [2]
During this early stage, immediate diagnosis and treatment remains key to minimise the development of secondary brain injuries, which is a massive challenge, particularly in developing countries where medical infrastructure and availability of state-of-the-art neurological care is already scare and may be further limited as a result of the disaster. Families are often separated, and symptoms of posttraumatic stress disorder can be common during the postacute phase.
As a result, early deployment of specialised emergency medical teams to meet the immediate needs of disaster victims is a key element of the immediate emergency response, and is guided by a range of World Health Organization initiatives, including Emergency Response Frameworks (Standards and Guidelines); Coordination Mechanisms, Emergency Medical Team Accreditation Process ensuring that rehabilitation professionals form part of the Emergency Medical Teams. [2][3]Specialised care teams are defined by the World Health Organization as “national or international teams embedded into Emergency Medical Teams or a national facility to provide specialist care”, which may include rehabilitation teams and are deployed based on the response to meet specific needs required at the request of the host health authorities. These teams should be multidisciplinary and need to be integrated into a disaster response and management plan and their skills need to be shared with local rehabilitation and health-care providers through mentoring and educating/training." [1]A specialised care team that is focused on traumatic brain injury rehabilitation in a disaster setting should include; [1][3]
| Rehabilitation Interventions | General Applicability of Recommendations in Disaster Settings | |
|---|---|---|
| Weak | ||
| Team Composition | Minimum Technical Standard;
A traumatic brian injury specialised rehabilitation team should be led by a rehabilitation physician and comprise of at least three other professionals from different disciplines, including rehabilitation medicine, nursing, physiotherapy, occupational therapy, speech and language therapy, and psychology. In addition, a team lead is required to represent the care team at health coordination level | |
| Qualification and Experience | Minimum Technical Standard;
Rehabilitation professionals in a traumatic brian injury specialised care team should have at least 6 months’ experience working in a traumatic brain injury unit or with traumatic brain injury patients in a major trauma center and at least 3 years of postqualifying clinical experience At least one team member, preferable the team leader, should have experience in emergency response and all team members should have undergone training in working in austere environments | |
| Rehabilitation Equipment | Minimum Technical Standard;
Specialized care teams for rehabilitation should have capability to rapidly provide the equipment here. | |
| Length of Stay | Minimum Technical Standard;
A team that embeds into a local facility should plan to stay for at least 1 month with evidence of a exit strategy and release mechanism. | |
Rehabilitation[edit | edit source]
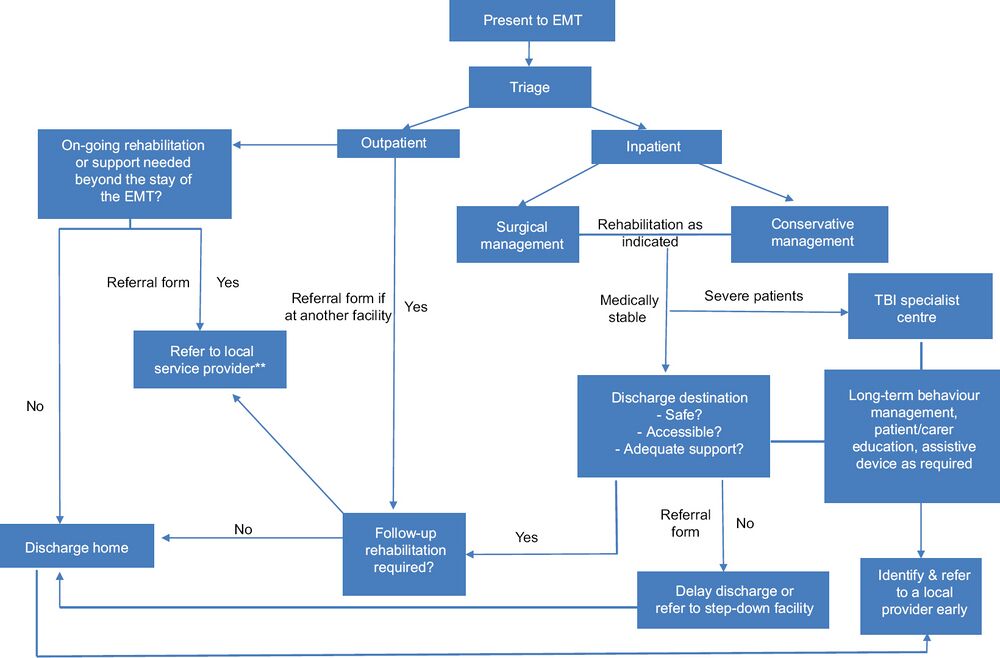
The overriding objective of traumatic brain injury care in disaster settings has now extended well beyond survival and acute management to successful implementation of rehabilitation structures to work towards reintegration of the individual with a traumatic brain injury back into home and community. The World Health Organization minimum standards for rehabilitation recommendations for managing patients with traumatic brain injury following a disasters include; [1][4]
- Cognitive and neurological changes should be monitored and regularly assessed
- Early referral to a step-down facility using local rehabilitation providers and support networks, as required
- Appropriate mobility aids prescribed for long-term mobility deficits using local service provider
- Patients with long term or permanent nerve injury considered for orthotic device, sought from a local provider
- Referral pathways identified for microsurgery for appropriate patients
Rehabilitation is a vital element of the treatment and management process post traumatic brain injury in a disaster setting and should prepare individuals with long-term impairment, their care providers and local rehabilitation personnel to manage their ongoing needs over a longer term and should be started early following any disaster.[4] Rehabilitation should focus on comprehensive assessment for neurological and functional limitations and individualised treatment program for specific functional goals with ongoing monitoring of outcomes. The goal of rehabilitation in a disaster setting is to improve functional outcomes, minimise secondary complications, and successful reintegration into the community, with an emphasis on patient and care giver education and self-management. Survivors of traumatic brain injury need support for acquisition of essential skills for maximum return to their previous level of functional independence, regardless of whether specific impairments can be eliminated. [1]
Heading 3 [edit | edit source]
Add your content to this page here!
Resources[edit | edit source]
References [edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Amatya B, Vasudevan V, Zhang N, Chopra S, Astrakhantseva I, Khan F. Minimum technical standards and recommendations for traumatic brain injury rehabilitation teams in sudden-onset disasters. The Journal of the International Society of Physical and Rehabilitation Medicine. [serial online] 2018 [cited 2019 Oct 19];1:72-94. Available from: http://www.jisprm.org/text.asp?2018/1/2/72/249854
- ↑ 2.0 2.1 Regens JL, Mould N. Prevention and treatment of traumatic brain injury due to rapid-onset natural disasters. Frontiers in public health. 2014 Apr 14;2:28.
- ↑ 3.0 3.1 Vasudevan V, Amatya B, Chopra S, Zhang N, Astrakhantseva I, Khan F. Minimum technical standards and recommendations for traumatic brain injury specialist rehabilitation teams in sudden-onset disasters (for Disaster Rehabilitation Committee special session). Annals of Physical and Rehabilitation Medicine. 2018 Jul 1;61:e120.
- ↑ 4.0 4.1 Lee SY, Amatya B, Judson R, Truesdale M, Reinhardt JD, Uddin T, Xiong XH, Khan F. Applicability of traumatic brain injury rehabilitation interventions in natural disaster settings. Brain injury. 2019 Aug 24;33(10):1293-8. DOI: 10.1080/02699052.2019.1641748