Rehabilitation Governance: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "Category:ReLAB Content Development Project" to "Category:ReLAB-HS Course Page") |
||
| (43 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' - Add your name/s here if you are the original editor/s of this page. [[User:Vidya Acharya|Vidya Acharya]] | '''Original Editors ''' - Add your name/s here if you are the original editor/s of this page. [[User:Vidya Acharya|Vidya Acharya]] and [http://relabhs.org/ ReLAB-HS] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div | </div> | ||
== Introduction == | == Introduction == | ||
Governance of health systems comprises the actions adopted by society to organize itself to promote the health of its population. Good governance results in the effective delivery of health services and improves health outcomes. As health services and service providers are often disorganised in various poor setting resources, it hampers their access. This results in the provision of poor quality services, inefficient use of resources, duplication of services, and decreased service-user satisfaction.<ref name=":4">McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, Geiser P, Duttine A, Mji G, McAuliffe E, Sprunt B. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Globalization and Health. 2016 Dec;12(1):1-8.</ref> | |||
Governance of health systems comprises the actions adopted by society to organize itself to promote the health of its population. Good governance results in the effective delivery of health services and improves health outcomes. As health services and service providers often disorganised in various poor setting resources, it hampers their access. This results in the provision of poor quality services, inefficient use of resources, duplication of services, and decreased service-user satisfaction.<ref name=":4">McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, Geiser P, Duttine A, Mji G, McAuliffe E, Sprunt B. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Globalization and Health. 2016 Dec;12(1):1-8.</ref> | |||
In recent years, governance has transitioned to the fore of the international development agenda, shifting from micro-level, project-specific objectives to macro-level issues of policy-making.<ref name=":4" /> There is a need for the policymakers in less-resourced settings to know how to most adequately strengthen the performance of health systems. | In recent years, governance has transitioned to the fore of the international development agenda, shifting from micro-level, project-specific objectives to macro-level issues of policy-making.<ref name=":4" /> There is a need for the policymakers in less-resourced settings to know how to most adequately strengthen the performance of health systems. | ||
The complexities of leadership and governance can be addressed through a participative, transparent, well-defined, and structured framework. To promote good governance and leadership of health systems, coherent and flexible policies | The complexities of leadership and governance can be addressed through a participative, transparent, well-defined, and structured framework. To promote good governance and leadership of health systems, coherent and flexible policies incorporating health-related human rights and opportunities together are essential. | ||
=== Leadership and Governance === | === Leadership and Governance === | ||
The leadership and governance of health systems <ref name=":5">EVERYBODY’S BUSINESS Strengthening Health systems to improve Health Outcomes WHO’s Frame Work for Action</ref>, also called stewardship, are the most complex and critical building block of any health system. It is about the role of the government in health and its relation to other actors whose activities impact health. It involves overseeing and guiding the whole health system, private as well as public, to protect the public interest. This needs both political and technical action with increased attention to corruption and calls for a more human rights based approach to health. <ref name=":5" /> | The leadership and governance of health systems<ref name=":5">EVERYBODY’S BUSINESS Strengthening Health systems to improve Health Outcomes WHO’s Frame Work for Action</ref>, also called stewardship, are the most complex and critical building block of any health system. It is about the role of the government in health and its relation to other actors whose activities impact health. It involves overseeing and guiding the whole health system, private as well as public, to protect the public interest. This needs both political and technical action with increased attention to corruption and calls for a more human rights-based approach to health. <ref name=":5" /> | ||
All governments are faced with the challenge of defining their role in health concerning other actors. Any approach to leadership and governance must be contingent on national circumstances. WHO helps governments as follows: <ref name=":5" /> | All governments are faced with the challenge of defining their role in health concerning other actors. Any approach to leadership and governance must be contingent on national circumstances. WHO helps governments as follows: <ref name=":5" /> | ||
* Develop health sector policies and frameworks | * Develop health sector policies and frameworks | ||
* Regulatory framework: | * Regulatory framework: design, implement and monitor health-related laws, regulations, and standards; regulation of medical products, [[vaccines]], and technologies; regulation concerning [[Introduction to Occupational Health|occupational health]] and workplace safety | ||
* Accountability on monitoring health system performance as discussed earlier in the building blocks. | * Accountability on monitoring health system performance as discussed earlier in the building blocks. | ||
* Generate and interpret intelligence and research on policy options | * Generate and interpret intelligence and research on policy options | ||
* Build coalitions across government ministries, with the private sector and with communities: to act on key determinants of health; to protect workers’ health; to ensure the health needs of the most vulnerable are properly addressed; to anticipate and address the health impact of public and commercial investments. | * Build coalitions across government ministries, with the private sector and with communities: to act on key determinants of health; to protect workers’ health; to ensure the health needs of the most vulnerable are properly addressed; to anticipate and address the health impact of public and commercial investments. | ||
* Work with external partners to promote greater harmonization and alignment with national health policies. | * Work with external partners to promote greater harmonization and alignment with national health policies. | ||
<br> | |||
Package of Rehabilitation Interventions (PRI) is developed to support ministries of health in planning, budgeting and integrating rehabilitation interventions into health systems.<ref>Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Archives of physical medicine and rehabilitation. 2019 Nov 1;100(11):2205-11.</ref> | Package of Rehabilitation Interventions (PRI) is developed to support ministries of health in planning, budgeting and integrating rehabilitation interventions into health systems.<ref>Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Archives of physical medicine and rehabilitation. 2019 Nov 1;100(11):2205-11.</ref> | ||
== Governance Framework == | == Governance Framework == | ||
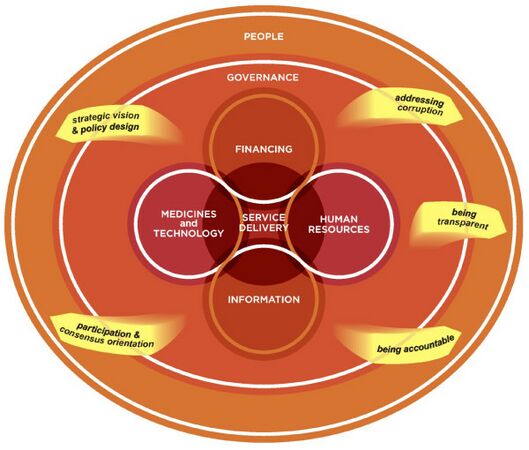
According to the WHO (2007) model of the Health system, the governance framework is based on major independent building blocks that overlap each other.<ref name=":6">Mikkelsen-Lopez I, Wyss K, de Savigny D. An approach to addressing governance from a health system framework perspective. BMC international health and human rights. 2011 Dec;11(1):1-1.</ref> | According to the WHO (2007) model of the Health system, the governance framework is based on major independent building blocks that overlap each other.<ref name=":6">Mikkelsen-Lopez I, Wyss K, de Savigny D. An approach to addressing governance from a health system framework perspective. BMC international health and human rights. 2011 Dec;11(1):1-1.</ref> | ||
# Service delivery acts as the output or is perceived as the quality of the Health System, | # ''Service delivery'' acts as the ''output'' or is perceived as the quality of the Health System, | ||
# Human Resources, Medical Technologies, Information/Data collection, and Financing form the health system inputs, | # ''Human Resources, Medical Technologies, Information/Data collection, and Financing'' form the ''health system inputs'', | ||
# And People, as the governance includes overseeing the entire health system, it permeates with all other building blocks and is driven by People and Actors in the system. | # And People, as the ''governance includes overseeing the entire health system'', it permeates with all other building blocks and is driven by ''People and Actors in the system''. | ||
Strategic vision & policy design and participation & consensus orientation can be viewed more conventionally as governance inputs; these are all interlinked within the governance building block and are dynamic and interchangeable. <ref name=":6" /> | <gallery mode="packed-overlay" widths="300" heights="200" caption="Health systems Building blocks "> | ||
File:Health system Building Blocks.jpg | |||
</gallery><br>'''Strategic vision''' '''& policy design''' and '''participation & consensus''' orientation can be viewed more conventionally as ''governance inputs''; these are all interlinked within the governance building block and are dynamic and interchangeable. <ref name=":6" /><gallery widths="300" heights="300" mode="packed"> | |||
File:Assessing governance across the Health System.jpg | |||
</gallery> | |||
* Strategic vision using transparent information by the stewards are important factors for good health system governance. | * Strategic vision using transparent information by the stewards are important factors for good health system governance. | ||
* A well-designed system should increase integration | * A well-designed system should increase integration, reduce fragmentation & duplication, and encourage the participation of all relevant stakeholders, both state and non-state (such as citizen groups, pharmaceutical companies, insurance firms) in designing policies. Literature suggests a need for meaningful participation of the person with disabilities in the policymaking process. The participation can be strengthened by supporting access to research, statistical information, training for people with disabilities. Governance in health can be assessed by estimating the Determinants of Governance which measures whether the procedure or regulation or policy or law exists. Governance Performance Indicator assesses implementation of rules or policies and it is done by surveys such as Public Expenditure Tracking Surveys, Exit Interviews. | ||
* Consensus should be sought when the voices of numerous stakeholders | * Consensus should be sought when the voices of numerous stakeholders differ and are not homogeneous. | ||
Addressing corruption, being transparent, and being accountable are governance processes.<ref name=":6" /> | <br>'''Addressing corruption, being transparent, and being accountable''' are ''governance processes''.<ref name=":6" /> | ||
* To ensure that the systems' rules are followed, a good health system governance should involve accountability. It includes holding public officials/service providers answerable for processes and outcomes, and imposing sanctions if the specified outcome is not delivered. | * To ensure that the systems' rules are followed, a good health system governance should involve accountability. It includes holding public officials/service providers answerable for processes and outcomes, and imposing sanctions if the specified outcome is not delivered. | ||
* Clear goals should be based on the participation of relevant stakeholders especially from disadvantaged groups or those with less power in order to influence policies, design transparent policies, and promote accountability thereby reducing the risk of corruption. | * Clear goals should be based on the participation of relevant stakeholders especially from disadvantaged groups or those with less power in order to influence policies, design transparent policies, and promote accountability, thereby reducing the risk of corruption. | ||
=== Political Priority === | === Political Priority === | ||
To increase demand for rehabilitation, rehabilitation must become a political priority. Initiatives are more likely to attract political support if they share certain features in each category: the power of actors, the influence of ideas, the nature of political contexts, and characteristics of the issue itself. These form the foundation of our framework on the determinants of political priority for global initiatives.Representatives of different rehabilitation stakeholder groups need to come together and discuss their contributions in making rehabilitation a political party. Global political priority depends on: <ref name=":7">World Health Organisation. Rehabilitation 2030 Meeting Report 8 - 9 July 2019. Available from: https://www.who.int/docs/default-source/documents/health-topics/rehabilitation/2nd-rehab2030-meeting/rehab2030-2ndmeeting-report.pdf?sfvrsn=bc6402fb_5 (accessed 2 Feb 2021). | To increase demand for rehabilitation, rehabilitation must become a political priority. Initiatives are more likely to attract political support if they share certain features in each category: the power of actors, the influence of ideas, the nature of political contexts, and characteristics of the issue itself. These form the foundation of our framework on the determinants of political priority for global initiatives. Representatives of different rehabilitation stakeholder groups need to come together and discuss their contributions in making rehabilitation a political party. Global political priority depends on: <ref name=":7">World Health Organisation. Rehabilitation 2030 Meeting Report 8 - 9 July 2019. Available from: [https://www.who.int/rehabilitation/Meeting-report-Rehab2030-251119-web.pdf https://www.who.int/docs/default-source/documents/health-topics/rehabilitation/2nd-rehab2030-meeting/rehab2030-2ndmeeting-report.pdf?sfvrsn=bc6402fb_5] (accessed 2 Feb 2021). | ||
</ref> | </ref> | ||
==== Actor Power ==== | ==== Actor Power ==== | ||
Policy communities are the network of individuals or | Policy communities are the network of individuals or organisations that operate at global levels and are linked by central concern for issues.<ref name=":8">Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. The lancet. 2007 Oct 13;370(9595):1370-9.</ref> For example, prominent NGO leaders, government officials, UN Agency members. Policy communities help to bring the attention of political leaders in order to solve problems. The emergence of respected leaders embraced by the community facilitates coalescence and gives direction to the initiative. It is important to have strong guiding institutions - organisations or coordinating mechanisms with a mandate to lead the initiative. Initiatives are more likely to gather political support if they are linked to the grassroots organisation in civil society to push global attention to issues rather than remain confined to select members of global policy.<ref name=":8" /> Strong stakeholder cohesion and leadership within rehabilitation are critical. It involves different professions and sub-specialties, and as a result, rehabilitation governance is considerably disintegrated. To strengthen the rehabilitation sector as a whole, it is important to embrace our diversity, create a culture of cohesion and create a common rehabilitation identity.<ref name=":7" /> | ||
==== Ideas ==== | ==== Ideas ==== | ||
Ideas shape political support for initiatives. It is the way in which actors understand and portray the issue and depends on the degree to which the policy community agrees on the definition of, causes of, and solutions to the problem and the public portrayals of the issue in ways that resonate with external audiences, especially the political leaders who control resources.<ref name=":8" /> Ideas | Ideas shape political support for initiatives. It is the way in which actors understand and portray the issue and depends on the degree to which the policy community agrees on the definition of, causes of, and solutions to the problem and the public portrayals of the issue in ways that resonate with external audiences, especially the political leaders who control resources.<ref name=":8" /> Ideas-rehabilitation requires a cohesive unified narrative, both within the rehabilitation community and with external partners. Despite the profession, setting, or sub-specialty, all rehabilitation stakeholders have a common goal – to optimize functioning. | ||
==== Political Contexts ==== | ==== Political Contexts ==== | ||
Political context is the | Political context is the environment in which actors operate. Political moments are when global conditions align favorably for an issue, presenting opportunities for advocates to influence decision-makers. The global rehabilitation community needs to seek political windows, identifying enablers in the system of which advantage can be taken. Rehabilitation is already an integral part of Universal Health Coverage and thus the broader Sustainable Development Goal 3, and is key to ensuring healthy lives and well-being for all at all ages. Rehabilitation is therefore well-positioned within the broader health and development agenda, and this political window needs to be leveraged. <ref name=":7" /><ref name=":8" /> | ||
==== Topic Characteristics ==== | ==== Topic Characteristics ==== | ||
It refers to the features of rehabilitation, and its relevance in the global health context. To raise awareness and advocate for the importance of rehabilitation, the rehabilitation field as a whole requires a strong evidence base. This involves relevant and credible rehabilitation indicators, data on functioning, integration of rehabilitation in the broader health information system, evidence on effective rehabilitation interventions, and a strong economic case for investment.<ref name=":7" /> | It refers to the features of rehabilitation, and its relevance is in the global health context. To raise awareness and advocate for the importance of rehabilitation, the rehabilitation field as a whole requires a strong evidence base. This involves relevant and credible rehabilitation indicators, data on functioning, integration of rehabilitation in the broader health information system, evidence on effective rehabilitation interventions, and a strong economic case for investment.<ref name=":7" /> | ||
== Current Health Priorities == | == Current Health Priorities == | ||
The Health 2020 policy is based on four priority areas for policy action:<ref>Health 2020: a European policy framework supporting action across government and society for health and well-being. Copenhagen: World Health Organization Regional Officie for Europe. 2012 Sep</ref> | The Health 2020 policy is based on four priority areas for policy action:<ref>Health 2020: a European policy framework supporting action across government and society for health and well-being. Copenhagen: World Health Organization Regional Officie for Europe. 2012 Sep</ref> | ||
* investing in health through a life-course approach and empowering people; | * investing in health through a life-course approach and empowering people; | ||
* tackling the | * tackling the region’s major health challenges of [[Non-Communicable Diseases|non-communicable]] and [[Communicable Diseases|communicable diseases]]; | ||
* strengthening people-centered health systems, public health capacity and emergency preparedness, surveillance and response; and | * strengthening people-centered health systems, public health capacity and emergency preparedness, surveillance and response; and | ||
* creating resilient communities and supportive environments. | * creating resilient communities and supportive environments. | ||
Health 2020 recognizes that successful governments can achieve real improvements in health if they work across government to fulfill two linked strategic objectives: | <br>Health 2020 recognizes that successful governments can achieve real improvements in health if they work across government to fulfill two linked strategic objectives: | ||
# improving health for all and reducing health inequalities, | # improving health for all and reducing health inequalities, | ||
# improving leadership and participatory governance for health <ref name=":5" /> | # improving leadership and participatory governance for health <ref name=":5" /> | ||
However the global rehabilitation needs continue to be unmet due to multiple factors, including:<ref name=":2" /> | <br>However, the global rehabilitation needs continue to be unmet due to multiple factors, including:<ref name=":2">World Health Organisation. Rehabilitation. Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (accessed on 12 Jan 2021)</ref> | ||
* Lack of prioritization, funding, policies and plans for rehabilitation at a national level | * Lack of prioritization, funding, policies and plans for rehabilitation at a national level | ||
* Lack of available rehabilitation services outside urban areas | * Lack of available rehabilitation services outside urban areas and long waiting times | ||
* High out-of-pocket expenses and non-existent or inadequate means of funding | * High out-of-pocket expenses and non-existent or inadequate means of funding | ||
* Lack of trained rehabilitation professionals, with less than 10 skilled practitioners per 1 million population in many low- and middle-income settings | * Lack of trained rehabilitation professionals, with less than 10 skilled practitioners per 1 million population in many low- and middle-income settings | ||
* Lack of resources, including assistive technology, equipment and consumables | * Lack of resources, including assistive technology, equipment, and consumables | ||
* | * Need for more research and data on rehabilitation | ||
* Ineffective and under-utilized referral pathways to rehabilitation | * Ineffective and under-utilized referral pathways to rehabilitation | ||
There is an increasing need for rehabilitation worldwide; more than half of people living in some low and middle-income countries | <br>There is an increasing need for rehabilitation worldwide; more than half of people living in some low and middle-income countries require rehabilitation services do not have access to it. The [[COVID-19]] [[Endemics, Epidemics and Pandemics|pandemic]] has led to a new increase in rehabilitation needs as well as causing severe disruption to existing rehabilitation services in 60-70% of countries worldwide.<ref name=":2" /> | ||
== Rehabilitation Policies and Plans == | == Rehabilitation Policies and Plans == | ||
=== | === United Nations Convention on the Rights of Persons with Disabilities === | ||
The [[Convention on the Rights of Persons with Disabilities|United National Convention on the Rights of Persons with Disability]] (UNCRPD) is an international document aimed at protecting the human rights and dignity of persons with a disability. The convention is written under the paradigm that people with a disability are not passive recipients of medical treatment and charity, but autonomous individuals with the right to actively participate in society.<ref name=":The convention in brief">[https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities/the-convention-in-brief.html United Nations, Division for Social Policy and Development Disability. The convention in brief]. Accessed May 8, 2018: </ref> The treaty differs from other international texts related to disability rights in that, if ratified, its provisions are legally binding. | |||
Adopted in 2006, the purpose of the UNCRPD is to promote, protect and ensure full and equal enjoyment of all human rights and fundamental freedoms by all persons with disabilities, and promote respect for their inherent dignity. Eight guiding principles underlie the Convention; <ref name=":1">United Nations. Convention on the Rights of Persons with Disabilities (CRPD): Guiding Principles of the Convention. United Nations DEPARTMENT OF ECONOMIC AND SOCIAL AFFAIRS. https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities/guiding-principles-of-the-convention.html | |||
=== Rehabilitation 2030 | </ref><ref>11. #Envision2030: 17 goals to transform the world for persons with disabilities. United Nations DEPARTMENT OF ECONOMIC AND SOCIAL AFFAIRS. <nowiki>https://www.un.org/development/desa/disabilities/envision2030.html</nowiki>.</ref> | ||
Rehabilitation 2030 <ref>World Health Organisation. Rehabilitation 2030 Initiative. Available from: https://www.who.int/initiatives/rehabilitation-2030 (accessed 2 Feb 2021).</ref> is a call for action to scale up rehabilitation so that countries can be prepared to address the evolving needs of populations up to 2030 was launched in February 2017.<ref>World Health Organisation. Rehabilitation 2030 A Call for Action Meeting Report Feb 6 - 7 2017. Available from: https://www.who.int/disabilities/care/Rehab2030MeetingReport2.pdf?ua=1 (accessed 2 Feb 2021).</ref> The initiative draws attention to the profound unmet need for rehabilitation worldwide and highlights the importance of strengthening health systems to provide rehabilitation. According to WHO’s definition, rehabilitation is one of the quality health services that should be included in Universal Health Coverage so all individuals would be able to access quality rehabilitation services without fear of financial hardship. It focuses on coordinated action from all stakeholders to improve rehabilitation leadership, political support, and investment; integrate rehabilitation within health systems and emergency preparedness; expand high-quality rehabilitation workforces and services; build stronger partnerships, and improve rehabilitation data collection and research capacity. Since the initial call, WHO has supported approximately 20 countries to strengthen health systems to better | |||
# Respect for inherent dignity, individual autonomy, including the freedom to make one’s own choices, and independence of persons; | |||
# Non-discrimination; | |||
# Full and effective participation and inclusion in society; | |||
# Respect for difference and acceptance of persons with disabilities as part of human diversity and humanity; | |||
# Equality of opportunity; | |||
# Accessibility; | |||
# Equality between men and women; | |||
# Respect for the evolving capacities of children with disabilities and respect for the right of children with disabilities to preserve their identities. | |||
<br>Article 25 of the UNCRPD reinforces the right of persons with disabilities to attain the highest standard of health care without discrimination, which includes general healthcare as well as specialized services such as rehabilitation.<ref name=":1" /> | |||
Article 26 deals with habilitation and rehabilitation. It stipulates that governments shall take steps to enable people with a disability to attain and maintain maximum independence and full inclusion and participation in all aspects of life. To accomplish this, it mandates that States shall: <ref name=":1" /> | |||
# Organize, strengthen, and extend comprehensive habilitation and rehabilitation services. | |||
# Promote the development of initial and continuing education for rehabilitation professionals and staff. | |||
# Promote the availability, knowledge, and use of [[Assistive Devices|assistive devices]] and technology for people with a disability. | |||
Read more about the United Nations Convention on the Rights of Persons with Disabilities [[Convention on the Rights of Persons with Disabilities|here]] or access the original text [http://www.un.org/disabilities/documents/convention/convention_accessible_pdf.pdf here]. | |||
=== WHO Global Disability Action Plan 2014-2021 === | |||
The [https://www.who.int/publications/i/item/who-global-disability-action-plan-2014-2021 WHO Global Disability Action Plan 2014-2021] is a significant step towards achieving health and well-being and human rights for people with disabilities. The action plan was endorsed by WHO Member States in 2014 and calls for them to remove barriers and improve access to health services and programs; strengthen and extend rehabilitation, assistive devices and support services, and community-based rehabilitation; and enhance collection of relevant and internationally comparable data on disability, and research on disability and related services. Achieving the objectives of the action plan better enables people with disabilities to fulfil their aspirations in all aspects of life. | |||
=== Sustainable Development Goals === | |||
The 17 Sustainable Development Goals (SDGs), also known as the Global Goals, are part of the ''2030 Agenda for Sustainable Development.''<ref name=":0">United Nations. ''The Sustainable Development Agenda''. 2017 [cited 2017 07.12.]; Available from: <nowiki>http://www.un.org/sustainabledevelopment/development-agenda/</nowiki>.</ref> Ongoing from its implementation in 2015, the goals universally aim to “mobilize efforts to end all forms of poverty, fight inequalities and tackle climate change, while ensuring that no one is left behind”.<ref name=":0" /> | |||
The concept of sustainability was first defined in the ''Brundtland Commission’s'' report ''Our common future'' in 1987. It presented a new concept of development, a “Global Agenda for Change”, which should “ensure that it meets the needs of the present without compromising the ability of future generations to meet their own needs”.<ref>World Commision on Environmnet and Development, ''Our Common Future''. 1987.</ref> It became a very successful approach, internationally influencing economic, social, and environmental issues.<ref>United Nations Economic Commission for Europe. ''Sustainable Development - concept and action''. 2017 [cited 2017 07.12.]; Available from: <nowiki>http://www.unece.org/oes/nutshell/2004-2005/focus_sustainable_development.html</nowiki>. .</ref> The latest outcome is the ''2030 Agenda for Sustainable Development'', which was developed after ''the Rio+20 Conference'' in 2012 and adopted by world leaders at a UN summit in September 2015 (New York).<ref name=":0" /><ref>United Nations. ''United Nations Sustainable Development Summit 2015''. 2017 [cited 2017 07.12.]; Available from: <nowiki>https://sustainabledevelopment.un.org/post2015/summit</nowiki>.</ref> The ''Millennium Development Goals'' were a predecessor of the SDGs.<ref>United Nations. ''Sustainable Development.'' 2017 [cited 2017 07.12.]; Available from: <nowiki>https://sustainabledevelopment.un.org/resourcelibrary</nowiki>.</ref> However, the SDG go further than the ''Millennium Development Goals'' did before, and target not only low-income countries but all countries.<ref name=":0" />[[File:E_2018_SDG_Poster_without_UN_emblem_Letter_US.png|center|1000x1000px|frameless|Figure.1 Sustainable Development Goals]] | |||
== Rehabilitation 2030 == | |||
Rehabilitation 2030 <ref>World Health Organisation. Rehabilitation 2030 Initiative. Available from: https://www.who.int/initiatives/rehabilitation-2030 (accessed 2 Feb 2021).</ref> is a call for action to scale up rehabilitation so that countries can be prepared to address the evolving needs of populations up to 2030 was launched in February 2017.<ref>World Health Organisation. Rehabilitation 2030 A Call for Action Meeting Report Feb 6 - 7 2017. Available from: https://www.who.int/disabilities/care/Rehab2030MeetingReport2.pdf?ua=1 (accessed 2 Feb 2021).</ref> The initiative draws attention to the profound unmet need for rehabilitation worldwide and highlights the importance of strengthening health systems to provide rehabilitation. According to WHO’s definition, rehabilitation is one of the quality health services that should be included in Universal Health Coverage so all individuals would be able to access quality rehabilitation services without fear of financial hardship. It focuses on coordinated action from all stakeholders to improve rehabilitation leadership, political support, and investment; integrate rehabilitation within health systems and emergency preparedness; expand high-quality rehabilitation workforces and services; build stronger partnerships, and improve rehabilitation data collection and research capacity. Since the initial call, WHO has supported approximately 20 countries to strengthen health systems to provide better rehabilitation services. Following are the recommendation for strengthening in Rehabilitation in Health Systems: <ref>World Health Organisation. Rehabilitation in Health Systems Booklet. Available from:https://www.who.int/disabilities/brochure_EN_2.pdf?ua=1 (accessed 2 Jan 2021).</ref> | |||
==== To integrate Rehabilitation into the Health System: ==== | |||
* Effectively integration of rehabilitation needs clear designation and strong governance. In most situations, the ministry of health will be the most appropriate agency for governing rehabilitation, with strong links to other relevant sectors, such as social welfare, education, and labor. | * Effectively integration of rehabilitation needs clear designation and strong governance. In most situations, the ministry of health will be the most appropriate agency for governing rehabilitation, with strong links to other relevant sectors, such as social welfare, education, and labor. | ||
==== To integrate rehabilitation services into and between primary, secondary, and tertiary levels of health systems ==== | ==== To integrate rehabilitation services into and between primary, secondary, and tertiary levels of health systems ==== | ||
* For the identification of needs and an effective continuum of care throughout a person’s recovery, rehabilitation is required at all levels. Standardized referral pathways and other coordination mechanisms between levels help | * For the identification of needs and an effective continuum of care throughout a person’s recovery, rehabilitation is required at all levels. Standardized referral pathways and other coordination mechanisms between levels help ensure a good transition of care for optimal outcomes. | ||
==== To ensure hospitals include | ==== To ensure hospitals include specialized rehabilitation units for inpatients with complex needs ==== | ||
* Specialized rehabilitation wards can provide intensive, highly | * Specialized rehabilitation wards can provide intensive, highly specialized interventions for restoring functioning to patients with complex rehabilitation needs - in cases with lower-limb amputation, spinal cord injury, stroke, and in the care of older people. The establishment or extension of specialized rehabilitation units should be based on the context of the health system, specifically the availability of rehabilitation workforce and funding. | ||
==== To ensure both community and hospital rehabilitation services are available ==== | ==== To ensure both community and hospital rehabilitation services are available ==== | ||
| Line 116: | Line 128: | ||
==== To ensure the availability of a multi-disciplinary rehabilitation workforce ==== | ==== To ensure the availability of a multi-disciplinary rehabilitation workforce ==== | ||
* A multi-disciplinary workforce would ensure that the rehabilitation needs within the population can be met. These interventions are effective in the management of many chronic, complex, or severe conditions that may significantly impact multiple domains of functioning (vision, communication, mobility, and cognition). As rehabilitation disciplines need distinct skills, a | * A multi-disciplinary workforce would ensure that the rehabilitation needs within the population can be met. These interventions are effective in the management of many chronic, complex, or severe conditions that may significantly impact multiple domains of functioning (vision, communication, mobility, and cognition). As rehabilitation disciplines need distinct skills, a multi-disciplinary workforce can significantly improve the quality of care and improve health outcomes. Long-term investment in the education, development, and retention of a multi-disciplinary rehabilitation workforce should thus be factored in health sector planning and budgets. | ||
==== To ensure financial resources are allocated to rehabilitation services ==== | ==== To ensure financial resources are allocated to rehabilitation services ==== | ||
* The service delivery gets significantly influenced by the way health systems allocate financial resources so there is a need to allocate specific budgets for rehabilitation services. Allocation of resources for rehabilitation can increase both the availability and the quality of rehabilitation services and minimize out-of-pocket expenses, which is a significant barrier to service utilization. | * The service delivery gets significantly influenced by the way health systems allocate financial resources, so there is a need to allocate specific budgets for rehabilitation services. Allocation of resources for rehabilitation can increase both the availability and the quality of rehabilitation services and minimize out-of-pocket expenses, which is a significant barrier to service utilization. | ||
==== To ensure rehabilitation services to be covered under health insurance ==== | ==== To ensure rehabilitation services to be covered under health insurance ==== | ||
* Access to rehabilitation services increases | * Access to rehabilitation services increases when health insurance includes rehabilitation. Because health insurance protects only a minority of the population in many parts of the world, this mechanism of financial protection should be part of broader initiatives to improve the affordability of rehabilitation services. | ||
==== To implement financing and procurement policies that ensure assistive products are available to everyone who needs them ==== | ==== To implement financing and procurement policies that ensure assistive products are available to everyone who needs them ==== | ||
* Assistive products, such as mobility devices, hearing aids, and white canes | * Assistive products, such as mobility devices, hearing aids, and white canes play an important role in improving functioning and increasing independence and participation. | ||
* A study shows that there are many barriers to both accessing and providing amputee rehabilitation services in the Western Area, Sierra Leone, and recommends a revised effort by the government to implement progressive policies on disability which will aid the improvement of amputee rehabilitation services. Increased funding and local training programs are needed to improve service delivery.<ref>Allen AP, Bolton WS, Jalloh MB, Halpin SJ, Jayne DG, Scott JD. Barriers to accessing and providing rehabilitation after a lower limb amputation in Sierra Leone–a multidisciplinary patient and service provider perspective. Disability and Rehabilitation. 2020 Nov 11:1-8.</ref> | |||
=== Second Global Rehabilitation 2030 === | |||
Two years after the launch of Rehabilitation 2030, the Second Global Rehabilitation 2030, held in July 2019, at WHO headquarters in Geneva to take stock of progress and collectively plan the next steps to continue advancing the global rehabilitation agenda.<ref name=":7" /> Over 260 rehabilitation stakeholders from 65 countries, including the Member States, United Nations agencies, civil society, professional organizations, academia, rehabilitation experts, and user groups, attended the event and shared personal stories and functioning data. The meeting emphasized: <ref name=":7" /> | |||
* the importance of ‘functioning’ as WHO’s third health indicator alongside mortality and morbidity, highlighting the central role that rehabilitation plays in optimizing functioning. | |||
* the need for strengthening health systems in general and primary health care, in particular, to reach all people in need. Efforts should be directed towards strengthening the health system as a whole. | |||
* the need for integrating rehabilitation into universal health coverage for rehabilitation to reach its full potential as it recognized universal health coverage as the vehicle for making sure that everyone who needs rehabilitation gets quality services to optimize and maintain their functioning in everyday life. | |||
* advancing health financing mechanisms and packages of care, health workforce capacity, and health information systems in countries | |||
* accelerating action at country level by Key WHO resources | |||
* the launch of the Rehabilitation in health systems: guide for action – a tool supporting countries to identify priorities and develop a strategic plan to increase quality, accessible and effective rehabilitation services. It has a four-phase process: assessment of the situation, developing rehabilitation and strategic plan, establishing rehabilitation monitoring and review process, and implementation of rehabilitation plan. | |||
== AT 2030 == | |||
The World Health Organization defines '''assistive technology''' as ‘the application of organized knowledge and skills related to assistive products, including systems and services.’ '''Assistive products''' are ‘any external product (including devices, equipment, instruments or software)…the primary purpose of which is to maintain or improve an individual’s functioning and independence, and thereby promote their well-being’.<ref>World Health Organisation. Priority Assistive Products List Available from: https://apps.who.int/iris/bitstream/handle/10665/207694/WHO_EMP_PHI_2016.01_eng.pdf?sequence=1 (accessed 30/06/2021)</ref> Put simply, assistive products are the products and assistive technology is the whole ecosystem that is needed for their safe and effective provision and use. It is estimated that by 2050, two billion people would benefit from assistive technology, yet 90% will not have access. A lack assistive technology access results in children rejected from education, adults excluded from work and family life, and older people prohibited from participating in their communities. | |||
The [https://www.at2030.org/ AT2030] programme for low cost, mass market, life-changing Assistive Technology for all, was launched in July 2018 at the Global Disability Summit in London and is part of a £20 million programme funded by the Foreign, Commonwealth & Development Office. Through partner collaborations with GDI HUB, the World Health Organisation Clinton Health Access Initiative, Leonard Cheshire and other key organisations such as Disabled People’s Organisations, AT 2030 hopes to transform access to life-changing assistive technology such as wheelchairs, prosthetics, hearing aids, glasses and digital assistive devices by creating partnerships with the private sector to build and shape markets testing innovative approaches and backing ‘what works' to get AT to those who need it the most. | |||
On March 28, 2019, The Minister of State for International Development, Lord Bates, announced that UK AID, from the British Government was doubling its investment in the flagship AT 2030 programme from £10 million to £19.8 million. This will be 100% matched by the private sector, country governments, academic institutions, NGOs and other partners. | |||
Over five years, AT2030 will test ‘what works’ to improve access to AT and will invest in and support solutions to scale with a focus on innovative products, new service models, and global capacity support. The programme will reach 9 million directly and 6 million more people indirectly to enable a lifetime of potential through life-changing Assistive Technology. AT2030 will work on this by developing partnerships which break down and overcome the traditional barriers to assistive technology access. By bringing partners who traditionally don’t work together, including people who haven’t worked before in the assistive technology space, we know there will be difficult conversations. However, these interactions have already started to pay dividends with new thinking and approaches being tested in over ten countries. | |||
In order to meet such goals the AT2030 programme seeks to: | |||
* Accelerate access to assistive technology by tackling supply and demand-side drivers to scaling assistive technology markets | |||
* Coordinate evidence to understand the value, impact and economics of assistive technology | |||
* Improve access to emerging technology with a focus on establishing an Innovation ecosystem | |||
* Test market shaping methodologies | |||
* Provide a set of global benchmarks and standards for assistive technology through the creation of an integrated service provision model which aim to open up market access | |||
* Build capacity for existing community-led activities by undertaking action research within informal settlements | |||
* | |||
* | |||
* | |||
* | |||
== Conclusion == | == Conclusion == | ||
To increase rehabilitation services globally, rehabilitation community must focus on: <ref name=":7" /> | To increase rehabilitation services globally, the rehabilitation community must focus on: <ref name=":7" /> consistent collection of information on functioning so that health policies can be planned. Researchers, journal editors and experts from WHO Collaborating Centres need to promote data collection on functioning and move towards research in health systems. | ||
Political commitment and investment in rehabilitation and assistive technology and rehabilitation stakeholders play a role in advancing the rehabilitation agenda. The responsibility is now on Member States and key rehabilitation stakeholders to ensure that rehabilitation and access to assistive technology is firmly positioned within the main health agenda and becomes a priority in their respective countries and regions. The Rehabilitation 2030 and AT 2030 agenda has paved the way for this process. | |||
Strengthening of health systems and integrating rehabilitation at all service levels including access to assistive technology is critical, particularly at the primary care level. Rehabilitation professionals need to strengthen their collaboration and join efforts for rehabilitation as a unified professional field. Organizations delivering services and organizations of specific medical specialties need to promote health system strengthening for rehabilitation. | |||
== Resources == | |||
Rehabilitation | === World Health Organisation === | ||
* [https://www.who.int/rehabilitation/rehab-2030-call-for-action/en/ Rehabilitation 2030] | |||
*[https://apps.who.int/iris/bitstream/handle/10665/325607/9789241515986-eng.pdf Rehabilitation in Health Systems Guide for Action] | |||
=== Rehab 2030 === | === Rehab 2030 === | ||
=== | * https://www.who.int/initiatives/rehabilitation-2030 | ||
=== AT 2030 === | |||
* https://www.at2030.org/ | |||
* https://atscale2030.org/ | |||
=== Relevant Articles === | |||
* Negrini S. [https://pubmed.ncbi.nlm.nih.gov/28488425/ The possibilities and challenges of "Rehabilitation 2030: a call for action" by the World Health Organization: a unique opportunity not to be missed]. European Journal of Physical and Rehabilitation Medicine. 2017;53(2):169-72. | |||
* Cieza A. [https://isaac-online.org/wp-content/uploads/a_RehabilitationTheHealthStrategyOfThe21stCentury.pdf Rehabilitation the health strategy of the 21st century, really?]. Archives of physical medicine and rehabilitation. 2019 Nov 1;100(11):2212-4. | |||
* Heinemann AW, Feuerstein M, Frontera WR, Gard SA, Kaminsky LA, Negrini S, Richards LG, Vallée C. [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-4962-8 Rehabilitation is a global health priority.] | |||
* McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, Geiser P, Duttine A, Mji G, McAuliffe E, Sprunt B. [https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-016-0182-8 Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis.] Globalization and Health. 2016 Dec 1;12(1):49. | |||
*[https://journals.sagepub.com/doi/pdf/10.1177/026921550201600102 Implementation of Clinical Governance in Rehabilitation Medicine] | |||
* Gilson L, Agyepong IA. [https://watermark.silverchair.com/czy052.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAArAwggKsBgkqhkiG9w0BBwagggKdMIICmQIBADCCApIGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMuzyZ82WeGROaVtq4AgEQgIICY_oVJp4mvt9SQ8IVLJ1WAZmvczF2_aJosgaKJBNFzbAVndE6 Strengthening health system leadership for better governance: what does it take?]. | |||
* Bamford‐Wade AN, Moss C. [https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1365-2834.2010.01134.x Transformational leadership and shared governance: an action study. Journal of nursing management.] 2010 Oct;18(7):815-21. | |||
* Kirigia JM, Kirigia DG. [https://link.springer.com/article/10.1186/1755-7682-4-11 The essence of governance in health development.] International Archives of Medicine. 2011 Dec 1;4(1):11. | |||
== References == | == References == | ||
| Line 173: | Line 202: | ||
[[Category:Understanding Rehabilitation Content Development Project]] | [[Category:Understanding Rehabilitation Content Development Project]] | ||
[[Category:Rehabilitation]] | [[Category:Rehabilitation]] | ||
[[Category: | [[Category:Course Pages]] | ||
[[Category:ReLAB-HS Course Page]] | |||
Latest revision as of 10:45, 1 June 2022
Original Editors - Add your name/s here if you are the original editor/s of this page. Vidya Acharya and ReLAB-HS
Top Contributors - Naomi O'Reilly, Vidya Acharya, Kim Jackson, Admin, Lucinda hampton, Oyemi Sillo and Ashmita Patrao
Introduction[edit | edit source]
Governance of health systems comprises the actions adopted by society to organize itself to promote the health of its population. Good governance results in the effective delivery of health services and improves health outcomes. As health services and service providers are often disorganised in various poor setting resources, it hampers their access. This results in the provision of poor quality services, inefficient use of resources, duplication of services, and decreased service-user satisfaction.[1]
In recent years, governance has transitioned to the fore of the international development agenda, shifting from micro-level, project-specific objectives to macro-level issues of policy-making.[1] There is a need for the policymakers in less-resourced settings to know how to most adequately strengthen the performance of health systems.
The complexities of leadership and governance can be addressed through a participative, transparent, well-defined, and structured framework. To promote good governance and leadership of health systems, coherent and flexible policies incorporating health-related human rights and opportunities together are essential.
Leadership and Governance[edit | edit source]
The leadership and governance of health systems[2], also called stewardship, are the most complex and critical building block of any health system. It is about the role of the government in health and its relation to other actors whose activities impact health. It involves overseeing and guiding the whole health system, private as well as public, to protect the public interest. This needs both political and technical action with increased attention to corruption and calls for a more human rights-based approach to health. [2]
All governments are faced with the challenge of defining their role in health concerning other actors. Any approach to leadership and governance must be contingent on national circumstances. WHO helps governments as follows: [2]
- Develop health sector policies and frameworks
- Regulatory framework: design, implement and monitor health-related laws, regulations, and standards; regulation of medical products, vaccines, and technologies; regulation concerning occupational health and workplace safety
- Accountability on monitoring health system performance as discussed earlier in the building blocks.
- Generate and interpret intelligence and research on policy options
- Build coalitions across government ministries, with the private sector and with communities: to act on key determinants of health; to protect workers’ health; to ensure the health needs of the most vulnerable are properly addressed; to anticipate and address the health impact of public and commercial investments.
- Work with external partners to promote greater harmonization and alignment with national health policies.
Package of Rehabilitation Interventions (PRI) is developed to support ministries of health in planning, budgeting and integrating rehabilitation interventions into health systems.[3]
Governance Framework[edit | edit source]
According to the WHO (2007) model of the Health system, the governance framework is based on major independent building blocks that overlap each other.[4]
- Service delivery acts as the output or is perceived as the quality of the Health System,
- Human Resources, Medical Technologies, Information/Data collection, and Financing form the health system inputs,
- And People, as the governance includes overseeing the entire health system, it permeates with all other building blocks and is driven by People and Actors in the system.
Strategic vision & policy design and participation & consensus orientation can be viewed more conventionally as governance inputs; these are all interlinked within the governance building block and are dynamic and interchangeable. [4]
- Strategic vision using transparent information by the stewards are important factors for good health system governance.
- A well-designed system should increase integration, reduce fragmentation & duplication, and encourage the participation of all relevant stakeholders, both state and non-state (such as citizen groups, pharmaceutical companies, insurance firms) in designing policies. Literature suggests a need for meaningful participation of the person with disabilities in the policymaking process. The participation can be strengthened by supporting access to research, statistical information, training for people with disabilities. Governance in health can be assessed by estimating the Determinants of Governance which measures whether the procedure or regulation or policy or law exists. Governance Performance Indicator assesses implementation of rules or policies and it is done by surveys such as Public Expenditure Tracking Surveys, Exit Interviews.
- Consensus should be sought when the voices of numerous stakeholders differ and are not homogeneous.
Addressing corruption, being transparent, and being accountable are governance processes.[4]
- To ensure that the systems' rules are followed, a good health system governance should involve accountability. It includes holding public officials/service providers answerable for processes and outcomes, and imposing sanctions if the specified outcome is not delivered.
- Clear goals should be based on the participation of relevant stakeholders especially from disadvantaged groups or those with less power in order to influence policies, design transparent policies, and promote accountability, thereby reducing the risk of corruption.
Political Priority[edit | edit source]
To increase demand for rehabilitation, rehabilitation must become a political priority. Initiatives are more likely to attract political support if they share certain features in each category: the power of actors, the influence of ideas, the nature of political contexts, and characteristics of the issue itself. These form the foundation of our framework on the determinants of political priority for global initiatives. Representatives of different rehabilitation stakeholder groups need to come together and discuss their contributions in making rehabilitation a political party. Global political priority depends on: [5]
Actor Power[edit | edit source]
Policy communities are the network of individuals or organisations that operate at global levels and are linked by central concern for issues.[6] For example, prominent NGO leaders, government officials, UN Agency members. Policy communities help to bring the attention of political leaders in order to solve problems. The emergence of respected leaders embraced by the community facilitates coalescence and gives direction to the initiative. It is important to have strong guiding institutions - organisations or coordinating mechanisms with a mandate to lead the initiative. Initiatives are more likely to gather political support if they are linked to the grassroots organisation in civil society to push global attention to issues rather than remain confined to select members of global policy.[6] Strong stakeholder cohesion and leadership within rehabilitation are critical. It involves different professions and sub-specialties, and as a result, rehabilitation governance is considerably disintegrated. To strengthen the rehabilitation sector as a whole, it is important to embrace our diversity, create a culture of cohesion and create a common rehabilitation identity.[5]
Ideas[edit | edit source]
Ideas shape political support for initiatives. It is the way in which actors understand and portray the issue and depends on the degree to which the policy community agrees on the definition of, causes of, and solutions to the problem and the public portrayals of the issue in ways that resonate with external audiences, especially the political leaders who control resources.[6] Ideas-rehabilitation requires a cohesive unified narrative, both within the rehabilitation community and with external partners. Despite the profession, setting, or sub-specialty, all rehabilitation stakeholders have a common goal – to optimize functioning.
Political Contexts[edit | edit source]
Political context is the environment in which actors operate. Political moments are when global conditions align favorably for an issue, presenting opportunities for advocates to influence decision-makers. The global rehabilitation community needs to seek political windows, identifying enablers in the system of which advantage can be taken. Rehabilitation is already an integral part of Universal Health Coverage and thus the broader Sustainable Development Goal 3, and is key to ensuring healthy lives and well-being for all at all ages. Rehabilitation is therefore well-positioned within the broader health and development agenda, and this political window needs to be leveraged. [5][6]
Topic Characteristics[edit | edit source]
It refers to the features of rehabilitation, and its relevance is in the global health context. To raise awareness and advocate for the importance of rehabilitation, the rehabilitation field as a whole requires a strong evidence base. This involves relevant and credible rehabilitation indicators, data on functioning, integration of rehabilitation in the broader health information system, evidence on effective rehabilitation interventions, and a strong economic case for investment.[5]
Current Health Priorities[edit | edit source]
The Health 2020 policy is based on four priority areas for policy action:[7]
- investing in health through a life-course approach and empowering people;
- tackling the region’s major health challenges of non-communicable and communicable diseases;
- strengthening people-centered health systems, public health capacity and emergency preparedness, surveillance and response; and
- creating resilient communities and supportive environments.
Health 2020 recognizes that successful governments can achieve real improvements in health if they work across government to fulfill two linked strategic objectives:
- improving health for all and reducing health inequalities,
- improving leadership and participatory governance for health [2]
However, the global rehabilitation needs continue to be unmet due to multiple factors, including:[8]
- Lack of prioritization, funding, policies and plans for rehabilitation at a national level
- Lack of available rehabilitation services outside urban areas and long waiting times
- High out-of-pocket expenses and non-existent or inadequate means of funding
- Lack of trained rehabilitation professionals, with less than 10 skilled practitioners per 1 million population in many low- and middle-income settings
- Lack of resources, including assistive technology, equipment, and consumables
- Need for more research and data on rehabilitation
- Ineffective and under-utilized referral pathways to rehabilitation
There is an increasing need for rehabilitation worldwide; more than half of people living in some low and middle-income countries require rehabilitation services do not have access to it. The COVID-19 pandemic has led to a new increase in rehabilitation needs as well as causing severe disruption to existing rehabilitation services in 60-70% of countries worldwide.[8]
Rehabilitation Policies and Plans[edit | edit source]
United Nations Convention on the Rights of Persons with Disabilities[edit | edit source]
The United National Convention on the Rights of Persons with Disability (UNCRPD) is an international document aimed at protecting the human rights and dignity of persons with a disability. The convention is written under the paradigm that people with a disability are not passive recipients of medical treatment and charity, but autonomous individuals with the right to actively participate in society.[9] The treaty differs from other international texts related to disability rights in that, if ratified, its provisions are legally binding.
Adopted in 2006, the purpose of the UNCRPD is to promote, protect and ensure full and equal enjoyment of all human rights and fundamental freedoms by all persons with disabilities, and promote respect for their inherent dignity. Eight guiding principles underlie the Convention; [10][11]
- Respect for inherent dignity, individual autonomy, including the freedom to make one’s own choices, and independence of persons;
- Non-discrimination;
- Full and effective participation and inclusion in society;
- Respect for difference and acceptance of persons with disabilities as part of human diversity and humanity;
- Equality of opportunity;
- Accessibility;
- Equality between men and women;
- Respect for the evolving capacities of children with disabilities and respect for the right of children with disabilities to preserve their identities.
Article 25 of the UNCRPD reinforces the right of persons with disabilities to attain the highest standard of health care without discrimination, which includes general healthcare as well as specialized services such as rehabilitation.[10]
Article 26 deals with habilitation and rehabilitation. It stipulates that governments shall take steps to enable people with a disability to attain and maintain maximum independence and full inclusion and participation in all aspects of life. To accomplish this, it mandates that States shall: [10]
- Organize, strengthen, and extend comprehensive habilitation and rehabilitation services.
- Promote the development of initial and continuing education for rehabilitation professionals and staff.
- Promote the availability, knowledge, and use of assistive devices and technology for people with a disability.
Read more about the United Nations Convention on the Rights of Persons with Disabilities here or access the original text here.
WHO Global Disability Action Plan 2014-2021[edit | edit source]
The WHO Global Disability Action Plan 2014-2021 is a significant step towards achieving health and well-being and human rights for people with disabilities. The action plan was endorsed by WHO Member States in 2014 and calls for them to remove barriers and improve access to health services and programs; strengthen and extend rehabilitation, assistive devices and support services, and community-based rehabilitation; and enhance collection of relevant and internationally comparable data on disability, and research on disability and related services. Achieving the objectives of the action plan better enables people with disabilities to fulfil their aspirations in all aspects of life.
Sustainable Development Goals[edit | edit source]
The 17 Sustainable Development Goals (SDGs), also known as the Global Goals, are part of the 2030 Agenda for Sustainable Development.[12] Ongoing from its implementation in 2015, the goals universally aim to “mobilize efforts to end all forms of poverty, fight inequalities and tackle climate change, while ensuring that no one is left behind”.[12]
The concept of sustainability was first defined in the Brundtland Commission’s report Our common future in 1987. It presented a new concept of development, a “Global Agenda for Change”, which should “ensure that it meets the needs of the present without compromising the ability of future generations to meet their own needs”.[13] It became a very successful approach, internationally influencing economic, social, and environmental issues.[14] The latest outcome is the 2030 Agenda for Sustainable Development, which was developed after the Rio+20 Conference in 2012 and adopted by world leaders at a UN summit in September 2015 (New York).[12][15] The Millennium Development Goals were a predecessor of the SDGs.[16] However, the SDG go further than the Millennium Development Goals did before, and target not only low-income countries but all countries.[12]
Rehabilitation 2030[edit | edit source]
Rehabilitation 2030 [17] is a call for action to scale up rehabilitation so that countries can be prepared to address the evolving needs of populations up to 2030 was launched in February 2017.[18] The initiative draws attention to the profound unmet need for rehabilitation worldwide and highlights the importance of strengthening health systems to provide rehabilitation. According to WHO’s definition, rehabilitation is one of the quality health services that should be included in Universal Health Coverage so all individuals would be able to access quality rehabilitation services without fear of financial hardship. It focuses on coordinated action from all stakeholders to improve rehabilitation leadership, political support, and investment; integrate rehabilitation within health systems and emergency preparedness; expand high-quality rehabilitation workforces and services; build stronger partnerships, and improve rehabilitation data collection and research capacity. Since the initial call, WHO has supported approximately 20 countries to strengthen health systems to provide better rehabilitation services. Following are the recommendation for strengthening in Rehabilitation in Health Systems: [19]
To integrate Rehabilitation into the Health System:[edit | edit source]
- Effectively integration of rehabilitation needs clear designation and strong governance. In most situations, the ministry of health will be the most appropriate agency for governing rehabilitation, with strong links to other relevant sectors, such as social welfare, education, and labor.
To integrate rehabilitation services into and between primary, secondary, and tertiary levels of health systems[edit | edit source]
- For the identification of needs and an effective continuum of care throughout a person’s recovery, rehabilitation is required at all levels. Standardized referral pathways and other coordination mechanisms between levels help ensure a good transition of care for optimal outcomes.
To ensure hospitals include specialized rehabilitation units for inpatients with complex needs[edit | edit source]
- Specialized rehabilitation wards can provide intensive, highly specialized interventions for restoring functioning to patients with complex rehabilitation needs - in cases with lower-limb amputation, spinal cord injury, stroke, and in the care of older people. The establishment or extension of specialized rehabilitation units should be based on the context of the health system, specifically the availability of rehabilitation workforce and funding.
To ensure both community and hospital rehabilitation services are available[edit | edit source]
- Rehabilitation in both hospital and community settings is necessary to ensure timely intervention and access to services. Rehabilitation in hospital settings enables early intervention speeding the recovery, optimizing the outcomes, and facilitating smooth, timely discharge. Many people require rehabilitation well beyond discharge from the hospital, while other users may require services solely in the community. People with developmental, sensory, or cognitive impairment may benefit from long-term interventions that are often best delivered at home, school, or in the workplace
To ensure the availability of a multi-disciplinary rehabilitation workforce[edit | edit source]
- A multi-disciplinary workforce would ensure that the rehabilitation needs within the population can be met. These interventions are effective in the management of many chronic, complex, or severe conditions that may significantly impact multiple domains of functioning (vision, communication, mobility, and cognition). As rehabilitation disciplines need distinct skills, a multi-disciplinary workforce can significantly improve the quality of care and improve health outcomes. Long-term investment in the education, development, and retention of a multi-disciplinary rehabilitation workforce should thus be factored in health sector planning and budgets.
To ensure financial resources are allocated to rehabilitation services[edit | edit source]
- The service delivery gets significantly influenced by the way health systems allocate financial resources, so there is a need to allocate specific budgets for rehabilitation services. Allocation of resources for rehabilitation can increase both the availability and the quality of rehabilitation services and minimize out-of-pocket expenses, which is a significant barrier to service utilization.
To ensure rehabilitation services to be covered under health insurance[edit | edit source]
- Access to rehabilitation services increases when health insurance includes rehabilitation. Because health insurance protects only a minority of the population in many parts of the world, this mechanism of financial protection should be part of broader initiatives to improve the affordability of rehabilitation services.
To implement financing and procurement policies that ensure assistive products are available to everyone who needs them[edit | edit source]
- Assistive products, such as mobility devices, hearing aids, and white canes play an important role in improving functioning and increasing independence and participation.
- A study shows that there are many barriers to both accessing and providing amputee rehabilitation services in the Western Area, Sierra Leone, and recommends a revised effort by the government to implement progressive policies on disability which will aid the improvement of amputee rehabilitation services. Increased funding and local training programs are needed to improve service delivery.[20]
Second Global Rehabilitation 2030[edit | edit source]
Two years after the launch of Rehabilitation 2030, the Second Global Rehabilitation 2030, held in July 2019, at WHO headquarters in Geneva to take stock of progress and collectively plan the next steps to continue advancing the global rehabilitation agenda.[5] Over 260 rehabilitation stakeholders from 65 countries, including the Member States, United Nations agencies, civil society, professional organizations, academia, rehabilitation experts, and user groups, attended the event and shared personal stories and functioning data. The meeting emphasized: [5]
- the importance of ‘functioning’ as WHO’s third health indicator alongside mortality and morbidity, highlighting the central role that rehabilitation plays in optimizing functioning.
- the need for strengthening health systems in general and primary health care, in particular, to reach all people in need. Efforts should be directed towards strengthening the health system as a whole.
- the need for integrating rehabilitation into universal health coverage for rehabilitation to reach its full potential as it recognized universal health coverage as the vehicle for making sure that everyone who needs rehabilitation gets quality services to optimize and maintain their functioning in everyday life.
- advancing health financing mechanisms and packages of care, health workforce capacity, and health information systems in countries
- accelerating action at country level by Key WHO resources
- the launch of the Rehabilitation in health systems: guide for action – a tool supporting countries to identify priorities and develop a strategic plan to increase quality, accessible and effective rehabilitation services. It has a four-phase process: assessment of the situation, developing rehabilitation and strategic plan, establishing rehabilitation monitoring and review process, and implementation of rehabilitation plan.
AT 2030[edit | edit source]
The World Health Organization defines assistive technology as ‘the application of organized knowledge and skills related to assistive products, including systems and services.’ Assistive products are ‘any external product (including devices, equipment, instruments or software)…the primary purpose of which is to maintain or improve an individual’s functioning and independence, and thereby promote their well-being’.[21] Put simply, assistive products are the products and assistive technology is the whole ecosystem that is needed for their safe and effective provision and use. It is estimated that by 2050, two billion people would benefit from assistive technology, yet 90% will not have access. A lack assistive technology access results in children rejected from education, adults excluded from work and family life, and older people prohibited from participating in their communities.
The AT2030 programme for low cost, mass market, life-changing Assistive Technology for all, was launched in July 2018 at the Global Disability Summit in London and is part of a £20 million programme funded by the Foreign, Commonwealth & Development Office. Through partner collaborations with GDI HUB, the World Health Organisation Clinton Health Access Initiative, Leonard Cheshire and other key organisations such as Disabled People’s Organisations, AT 2030 hopes to transform access to life-changing assistive technology such as wheelchairs, prosthetics, hearing aids, glasses and digital assistive devices by creating partnerships with the private sector to build and shape markets testing innovative approaches and backing ‘what works' to get AT to those who need it the most.
On March 28, 2019, The Minister of State for International Development, Lord Bates, announced that UK AID, from the British Government was doubling its investment in the flagship AT 2030 programme from £10 million to £19.8 million. This will be 100% matched by the private sector, country governments, academic institutions, NGOs and other partners.
Over five years, AT2030 will test ‘what works’ to improve access to AT and will invest in and support solutions to scale with a focus on innovative products, new service models, and global capacity support. The programme will reach 9 million directly and 6 million more people indirectly to enable a lifetime of potential through life-changing Assistive Technology. AT2030 will work on this by developing partnerships which break down and overcome the traditional barriers to assistive technology access. By bringing partners who traditionally don’t work together, including people who haven’t worked before in the assistive technology space, we know there will be difficult conversations. However, these interactions have already started to pay dividends with new thinking and approaches being tested in over ten countries.
In order to meet such goals the AT2030 programme seeks to:
- Accelerate access to assistive technology by tackling supply and demand-side drivers to scaling assistive technology markets
- Coordinate evidence to understand the value, impact and economics of assistive technology
- Improve access to emerging technology with a focus on establishing an Innovation ecosystem
- Test market shaping methodologies
- Provide a set of global benchmarks and standards for assistive technology through the creation of an integrated service provision model which aim to open up market access
- Build capacity for existing community-led activities by undertaking action research within informal settlements
Conclusion[edit | edit source]
To increase rehabilitation services globally, the rehabilitation community must focus on: [5] consistent collection of information on functioning so that health policies can be planned. Researchers, journal editors and experts from WHO Collaborating Centres need to promote data collection on functioning and move towards research in health systems.
Political commitment and investment in rehabilitation and assistive technology and rehabilitation stakeholders play a role in advancing the rehabilitation agenda. The responsibility is now on Member States and key rehabilitation stakeholders to ensure that rehabilitation and access to assistive technology is firmly positioned within the main health agenda and becomes a priority in their respective countries and regions. The Rehabilitation 2030 and AT 2030 agenda has paved the way for this process.
Strengthening of health systems and integrating rehabilitation at all service levels including access to assistive technology is critical, particularly at the primary care level. Rehabilitation professionals need to strengthen their collaboration and join efforts for rehabilitation as a unified professional field. Organizations delivering services and organizations of specific medical specialties need to promote health system strengthening for rehabilitation.
Resources[edit | edit source]
World Health Organisation[edit | edit source]
Rehab 2030[edit | edit source]
AT 2030[edit | edit source]
Relevant Articles[edit | edit source]
- Negrini S. The possibilities and challenges of "Rehabilitation 2030: a call for action" by the World Health Organization: a unique opportunity not to be missed. European Journal of Physical and Rehabilitation Medicine. 2017;53(2):169-72.
- Cieza A. Rehabilitation the health strategy of the 21st century, really?. Archives of physical medicine and rehabilitation. 2019 Nov 1;100(11):2212-4.
- Heinemann AW, Feuerstein M, Frontera WR, Gard SA, Kaminsky LA, Negrini S, Richards LG, Vallée C. Rehabilitation is a global health priority.
- McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, Geiser P, Duttine A, Mji G, McAuliffe E, Sprunt B. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Globalization and Health. 2016 Dec 1;12(1):49.
- Implementation of Clinical Governance in Rehabilitation Medicine
- Gilson L, Agyepong IA. Strengthening health system leadership for better governance: what does it take?.
- Bamford‐Wade AN, Moss C. Transformational leadership and shared governance: an action study. Journal of nursing management. 2010 Oct;18(7):815-21.
- Kirigia JM, Kirigia DG. The essence of governance in health development. International Archives of Medicine. 2011 Dec 1;4(1):11.
References[edit | edit source]
- ↑ 1.0 1.1 McVeigh J, MacLachlan M, Gilmore B, McClean C, Eide AH, Mannan H, Geiser P, Duttine A, Mji G, McAuliffe E, Sprunt B. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Globalization and Health. 2016 Dec;12(1):1-8.
- ↑ 2.0 2.1 2.2 2.3 EVERYBODY’S BUSINESS Strengthening Health systems to improve Health Outcomes WHO’s Frame Work for Action
- ↑ Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Archives of physical medicine and rehabilitation. 2019 Nov 1;100(11):2205-11.
- ↑ 4.0 4.1 4.2 Mikkelsen-Lopez I, Wyss K, de Savigny D. An approach to addressing governance from a health system framework perspective. BMC international health and human rights. 2011 Dec;11(1):1-1.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 World Health Organisation. Rehabilitation 2030 Meeting Report 8 - 9 July 2019. Available from: https://www.who.int/docs/default-source/documents/health-topics/rehabilitation/2nd-rehab2030-meeting/rehab2030-2ndmeeting-report.pdf?sfvrsn=bc6402fb_5 (accessed 2 Feb 2021).
- ↑ 6.0 6.1 6.2 6.3 Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. The lancet. 2007 Oct 13;370(9595):1370-9.
- ↑ Health 2020: a European policy framework supporting action across government and society for health and well-being. Copenhagen: World Health Organization Regional Officie for Europe. 2012 Sep
- ↑ 8.0 8.1 World Health Organisation. Rehabilitation. Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (accessed on 12 Jan 2021)
- ↑ United Nations, Division for Social Policy and Development Disability. The convention in brief. Accessed May 8, 2018:
- ↑ 10.0 10.1 10.2 United Nations. Convention on the Rights of Persons with Disabilities (CRPD): Guiding Principles of the Convention. United Nations DEPARTMENT OF ECONOMIC AND SOCIAL AFFAIRS. https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities/guiding-principles-of-the-convention.html
- ↑ 11. #Envision2030: 17 goals to transform the world for persons with disabilities. United Nations DEPARTMENT OF ECONOMIC AND SOCIAL AFFAIRS. https://www.un.org/development/desa/disabilities/envision2030.html.
- ↑ 12.0 12.1 12.2 12.3 United Nations. The Sustainable Development Agenda. 2017 [cited 2017 07.12.]; Available from: http://www.un.org/sustainabledevelopment/development-agenda/.
- ↑ World Commision on Environmnet and Development, Our Common Future. 1987.
- ↑ United Nations Economic Commission for Europe. Sustainable Development - concept and action. 2017 [cited 2017 07.12.]; Available from: http://www.unece.org/oes/nutshell/2004-2005/focus_sustainable_development.html. .
- ↑ United Nations. United Nations Sustainable Development Summit 2015. 2017 [cited 2017 07.12.]; Available from: https://sustainabledevelopment.un.org/post2015/summit.
- ↑ United Nations. Sustainable Development. 2017 [cited 2017 07.12.]; Available from: https://sustainabledevelopment.un.org/resourcelibrary.
- ↑ World Health Organisation. Rehabilitation 2030 Initiative. Available from: https://www.who.int/initiatives/rehabilitation-2030 (accessed 2 Feb 2021).
- ↑ World Health Organisation. Rehabilitation 2030 A Call for Action Meeting Report Feb 6 - 7 2017. Available from: https://www.who.int/disabilities/care/Rehab2030MeetingReport2.pdf?ua=1 (accessed 2 Feb 2021).
- ↑ World Health Organisation. Rehabilitation in Health Systems Booklet. Available from:https://www.who.int/disabilities/brochure_EN_2.pdf?ua=1 (accessed 2 Jan 2021).
- ↑ Allen AP, Bolton WS, Jalloh MB, Halpin SJ, Jayne DG, Scott JD. Barriers to accessing and providing rehabilitation after a lower limb amputation in Sierra Leone–a multidisciplinary patient and service provider perspective. Disability and Rehabilitation. 2020 Nov 11:1-8.
- ↑ World Health Organisation. Priority Assistive Products List Available from: https://apps.who.int/iris/bitstream/handle/10665/207694/WHO_EMP_PHI_2016.01_eng.pdf?sequence=1 (accessed 30/06/2021)