Rehabilitation Contexts
Original Editors - Add your name/s here if you are the original editor/s of this page. User Name and ReLAB-HS
Top Contributors - Naomi O'Reilly, Vidya Acharya, Kim Jackson, Tarina van der Stockt, Lucinda hampton, Oyemi Sillo, Jess Bell and Ashmita Patrao
Introduction[edit | edit source]
One of the most important factors in rehabilitation are the contextual factors, as this goes a long way to help rehabilitation professionals understand and assess the psychological, emotional state and well-being of the individual throughout the course of their rehabilitation. We know that the environment is known to have significant impact on treatment generally, therefore, the circumstances surrounding rehabilitation, from the situation before, during and after the event leading to a oss in function are all important factors to consider throughout the rehabilitation process.[1] The context in which rehabilitation occurs greatly influences the range and availability of rehabilitation services and their utilization.
The World Health Organisation defines social determinants of health as ‘the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life’, which are largely responsible for health inequalities, including inequity. In other words a holistic view of the context in which healthcare is provided, is key to improving health equity, and that the biggest gains in health may not necessarily be achieved by improving healthcare alone but also through strategies to improve these social determinants..
Low Resource Contexts[edit | edit source]
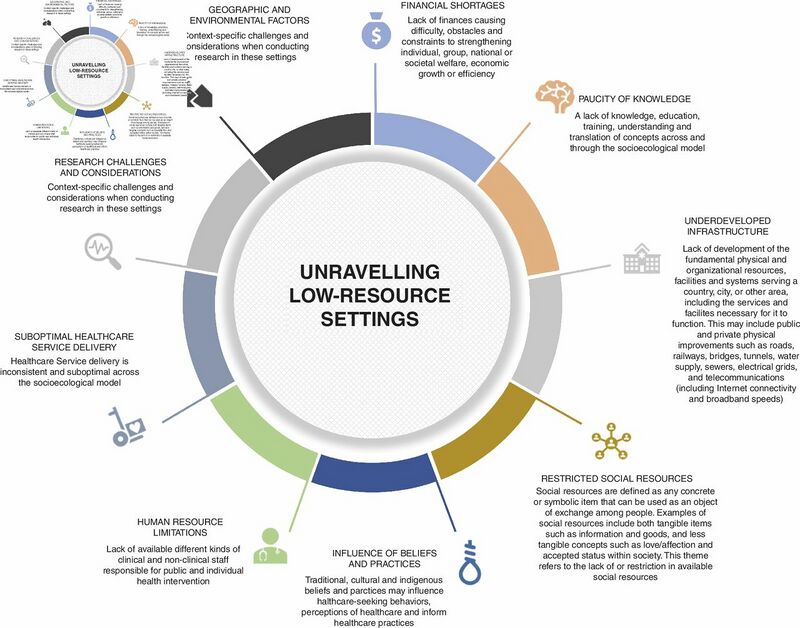
The effects of healthcare-related inequalities are most evident in low-resource settings, which are are often not explicitly defined, and where umbrella terms which are easier to operationalise, such as ‘low-to-middle-income countries’ or ‘developing countries’, are often used. Without a deeper understanding of context, such proxies are pregnant with assumptions, insinuate homogeneity that is unsupported and hamper knowledge translation between settings.
Conflict and Disasters Contexts[edit | edit source]
From the first world war to more recent disasters, such as the 2015 Nepal earthquake, the importance of integrating rehabilitation into emergency responses to conflicts and disasters has been clear. The World Health Organization emergency medical team standards and recommendations for rehabilitation, launched in 2016, signalled significant progress in recognising the role that rehabilitation professionals play and the necessity of early intervention. However, while the emergency medical community takes strides towards integrating early rehabilitation in conflict and disaster response, early rehabilitation remains an emerging area.
Rehabilitation professionals face unique challenges associated with complex trauma, injury surge and resource scarcity that many have never encountered before. Practical guidance to deliver quality early rehabilitation in these contexts is essential if conflict and disaster response is to evolve beyond its life- and limb-saving mandate to deliver care that maximises patient outcomes. Rehabilitation professionals need to be equipped with the knowledge and skills to meet patient needs and navigate the demands of emergency medical response. In humanitarian emergency situations such as during or post-conflict and natural disaster situations, the need for basic functional rehabilitation services is overwhelming and critical to preventing disability and improving the lives of people with disabilities. Early Rehabilitation is now recognised as being an integral part of a patient’s recovery in conflicts and disaster situations. Starting in acute care, early rehabilitation can help prevent complications, speed recovery, and help ensure continuity of care. Rehabilitation professionals working in early rehabilitation need skills across a wide range of clinical areas, and in conflicts and disasters need to be able to manage challenges including large surges in patient numbers, limited equipment, and complex clinical presentations. Due to advances in response, management and post medical care in disaster situations, high mortality rates has gradually transitioned to an increased morbidity rates. Victims of natural disasters now have higher chance of survival, they may however have disabilities which may significantly impact their physical and psychological health and affect their quality of life, patients with pre-existing disabilities and co-morbidities are also at the risk of higher mortality rate.[2][3]
Rehabilitation in natural disaster situations should be of utmost concern due to the vulnerability of the victims, some areas which need interventions in disaster situation include; [1]
- Collaboration and governance
- Capacity building
- Person-centred multidisciplinary care
- Improved communication
- Increased public awareness and active participation/inclusion of disaster survivors/family/community partners
- Strengthen evidence-based information, education and access to information
- Strengthen community-based rehabilitation.
Resources[edit | edit source]
- Early Rehabilitation in Conflict and Disasters Field Handbook
- Rehabilitation in Sudden Onset Disasters
- Responding Internationally to Disasters
- The Role of Physical Therapists in Disaster Management
References [edit | edit source]
- ↑ 1.0 1.1 Khan F, Amatya B, Rathore FA, Galea MP. Medical Rehabilitation in Natural Disaster in the Asia Pacific Region: The Way Forward. International Journal of Natural Disaster Health Security. 2015: 2(2); 6 - 12
- ↑ Rehinhardt JD, Li J, Gosney J, Rathore FA, Haig AJ. Disability and Health-related Intervention in International Disaster Relief. Journal of Global Health Action. 2011. 4:7191
- ↑ Rathore FA, Gosney J, Reinhardt JD, Haig AJ, Li J. Medical Rehabilitation after Natural Disasters: Why, When and How?. Archives of Physical and Medical Rehabilitation. 2012. 93(10);1875 - 81