Pressure Ulcers: Difference between revisions
Jayati Mehta (talk | contribs) No edit summary |
Jayati Mehta (talk | contribs) No edit summary |
||
| Line 184: | Line 184: | ||
== MANAGEMENT == | == MANAGEMENT == | ||
Addressing the many aspects of wound care usually requires a multidisciplinary approach. Members of your care team may include: | Addressing the many aspects of wound care usually requires a multidisciplinary approach. Members of your care team may include:<ref name="same">http://www.mayoclinic.org/diseases-conditions/bedsores/basics/treatment/con-20030848</ref> | ||
*A ''primary care physician'' who oversees the treatment plan | *A ''primary care physician'' who oversees the treatment plan | ||
| Line 197: | Line 197: | ||
#'''Reducing pressure''' | #'''Reducing pressure''' | ||
The first step in treating a bedsore is reducing the pressure that caused it. Strategies include the following: | The first step in treating a bedsore is reducing the pressure that caused it. Strategies include the following:<ref name="same" /> | ||
*<u>Repositioning</u> - In case of a pressure sore, the patient need to be repositioned regularly and placed in correct positions. If using a wheelchair, try shifting weight every 15 minutes or so.If the patient is confined to a bed, change positions every two hours.If the patient has enough upper body strength,he should try repositioning himself using a device such as a trapeze bar. Caregivers can use bed linens to help lift and reposition you. This can reduce friction and shearing. | *<u>Repositioning</u> - In case of a pressure sore, the patient need to be repositioned regularly and placed in correct positions. If using a wheelchair, try shifting weight every 15 minutes or so.If the patient is confined to a bed, change positions every two hours.If the patient has enough upper body strength,he should try repositioning himself using a device such as a trapeze bar. Caregivers can use bed linens to help lift and reposition you. This can reduce friction and shearing. | ||
Revision as of 19:29, 23 December 2016
Original Editor - Jayati Mehta
Lead Editors
DEFINITION[edit | edit source]
The National Pressure Ulcer Advisory Panel,U.S (NPUAP) defines a pressure ulcer as an area of unrelieved pressure over a defined area, usually over a bony prominence, resulting in ischemia, cell death, and tissue necrosis.[1]
The terms decubitus ulcer (from Latin decumbere, “to lie down”), pressure sore, and pressure ulcer often are used interchangeably
PATHOPHYSIOLOGY[edit | edit source]
In 1873, Sir James Paget described the production of pressure ulcers remarkably well, and his description is still quite accurate today.[2]
Many factors contribute to the development of pressure ulcers, but pressure leading to ischemia and necrosis is the final common pathway.
Pressure ulcers result from constant pressure sufficient to impair local blood flow to soft tissue for an extended period. This external pressure must be greater than the arterial capillary pressure (32 mm Hg) to impair inflow and greater than the venous capillary closing pressure (8-12 mm Hg) to impede the return of flow for an extended time[3].Tissues are capable withstanding enormous pressures for brief periods, but prolonged exposure to pressures just slightly above capillary filling pressure initiates a downward spiral toward tissue necrosis and ulceration. The superficial dermis can tolerate ischemia for 2 to 8 hours before breakdown occurs. Deeper muscle, connective, and fat tissues tolerate pressures for 2 hours or less(probably because of its increased need for oxygen and higher metabolic requirements). Thus, there may be significant damage to underlying tissues while the epidermis and dermis remain intact.By the time ulceration is present through the skin level, significant damage of underlying muscle may already have occurred, making the overall shape of the ulcer an inverted cone.
Other factors contributing to pressure ulcers include-[4]
- Friction
Friction is the resistance to motion. It may occur when the skin is dragged across a surface, such as when you change position or a care provider moves you. The friction may be even greater if the skin is moist. Friction may make fragile skin more vulnerable to injury.
- Shear
Shear occurs when two surfaces move in the opposite direction. For example, when a hospital bed is elevated at the head, you can slide down in bed. As the tailbone moves down, the skin over the bone may stay in place — essentially pulling in the opposite direction. This motion may injure tissue and blood vessels, making the site more vulnerable to damage from sustained pressure.
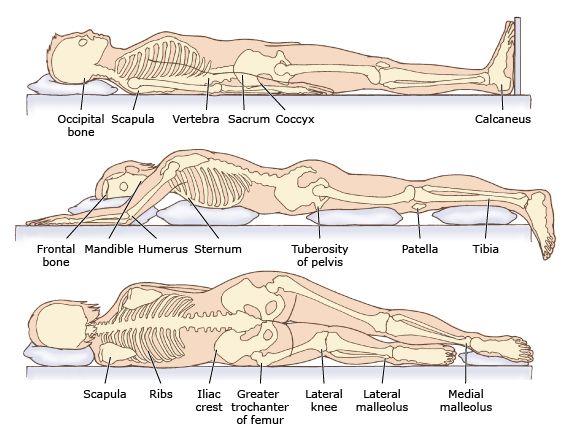
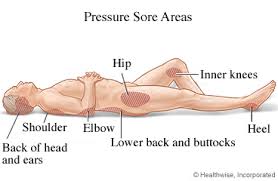
SITES[edit | edit source]
The areas most susceptiblle to pressure in recumbent position include:[5]
- SUPINE :
- Occiput
- Scapulae
- Vertebrae
- Elbows
- Sacrum
- Coccyx
- Heels
- PRONE :
- Ears (head rotated)
- Shoulders (anterior aspect)
- Illiac crest
- Male genital region
- Patella
- Dorsum of feet
- SIDE-LYING -
- Scapulae
- Vertebrae
- Elbows
- Sacrum
- Coccyx
- Heels
- Ears
- Shoulders (lateral aspect)
- Greater trochanter
- Head of fibula
- Knees (medial aspect from contact between knees)
- Lateral malleolus
- Medial malleolus (contact between malleoli)
RISK FACTORS[edit | edit source]
People are at risk of developing pressure sores if they have difficulty moving and are unable to easily change position while seated or in bed. Immobility may be due to:[6]
- Generally poor health or weakness
- Paralysis
- Injury or illness that requires bed rest or wheelchair use
- Recovery after surgery
- Sedation
- Coma
Other factors that increase the risk of pressure sores include:
- Age. The skin of older adults is generally more fragile, thinner, less elastic and drier than the skin of younger adults. Also, older adults usually produce new skin cells more slowly. These factors make skin vulnerable to damage.
- Lack of sensory perception. Spinal cord injuries, neurological disorders and other conditions can result in a loss of sensation. An inability to feel pain or discomfort can result in not being aware of bedsores or the need to change position.
- Weight loss. Weight loss is common during prolonged illnesses, and muscle atrophy and wasting are common in people with paralysis. The loss of fat and muscle results in less cushioning between bones and a bed or a wheelchair.
- Poor nutrition and hydration. People need enough fluids, calories, protein, vitamins and minerals in their daily diet to maintain healthy skin and prevent the breakdown of tissues.
- Excess moisture or dryness. Skin that is moist from sweat or lack of bladder control is more likely to be injured and increases the friction between the skin and clothing or bedding. Very dry skin increases friction as well.
- Bowel incontinence. Bacteria from fecal matter can cause serious local infections and lead to life-threatening infections affecting the whole body.
- Medical conditions affecting blood flow. Health problems that can affect blood flow, such as diabetes and vascular disease, increase the risk of tissue damage.
- Smoking. Smoking reduces blood flow and limits the amount of oxygen in the blood. Smokers tend to develop more-severe wounds, and their wounds heal more slowly.
- Limited alertness. People whose mental awareness is lessened by disease, trauma or medications may be unable to take the actions needed to prevent or care for pressure sores.
- Muscle spasms. People who have frequent muscle spasms or other involuntary muscle movement may be at increased risk of pressure sores from frequent friction and shearing.
PRESSURE SORE GRADING[edit | edit source]
The definitions of the four pressure ulcer stages are revised periodically by the National Pressure Ulcer Advisor Panel (NPUAP) in the United States and the European Pressure Ulcer Advisor Panel (EPUAP) in Europe.
The updated staging system includes the following definitions[7]:
Pressure Injury:
A pressure injury is localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue.
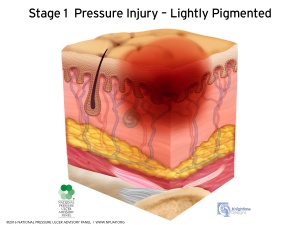
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration; these may indicate deep tissue pressure injury.
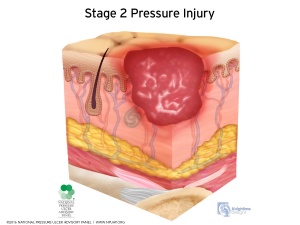
- Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis
Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible and deeper tissues are not visible. Granulation tissue, slough and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture associated skin damage (MASD) including incontinence associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
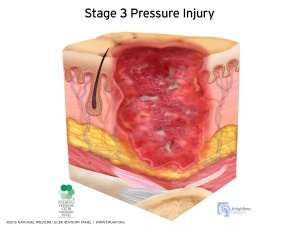
- Stage 3 Pressure Injury: Full-thickness skin loss
Full-thickness loss of skin, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
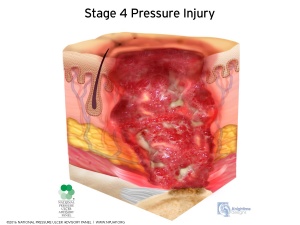
- Stage 4 Pressure Injury: Full-thickness skin and tissue loss
Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole (rolled edges), undermining and/or tunneling often occur. Depth varies by anatomical location. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
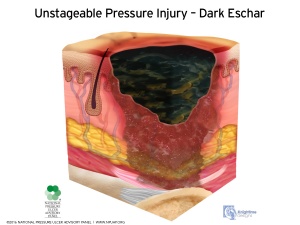
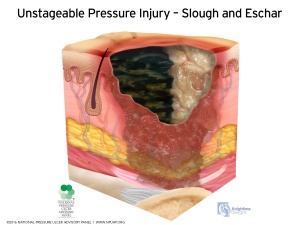
- Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e. dry, adherent, intact without erythema or fluctuance) on the heel or ischemic limb should not be softened or removed.
CLINICAL PRESENTATION[edit | edit source]
The severity of pressure ulceration can be estimated by observing clinical signs. A progression from least tissue damage to most severe damage is presented here.[5]
• The first clinical sign of pressure ulceration is blanchable erythemaalong with increased skin temperature. If pressure is relieved, tissues may recover in 24 hours. If pressure is unrelieved, nonblanchable erythema occurs.
• Progression to a superficial abrasion, blister, or shallow crater indicates involvement of the dermis.
• When full-thickness skin loss is apparent, the ulcer appears as a deep crater. Bleeding is minimal, and tissues are indurated and warm. Eschar formation marks full-thickness skin loss. Tunneling or undermining is often present.
• The majority of all pressure ulcers develop over six primary bony areas sacrum, coccyx, greater trochanter, ischial tuberosity, calcaneus (heel), and lateral malleolus.
DIAGNOSIS[edit | edit source]
HISTORY[edit | edit source]
If an individual has a history of a period of immobility followed by the discovery of a warm, red, spot over a bony prominence, a pressure ulcer can usually be confirmed. If the spot is unnaturally soft to the touch, sometimes referred to as “boggy,” this is enough evidence to suspect that damage is deeper than the epidermis.[5]
TESTS[edit | edit source]
The following tests may be performed :
- Blood tests
- Tissue cultures to diagnose a bacterial or fungal infection in a wound that doesn't heal with treatment or is already at stage IV.
- Tissue cultures to check for cancerous tissue in a chronic, nonhealing wound.[8]
PREVENTION[edit | edit source]
The NPUAP has described the following pressure injury prevention points[9]:
RISK ASSESSMENT
1) Consider bedfast and chairfast individuals to be at risk for development of pressure injury.
2) Use a structured risk assessment, such as the Braden Scale, to identify individuals at risk for pressure injury
as soon as possible (but within 8 hours after admission).
3) Refine the assessment byincluding these additional riskfactors:
- Fragile skin
- Existing pressure injury of anystage, including those ulcers that have healed or are closed
- Impairments in blood flow to the extremities from vascular disease, diabetes or tobacco use
- Pain in areas of the body exposed to pressure
4) Repeat the risk assessment at regular intervals and with anychange in condition. Base the frequency of regular assessments on acuitylevels:
A. Acute care Every shift
B. Long term care. Weeklyfor 4 weeks, then quarterly
C. Home care. At every nurse visit
5) Develop a plan of care based on the areas of risk, rather than on the total risk assessment score. For example, if the risk stems from immobility, address turning, repositioning, and the support surface. If the riskis from malnutrition, address those problems.
SKIN CARE
1 Inspect all of the skin upon admission as soon as possible (but within 8 hours).
2 Inspect the skin at least dailyfor signs of pressure injury, especially nonblanchable erythema.
3 Assess pressure points, such as the sacrum, coccyx, buttocks, heels, ischium, trochanters, elbows and beneath medical devices.
4 When inspecting darkly pigmented skin, lookfor changes in skin tone,skin temperature and tissue consistencycompared to adjacent skin.
Moistening the skin assists in identifying changes in color.
5 Cleanse the skin promptly after episodes of incontinence.
6 Use skin cleansers that are pH balanced for the skin.
7 Use skin moisturizers daily on dry skin.
8 Avoid positioning an individual on an area of erythema or pressure injury.
NUTRITION
1 Consider hospitalized individuals to be at riskfor under nutrition and malnutrition from their illness or being NPO for diagnostic testing.
2 Use a valid and reliable screening tool to determine risk of malnutrition,such as the Mini Nutritional Assessment.
3 Refer all individuals at riskfor pressure injuryfrom malnutrition to a registered dietitian/nutritionist.
4 Assist the individual at mealtimes to increase oral intake.
5 Encourage all individuals at riskfor pressure injuryto consume adequate fluids and a balanced diet.
6 Assess weight changes over time.
7 Assess the adequacy of oral, enteral and parenteral intake.
8 Provide nutritional supplements between meals and with oral medications, unless contraindicated.
REPOSITIONING AND MOBILIZATION
1 Turn and reposition all individuals at risk for pressure injury, unless contraindicated due to medical condition or medical treatments.
2 Choose a frequencyfor turning based on the support surface in use, the tolerance of skin for pressure and the individual’s preferences.
3 Consider lengthening the turning schedule during the night to allow for uninterrupted sleep.
4 Turn the individual into a 30-degree side lying position, and use your hand to determine if the sacrum is off the bed
5 Avoid positioning the individual on body areas with pressure injury.
6 Ensure that the heels are free from the bed.
7 Consider the level of immobility, exposure to shear,skin moisture, perfusion, bodysize and weight of the individual when choosing a support surface.
8 Continue to reposition an individual when placed on any support surface.
9 Use a breathable incontinence pad when using microclimate management surfaces.
10 Use a pressure redistributing chair cushion for individuals sitting in chairs or wheelchairs.
11 Reposition weak or immobile individuals in chairs hourly.
12 If the individual cannot be moved or is positioned with the head of the bed elevated over 30°, place a polyurethane foam dressing on the sacrum.
13 Use heel offloading devices or polyurethane foam dressings on individuals at high-riskfor heel ulcers
14 Place thin foam or breathable dressings under medical devices.
EDUCATION
1 Teach the individual and family about risk for pressure injury
2 Engage individual and family in risk reduction interventions.
MANAGEMENT[edit | edit source]
Addressing the many aspects of wound care usually requires a multidisciplinary approach. Members of your care team may include:[10]
- A primary care physician who oversees the treatment plan
- A physician specializing in wound care
- Nurses or medical assistants who provide both care and education for managing wounds
- A social worker who helps you or your family access appropriate resources and addresses emotional concerns related to long-term recovery
- A physical therapist who helps with improving mobility
- A dietitian who monitors your nutritional needs and recommends an appropriate diet.
The following include the goals and steps of treatment:
- Reducing pressure
The first step in treating a bedsore is reducing the pressure that caused it. Strategies include the following:[10]
- Repositioning - In case of a pressure sore, the patient need to be repositioned regularly and placed in correct positions. If using a wheelchair, try shifting weight every 15 minutes or so.If the patient is confined to a bed, change positions every two hours.If the patient has enough upper body strength,he should try repositioning himself using a device such as a trapeze bar. Caregivers can use bed linens to help lift and reposition you. This can reduce friction and shearing.
- Using support surfaces. - Use a mattress, bed and special cushions that helps lie in an appropriate position, relieve pressure on any sores and protect vulnerable skin. If the patient is in a wheelchair, use a cushion. Styles include foam, air filled and water filled. Select one that suits the condition, body type and mobility.
2. Dressing
It is important that pressure ulcers be kept clean, moist, and covered. This helps reduce the risk of infection and speeds up the healing process.[11]
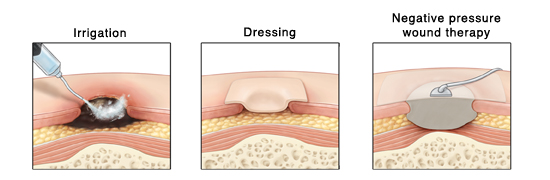
Wound irrigation
An irrigating catheter or syringe and saline may be used to flush the ulcer free of debris. Wound cleansers may also be used to loosen up and clean out debris. The amount of pressure used during irrigation should be enough to clean the wound without damaging it. Follow your facility’s guidelines regarding irrigation.
Types of dressings
Some guidelines for dressing include:[12]
| Condition | Cover dressing |
| None to moderate exudates | Gauze with tape or composite |
| Moderate to heavy exudates | Foam dressing with tape or composite |
| Frequent soiling | Hydrocolloid dressing, film or composite |
| Fragile skin | Stretch gauze or stretch net |
Negative pressure wound therapy
Negative pressure wound therapy (NPWT)—also called vacuum-assisted closure—removes exudate, helps reduce bacterial growth, and promotes blood flow and granulation formation. First, a foam dressing is placed in the wound and the wound is covered with an occlusive dressing. Then tubing is attached to a pump, which creates subatmospheric pressure in the wound
3. Surgical intervention[13]
Debridement - Necrotic tissue should be removed in most pressure ulcers. The heel is an exception in many cases when the limb has an inadequate blood supply. Necrotic tissue is an ideal area for bacterial growth, which has the ability to greatly compromise wound healing. There are five ways to remove necrotic tissue.
- Autolytic debridement is the use of moist dressings to promote autolysis with the body's own enzymes and white blood cells. It is a slow process, but mostly painless, and is most effective in individuals with a properly functioning immune system.
- Biological debridement, or maggot debridement therapy, is the use of medical maggots to feed on necrotic tissue and therefore clean the wound of excess bacteria. Although this fell out of favor for many years, in January 2004, the FDA approved maggots as a live medical device.
- Chemical debridement, or enzymatic debridement, is the use of prescribed enzymes that promote the removal of necrotic tissue.
- Mechanical debridement, is the use of debriding dressings, whirlpool or ultrasound for slough in a stable wound
- Surgical debridement, or sharp debridement, is the fastest method, as it allows a surgeon to quickly remove dead tissue
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
Reference
[edit | edit source]
- ↑ http://emedicine.medscape.com/article/190115-overview
- ↑ http://emedicine.medscape.com/article/190115-overview#a4
- ↑ http://emedicine.medscape.com/article/190115-overview#a2
- ↑ http://www.mayoclinic.org/diseases-conditions/bedsores/basics/causes/con-20030848
- ↑ 5.0 5.1 5.2 Susan B. O’Sullivan,Thomas J. Schmitz,George D. Fulk, Physical Rehabilitstion,6th edition,United States of America,F.A. Davis Company,2014
- ↑ http://www.mayoclinic.org/diseases-conditions/bedsores/basics/risk-factors/con-20030848
- ↑ https://www.npuap.org/national-pressure-ulcer-advisory-panel-npuap-announces-a-change-in-terminology-from-pressure-ulcer-to-pressure-injury-and-updates-the-stages-of-pressure-injury/
- ↑ http://www.mayoclinic.org/diseases-conditions/bedsores/basics/tests-diagnosis/con-20030848
- ↑ http://www.npuap.org/resources/educational-and-clinical-resources/pressure-injury-prevention-points/
- ↑ 10.0 10.1 http://www.mayoclinic.org/diseases-conditions/bedsores/basics/treatment/con-20030848
- ↑ http://www.fairview.org/healthlibrary/Article/84022
- ↑ http://www.hopkinsmedicine.org/gec/series/wound_care.html
- ↑ https://en.wikipedia.org/wiki/Pressure_ulcer