Prescribing in Physiotherapy for Pain
Prescribing in Physiotherapy for Pain: A Current and Emerging Role[edit | edit source]
Aim[edit | edit source]
With changing demographics, higher expectations and an increase in long term conditions [1] there is an heightened pressure and demand on the NHS. To meet these demands the roles within the NHS have had to change and expand.
As recently as 2013, physiotherapists in England have been granted the right to independently prescribe, giving them the ability to prescribe drugs, including some controlled drugs. These prescriptions must be used “within the overarching framework of human movement, performance and function” [2]
With these new responsibilities that are becoming a part of a physiotherapist’s remit, this page looks to explore prescribing as a physiotherapist. It also looks to provide information around their scope and responsibilities for prescribing for pain that impacts specialist musculoskeletal physiotherapist’s areas of expertise.
Audience: The resource was produced for use by Band 5 physiotherapists to understand the role the profession plays in prescribing medicines. It may be of benefit to other health professionals seeking knowledge. A case study and questions will be included, which can be used to check understanding after each section
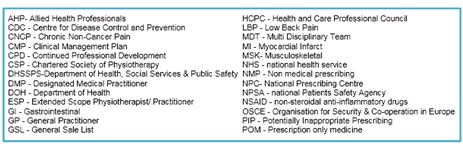
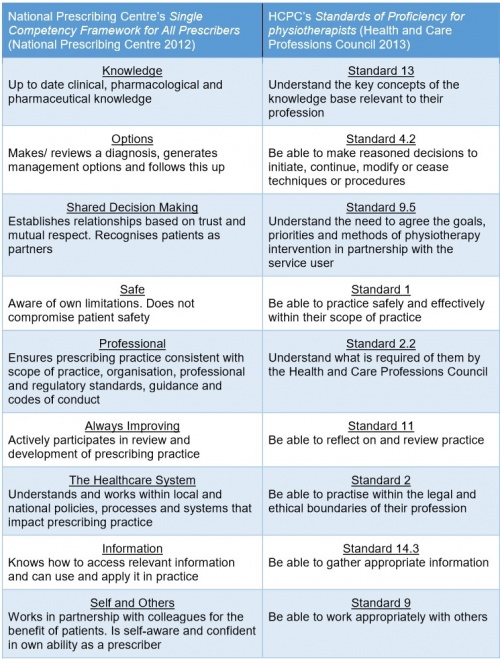
Abbreviations[edit | edit source]
Learning Outcomes[edit | edit source]
LO1. – The learner will able to complete the case study questions to demonstrate an understanding of prescribing within physiotherapy.
LO2. – the learner will be able to distinguish the scope of practice for non-prescribers, supplementary prescribers and independent prescribers within physiotherapy.
LO3. - The learner will be able to comprehend the process of how to become an independent and supplementary prescriber.
LO4. – The learner will be able to describe the effects & side effects of common groups of pain medication, and the role they have to play in patient centred care. Also, they should be able to provide general advice at a band 5 level for pain.
LO5. - The learner will be able to evaluate the effect of prescribing on the current and future role of physiotherapists.
Key Definitions[edit | edit source]
- Pain - The ISAP define pain as “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” http://www.iasp-pain.org/Taxonomy#Pain
- Extended Scope Practitioner - A clinician who applies and expands their expert knowledge and skills to areas of healthcare traditionally performed by another healthcare profession, which is currently seen as outside the scope of practice of the majority of their profession.[3]
- Drug Classes - A drug is put into a class based on the penalty it would have if there was any offence involving the drug.
- Non-prescribers - Physiotherapists without further training within the prescribing field, newly qualified Band 5’s fit within this areas.
- Supplementary prescriber- Those who have had some further training and have an agreed working relationship with a doctor or a dentist to implement treatment plans, any prescriptions that are written by this group must be signed off by the medical practitioner.
- Independent prescribers - Without consultation are able to either from their own diagnosis or a previous diagnosis prescribe treatment including prescribing and are fully responsible and accountable for the treatment. This should be done within the physiotherapists area of expertise.
- Non-Medical Prescriber - Any healthcare professional other than doctors or dentists who can independently prescribe medicine to a patient this includes physiotherapists nurses, podiatrists, pharmacists, chiropodists and optometrists.
Background[edit | edit source]
In 2013 in England and in 2014 for the rest of the UK, physiotherapists were given the right to train to prescribe independently. Below shows a timeline of Key dates:
insert picture here
As the healthcare needs of the British population change, the NHS must also change and adapt to meet them. For example, the British public are living longer and acquiring more long term conditions as a result. These are estimated to occupy 50% of the GP appointments and 70% of hospital beds. Another issue is that there is also thought to be an increase in the expectations of patients who want a co-ordinated, accessible 7-day service from the NHS. It has also been felt in literature that patients may find their healthcare experience disjointed and repetitive, due to a lack of integration between healthcare professionals (Morris 2002). Each of these puts extra pressure on a resource strapped service, with costs currently thought to be around £12.3 billion per year (Donaldson, 2008). To meet these challenges new approaches and changing roles are being implemented (NHS England 2013) .
Due to this setting of increasing demand and reducing resources, a supported decision was made to grant physiotherapists prescribing powers. Some of the many highlighted benefits of this for the patient include;
- Making a patient’s prescribing experience an easier, quicker and more streamlined pathway within a single appointment, reducing a patient’s total number of appointments within the NHS (NHS England Publications, 2013)
- Increasing involvement and independent management of a patient’s entire healthcare journey, as a result of the increasing use of physiotherapists as first-contact practitioners (Chartered Society of Physiotherapy 2013)
- Reducing demand on finite medical resources by preventing delays and contributing to a flexible team (DHSSPS, 2013)
- Utilising the skills of the non-medical professions expertise in their specialist area to provide patient centred care.
This was summed up by Phil Gray, chief executive of the Chartered Society of Physiotherapy, upon physiotherapists being awarded the right to independently prescribe said that:
"This is a landmark moment that will lead to patients receiving faster, more effective treatment for their condition” (BBC 2013).
Of the 94 physiotherapists who have taken this professional leap forward, six interviewed by the magazine Frontline indicated that they felt the greatest benefit of their prescribing power was the ability to streamline patient care. They felt that it allowed them to begin treating patients immediately, without having to send them back to their GP for sufficient pain relief, and allowed them to view the bigger picture of a patient’s care (Hunt 2015).
Whilst this resource looks to educate on the drugs used by physiotherapists for pain, physiotherapists are also using the independent prescribing power to help prescribe for other conditions such as spasticity management (Ashford et al 2014)
Scope of Practice[edit | edit source]
Prescribing may appear a strange addition to a physiotherapist’s toolkit and outside the remit of the profession, which are defined by the Chartered Society of Physiotherapy[4] as anything within the 4 pillars of practice. These are:
- Massage
- Exercise and movement
- Electrotherapy
- Kindred methods of treatment
Any physiotherapist must not only work within their own personal scope of practice, but also within the scope of the profession.[5]
? Do you think prescribing is within the scope of physiotherapy?
In a narrative review[3], comment that physiotherapists demonstrate an excellent ability to clinically reason and adapt to the changing needs of the societies they serve. The UK government has been convinced that prescribing is within physiotherapy’s scope because physiotherapists already possess the core skills that it requires.
The National Prescribing Centre[6] has produced a framework that applies to all prescribers, no matter what profession they come from. Below is a comparison of this framework it to the HCPC’s Standards of Proficiency for physiotherapists[7]:
Personal Scope of Practice[edit | edit source]
Although prescribing is within the scope of the profession, like any skill, it only becomes part of an individual physiotherapist’s scope of practice when they become competent through training[5]. This means that before prescribing is suitable addition to a physiotherapist’s skill set, they must already be an expert in the field they wish to apply it[6]. As a consequence, although the scope of prescribing within in physiotherapy is very wide, it is limited to only an individual's clinical specialty.[5] This is a major difference from medical prescribing who may prescribe for any condition.
! It is important to remember that prescribing physiotherapists are not the equivalent of doctors, and their practice is restricted to their own patients, who they have performed a comprehensive assessment on.[5]
? You may reach a point in your career where begin to feel that you have gained enough knowledge, training and experience that prescribing is becoming within your scope of practice. Would you be able to ‘tick all these boxes’? Only then is prescribing completely within your scope[8]:
Insert boxes here
Once a physiotherapist decides that prescribing would be of benefit and for their practice there are two types of prescriber they can become, based on their level of training.
Supplementary Prescribers[edit | edit source]
Supplementary prescribers can prescribe any medication, but it must be detailed in a written CMP. The CMP is created in partnership with the patient and a medical prescriber.[5] This means that although they are accountable for their decision to prescribe, they share accountability with the medical prescriber for the decision to put the medication in the CMP.[5] In their nursing supplementary prescriber counterparts, this leads many doctors to feel that they have the ultimate responsibility for both supplementary prescriber and patient. This can result in supplementary prescribers feeling subordinate, rather than in partnership with their medical prescriber.[9]
Supplementary prescribing is particularly suited to the care of chronic conditions, as once a CMP is in place, medical prescriber can pass over management of a patient to the supplementary prescriber. Supplementary prescribers have expert knowledge of medications within their specialty, and can therefore modify or prescribe any drug detailed within the CMP, but have no influence on drugs that patients receive for other co-morbidities.[4] As experts in prescribing they may also provide detailed advice on any aspect of a medication for a patient, so long as they are used in their area of clinical specialty.[4]
Independent Prescribers[edit | edit source]
Independent prescribers share many features and core skills with supplementary prescribers.[6] However, as they prescribe completely autonomously and not in partnership with medical prescribers, they are wholly responsible for every aspect of the prescribing process.[5] They can actually prescribe fewer medicines than a supplementary prescriber, but are fully autonomous when doing so. As a result, Creedon et al.[9] feel that they represent a greater challenge to medical authority.
? Do you think you would rather become a supplementary or independent prescriber? What would be a more useful adjunct to your practice?
How does a physiotherapist decide what is within their scope? In a qualitative study by Dawson and Ghazi[10] of physiotherapists working in similar roles, as extended scope practitioners in orthopaedic clinics, many participants commented that they felt many of the skills required were beyond the current scope of physiotherapy. However, all felt confident in their jobs despite this, as they were aware of their limitations and able to liaise with their medical colleagues when in need of advice. This really highlights the key question any responsible physiotherapy prescriber should ask themselves when deciding what is within their scope. Simply put, it is ‘do I feel confident practicing this, with my current level of knowledge and skill set?’ This directly relates to some of the key competencies of a good prescriber, detailed by the Single Competency Framework For All Prescribers[6], where prescribers, irrespective of who they are, should be self-aware, aware of their limitations, and confident in their ability.
Non-Prescribers[edit | edit source]
The vast majority of physiotherapists globally are not prescribers and there appears to be debate regarding what their level of involvement in prescribing should be. In Australia, like in the UK, this is felt to be a legislative ‘grey’ area; different physiotherapist have different opinions on the extent of their scope regarding medicines.[11] This is reflected in the guidance provided by professional bodies, as they feel an individual’s scope should vary depending on the depth of knowledge that they can demonstrate.[4]
Studies investigating this have found that physiotherapists are frequently asked a wide variety of questions regarding NSAIDs and often feel pressured by patients to provide advice and recommendations regarding them. Almost all felt concerned that they lacked sufficient knowledge to confidently provide this, commensurate with their duty of care to their patients.[12]
Kumar and Grimmer[13] also found that most of the physiotherapists were not aware of the up to date research that has influenced best practice for NSAIDs. It would therefore be argued that this was not within the scope of these physiotherapists. It is expected in the UK that all newly qualified Band 5 physiotherapists should be sufficiently competent to advise patients on where to find appropriate advice regarding their medications, and give appropriate advice of medications that might be suitable for a patient. If they can demonstrate their competence, they can give general information on a medicine, such as widely known side-effects of a commonly accessible medicine like ibuprofen.[4] However, they are keen to stress there is a difference between giving advice and prescribing, and therefore non-prescribing physiotherapists can not suggest alterations to a patient’s prescribed medications.
! Importantly, if you notice a patient is taking a medication wrongly, you can show them the directions that have been prescribed. If you feel a medicine would be of benefit to a patient, you can suggest they speak to their doctor regarding it; and if you are concerned of the effects of a medication you may ask them to speak to their doctor, or directly contact them.[4]
There are a few very specific emergency events where a non-prescribing physiotherapist may aid the administration of drugs. If a patient brings in their medication, with instructions, in an emergency, you may administer drugs in accordance with these, as you are assisting them to take their prescribed medication. In an emergency, like any member of the public, a physiotherapist can also lawfully give certain life-saving POMs to someone acutely unwell without a prescription. The most important of these is adrenaline which is indicated for anaphylactic shock.[4]
Below is a useful summary of who can prescribe and what they can prescribe:
Insert table xxx here
Case Study Questions[edit | edit source]
- Mr Smith also mentions he is having terrible trouble with indigestion, you hear him ask your independent prescriber colleague, seeing as they are already writing him a prescription, to give him something to help. Can they?
- At lunch your colleague discusses their patient with you. They feel that they would benefit from tramadol and are considering asking an independent prescriber colleague to prescribe it. What should you say?
- Could you, as a non-prescriber, recommend Mr Smith also take paracetamol for his pain?
Answers
- No. As a MSK specialist, they only have sufficient knowledge on MSK conditions to prescribe safely. Although they may know a little about the gastrointestinal system, it is out of their scope of practice to treat it as a clinician. They are a specialist clinician, not a one-stop shop! Mr Smith should see his doctor.
- Your colleague has 2 options: either recommend the patient sees their GP and ask for tramadol on their recommendation; or they can pass this patient onto an independent prescriber under their caseload. They would really need to see the patient and complete a full assessment of them before it would be safe to prescribe tramadol. In either case, it can’t be guaranteed that the patient will receive tramadol, as it may not be suitable
- No, this would be outside of your scope. Although this is a very widely known drug, available under a GSL, Mr Smith is on a variety of other medications. You currently don’t have the detailed knowledge of drug interactions to recommend this safely.
Accountability in Prescribing[edit | edit source]
It is not enough for a physiotherapists to feel that prescribing is within their scope of practice. There must be some way that they are held accountable for their actions, and prove their competency and appropriate scope of practice. Two of the main ways that this can be done is through audits and CPD[5], where physiotherapists review their practice, or seek to increase their knowledge and skills.
Physiotherapists are not only responsible for their prescribing decisions, but also every aspect of the prescribing process they are involved in. Both supplementary and independent prescribers are accountable for the decision to delegate the administration of a medicine to someone else, such as the patient or another healthcare professional, although if their decision is justified, they are not accountable for how well the individual carries out the task.[5] This could be thought of as prescribers having to not only judge their own scope, but also the scope of practice of others.
The literature identifies that physiotherapy as a profession demonstrates internal and external accountability measures already in place, but an individual’s internal rigor of accountability has the potential to be flawed.[14] This may be a particular risk for prescribers within physiotherapy. As this is such as emerging role, like many other advanced scope practitioners, their job description and scope of practice is often still subject to revision and alteration.[3] This lack of definition to their role gives them less external support in deciding their role, making them rely more on their own internal accountability measures, which may be subject to disagreement between professionals.
Evidence Base For Prescribing Within Physiotherapy.[edit | edit source]
Overall, there is a lack of high quality evidence into the effectiveness of prescribing within physiotherapy, and this is a concern which needs to tackled by the profession.[15] We speculate, however, that this may well reflect the currently low levels of qualified prescribers and the novelty of this emerging role. However, the University of Surrey is currently conducting a study to understand the impact of prescribing by physiotherapists.
Despite this, there is evidence emerging that prescribing is within the scope of physiotherapy. Effective prescribing relies on the diagnostic accuracy of the prescriber. Physiotherapists in a range of MSK advanced scope roles have be shown through randomised controlled trials and systematic reviews to have equal diagnostic skill to orthopaedic surgeons and to be more accurate than other healthcare professionals, including non-orthopaedic physicians.[16][17] In addition to this, the UK Department of Health for the year January 2005 to January 2006 reported that of the 60,000 medication incidents, none were related to physiotherapists.[11]
From the body of evidence regarding the more established nurse prescribing, it has been found that patients have embraced this due to the ease of access, reduced waiting times, knowledge, safety and holistic nature of nurse practice.[9] Norman et al.[18] have also found that non-medical prescribing made no difference to self-reported adherence to medication regimes, compared to medical prescribing, in the mental health setting. We can tentatively assume that some of these may be shared features, as the role within physiotherapy expands.
The effect on patients should be the most important aspect for any change in role, and Gimore et al.[19] comment that professions should only expand their scope when there is a clear patient need. Within the nursing profession, patients opinions on nurse prescribing have become increasingly favourable as more patients experience it.[9] They report that patients are very satisfied and feel confident with nurse prescribing. This paper believes that key to this is the nurse-patient relationship, as patients find them easier to speak to, better at communicating and more likely to implement shared decision making than doctors.[9] Norman et al.[18] also found the only significant difference between nurse supplementary prescribing and medical prescribing in the mental health setting was that of the higher patient satisfaction in those allocated to nurse prescribers. The general public has also expressed an opinion that they support nurse prescribing, and that non-medical versus medical prescribers would make no difference to their adherence.[20] In addition to this, a national survey of nurses and pharmacists in 2008[21] suggested that their non-medical prescribing was also highly accepted by both the patient and MDT.
This has been reflected in the preliminary findings for physiotherapy. Physiotherapists working in an extended scope, including supplementary prescribing, in emergency departments have been shown to produce higher satisfaction rates than doctors or extended nurse practitioners. Patients felt they reduced waiting times and spent more time giving better advice and explanations, which educated and empowered them.[22] In a systematic review, physiotherapists have been noted to provide significantly more advice, prescribe less medication and have higher rates of patient satisfaction than doctors.[16] In their literature review, Kersten et al.[15] found that the vast majority of sources were supportive of physiotherapists working in extended scope roles.
In a qualitative study of physiotherapists working in extended scope roles in Scotland, all commented that they felt they have learned and changed as physiotherapists through their extended roles. They felt better and more efficient at assessments, and enjoyed being able to treat patients more comprehensively. However they noted increased anxiety and pressure which came with these roles, risking burn-out, and feeling as if they had hit a ceiling of specialisation.[10] This was shared with nurse prescribers, who felt prescribing had increased their autonomy and effectiveness, but came with increased workload, anxiety about ability, increased personal cost and concern over effect on professional relationships.[9] Sadly, like other non-medical prescribers, such as nurses and pharmacists, who indicated that not all of those trained were currently prescribing (86% of nurses and 71% of pharmacists) (Latter et al. 2010), one third of qualified prescriber AHPs indicated they did not prescribe.[23] Within the same study it was commented that rates of prescribing are related to the levels of support they receive throughout their journey as a prescriber.[23] However, due to the novel nature of non-medical prescribing, Stewart et al.[24]note that there is a lack of substantial, longitudinal and high quality research on this group of prescribers.
Insert diagram 1 xxxx here
? At the beginning of this section, you were asked to reflect whether you believed prescribing to be within the scope of physiotherapy. What are your opinions now?
References[edit | edit source]
- ↑ Department of Health. Long-term conditions compendium of information: 3rd edition. 2012; Available at: https://www.gov.uk/government/publications/long-term-conditions-compendium-of-information-third-edition. Accessed 5th November, 2015.
- ↑ NHS England Publications. Frequently Asked Questions: Independent prescribing by physiotherapists and podiatrists Publications Gateway Reference 00364 . 2013; Available at:https://www.england.nhs.uk/wp-content/uploads/2013/08/faqs-ippp1.pdf. Accessed 15th November, 2015.
- ↑ 3.0 3.1 3.2 Crane J, Delany C. Physiotherapists in emergency departments: responsibilities, accountability and education. Physiotherapy 2013; 99:95-100.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy. file:///C:/Users/user/Downloads/csp_pd019_medicines_prescribing_physiotherapy_2013_0.pdf (accessed 25 Oct 2015)
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Chartered Society of Physiotherapy. Practice guidance for physiotherapist supplementary and/or independent prescribers in the safe use of medicines. file:///C:/Users/user/Downloads/csp_pd026_practice_guidance_prescribers_aug2013_0_0.pdf (accessed 25 Oct 2015)
- ↑ 6.0 6.1 6.2 6.3 National Prescribing Centre., A single competency framework for all prescribers. http://www.webarchive.org.uk/wayback/archive/20140627112901/http://www.npc.nhs.uk/improving_safety/improving_quality/resources/single_comp_framework_v2.pdf (accessed 6 Nov 2015)
- ↑ Health and Care Professions Council. Standards of proficiency: Physiotherapists. http://www.hcpc-uk.co.uk/assets/documents/10000DBCStandards_of_Proficiency_Physiotherapists.pdf (accessed 11 Nov 2015).
- ↑ Health and Care Professions Council. Standards for prescribing. http://www.hcpc-uk.org/assets/documents/10004160Standardsforprescribing.pdf (accessed 6 Nov 2015)
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. British Journal of Nursing 2015; 24:878-885.
- ↑ 10.0 10.1 Dawson LJ, Ghazi F. The experience of physiotherapy extended scope practitioners in orthopaedic outpatient clinics. Physiotherapy 2004; 90:210-6.
- ↑ 11.0 11.1 Morris JH, Grimmer K. Non-medical prescribing by physiotherapists: Issues reported in the current evidence. Manual Therapy 2014; 19:82-6.
- ↑ Kumar S, Grimmer K. Nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy management of musculoskeletal conditions: a professional minefield? Therapeutics and Clinical Risk Management 2005; 1:69-76.
- ↑ Kumar S, Grimmer K. Nonsteroidal anti-inflammatory drugs (NSAIDs) and physiotherapy management of musculoskeletal conditions: a professional minefield? Therapeutics and Clinical Risk Management 2005; 1:69-76.
- ↑ Morris J. Current issues of accountability in physiotherapy and higher education: implications for physiotherapy educators. Physiotherapy 2002; 88:354-63.
- ↑ 15.0 15.1 Kersten P, McPherson K, Lattimer V, George S, Breton A, Ellis B. Physiotherapy extended scope of practice - who is doing what and why? Physiotherapy 2007; 93:235-42.
- ↑ 16.0 16.1 Desmeules F, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advance practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskeletal Disorders 2012; 13:1-21.
- ↑ Daker-White G, Carr AJ, Harvey I, Wollhead G, Bannister G, Nelson I, Kammerling M. A randomised controlled trial. Shifting the boundaries of doctors and physiotherapists in orthopaedic outpatient departments. Journal of Epidemiology and Community Health 1999; 53:643-50.
- ↑ 18.0 18.1 Norman IJ, Coster S, McCrone P, Sibley A, Whittlesea C. A comparison of the clinical effectiveness and costs of mental health nurse supplementary prescribing and independent medical prescribing: a post-test control group study. BMC Health Services Research 2010; 10:1-9.
- ↑ Gimore LG, Morris JH, Murphy K, Grimmer-Somers K, Kumar S. Skills escalator in allied health: a time for reflection and refocus. Journal of Healthcare Leadership 2011; 3:53-8.
- ↑ Berry D, Courtenay M, Bersellini E, Attitudes towards, and information needs in relation to supplementary nurse prescribing in the UK: an empirical study. Journal of Clinical Nursing 2006; 15:22-8
- ↑ Cooper R, Anderson C, Avery T, Bissell P, Guillaume L, Hutchinson A, et al. Stakeholders' views of UK nurse and pharmacist supplementary prescribing. J Health Serv Res Policy 2008 Oct;13(4):215-221.
- ↑ McClellan CM, Greenwood R, Benger JR. Effect of an extended scope of physiotherapy service on patient satisfaction and the outcome of soft tissue injuries in an adult emergency department. Emergency Medicine Journal 2006; 23:384-7.
- ↑ 23.0 23.1 COURTENAY, M., CAREY, N. and STENNER, K., 2012. An overview of non medical prescribing across one strategic health authority: a questionnaire survey. BMC Health Services Research. Jun, vol. 12, pp. 138-151.
- ↑ Stewart D, MacLure K, George J. Educating nonmedical prescribers. Br J Clin Pharmacol 2012;74(4):662-667.