Prepatellar Bursitis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Kim Jackson moved page Prepatellar bursitis to Prepatellar Bursitis) |
||
| (20 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
<div class="editorbox"> | '''Original Editor ''' [[User:Daan Vandebriel|Daan Vandebriel]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition/ Description == | == Definition/ Description == | ||
Prepatellar bursitis is also called housemaid's knee or carpenter's knee. A bursa is a fluid-filled sac which ensures there is less friction between body parts. The prepatellar bursa is located | Prepatellar bursitis is also called housemaid's knee or carpenter's knee. A bursa is a fluid-filled sac which ensures there is less friction between body parts. The prepatellar bursa is located superficially between the skin and the patella. The inflammation of a bursa is called [[bursitis]]. This inflammation can take form by either an infectious nature (30%) or a non-infectious nature (70%). A direct fall on the [[patella]], an acute trauma, repeated blows or friction on the knee may cause prepatellar bursitis. Other causes include infections or low-grade inflammatory conditions, such as [[gout]], [[syphilis]], [[tuberculosis]] or [[Rheumatoid Arthritis|rheumatoid arthritis]].<ref name="p5">Yu-Chih H, et al. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011; 35(3): 355–358. (2)</ref> Prepatellar bursitis often occurs in specific jobs which involves a position where they work on their knees for a prolonged period of time such as miners, gardeners, carpet layers and mechanics.<ref name="p5" /> | ||
Prepatellar bursitis often occurs in specific jobs which | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
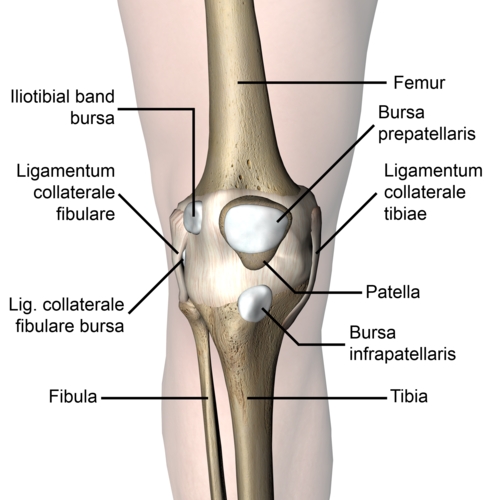
The | The patella is a triangular-shaped bone in front of the knee. It moves up and down in the groove of the [[femur]] when you bend and straighten your knee. The patellar tendon is a thick structure that connects the bottom of the patella with the tibia. The upper part of the patella is connected to the quadriceps, which allows the knee extension and moves the patella upwards. Bursae around the knee can be divided into two groups- those around the patella (suprapatellar bursa, the superficial and deep infrapatellar bursae & prepatellar bursa) and those that occur elsewhere (pes anserinus bursa and the iliotibial bursa) <ref name="p4">Mcafee J.H. et al.. Olecranon and prepatellar bursitis: diagnosis and treatment. West Journal Medecine, 1988; 149: 607-610.</ref><sup> </sup><ref name="p5" /><br> | ||
[[Image:Knee_bursas.png]] |{{#ev:youtube|CZ18PGwUG-0}} | |||
== Epidemiology == | |||
Prepatellar bursitis affects men more often than women and it can emerge at all ages. 80% of the people with prepatellar bursitis are men aged between 40 – 60 years. 1/3 of the prepatellar bursitis are septic and 2/3 are non-septic. <ref name="p3">Le Manac’h A.P. et al. Prevalence of knee bursitis in de workforce. Occupational medecine 2012; 62: 658-660</ref> An infectious prepatellar bursitis emerges more often with children than grown-ups. Prepatellar bursitis occurs often, with at least an annual incidence of 10/100 000. The incidence of prepatellar bursa is probably underestimated because most of the case are non-septic and only patients with the most severe cases of prepatellar bursitis requires admission in the hospital. <ref name="p2">Baumbach, S.F., et al. Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Archives of Orthopaedic and Trauma Surgery 2014; 134: 359.</ref> | |||
== Epidemiology | |||
Prepatellar bursitis affects men more often than women and it can emerge at all ages. 80% of the people with prepatellar bursitis are men aged between 40 – 60 years. 1/3 of the prepatellar bursitis are septic and 2/3 are non-septic. <ref name="p3">Le Manac’h A.P. et al. Prevalence of knee bursitis in de workforce. Occupational medecine 2012; 62: 658-660</ref> An infectious prepatellar bursitis emerges more often with children than grown-ups. Prepatellar bursitis occurs often, with at least an annual incidence of 10/100 000. The incidence of prepatellar bursa is probably underestimated because most of the case are non-septic and only patients with the most severe cases of prepatellar bursitis requires admission in the hospital. <ref name="p2" /> | |||
== Etiology == | == Etiology == | ||
* Direct | * Direct trauma/blow to the anterior knee | ||
* | * Frequent falls on the knee | ||
* Constant friction between the [[skin]] and the patella <ref name="p5" /> can be a cause of this condition. By the impact, the damaged blood vessels in the knee result in inflammation and swelling of the bursa. Actually, a bacterial seeding of the bursal sac caused by a hematoma is rare, because of the limited vascular supply of the bursal tissue. | |||
<sup></sup> | * Infection:Typically for a septic prepatellar bursitis is a break in the skin near the bursa, which leads to swelling and pain around this area. This happens when a bacteria (for example S. Aureus, 80% of the cases) have passed across the soft tissues from a break in the skin and begins to multiply within the bursa. <ref name="p4" /> When a bursa is infected it can probably cause pain, fever, tenderness and an elevated amount of white blood cells. | ||
* Co-existing inflammatory disease- [[Rheumatoid Arthritis|rheumatoid arthritis]], [[gout]] etc. <sup></sup> | |||
== Characteristics/Clinical Presentation == | |||
* Pain | |||
== Characteristics/Clinical Presentation | * Swelling<ref>Rennie, WJ, Saifuddin, A. Pes anserine bursitis: incidence in symptomatic knees and clinical presentation. Skeletal Radiol 2005; 34:395.</ref> | ||
* Differential warmth around the knee | |||
* Painful and limited ROM at the knee | |||
* If bursitis is caused by an infection, pain is associated with fever and chills. | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 48: | Line 35: | ||
* [[Lateral Collateral Ligament Injury of the Knee|Lateral Collateral Ligament Injury]] | * [[Lateral Collateral Ligament Injury of the Knee|Lateral Collateral Ligament Injury]] | ||
* [[Osteoarthritis]] | * [[Osteoarthritis]] | ||
* Pes Anserinus bursitis | * [[Pes Anserinus Bursitis|Pes Anserinus bursitis]] | ||
* [[Posterior Cruciate Ligament Injury]] | * [[Posterior Cruciate Ligament Injury]] | ||
* [[Rheumatoid Arthritis]] | * [[Rheumatoid Arthritis]] | ||
* Patellar tendon rupture | * [[Patellar tendon tear|Patellar tendon rupture]] | ||
* Chondromalacia patellae | * Chondromalacia patellae | ||
* Patellofemoral pain | * [[Patellofemoral Pain Syndrome|Patellofemoral pain]] | ||
== Diagnostic Procedures == | |||
<ref>van Everdingen, J.J.E. Diagnose en therapie. Bohn, Springer Uitgeverij, 2010, 943 pagina’s. (5)</ref>Bursitis can be diagnosed through a detailed history (about the onset of symptoms, the pattern of knee pain and swelling and how the symptoms affect their lifestyle)<ref>Housten Methodist, eOrthopod Medical Multimedia Group L.L.C. Prepatellar bursitis: A patient’s guide to prepatellar bursitis. http://www.houstonmethodist.org/orthopedics/where-does-it-hurt/knee/prepatellar-bursitis (accessed 5 November 2016). (5)</ref> and a physical examination, however, X-ray, MRI and CT-scan can be done to rule out the possibility of a fracture or soft tissue injury. If it is uncertain whether or not the bursa is infected, an arthrocentesis can be done. It is typically done for three reasons: necessary information is needed to make a diagnose, to relieve the pressure in the joint and will help alleviate the pain and excess fluid also needs to be removed before a therapeutic injection is given. <ref name="p0">Dean Cole., J. MD, (2013), Knee (prepatellar) bursitis. http://www.arthritis-health.com/types/bursitis/knee-prepatellar-bursitis (accessed 5 November 2016). (5)</ref> | |||
== Outcome Measures == | == Outcome Measures == | ||
* [[Visual Analogue Scale]] | * [[Visual Analogue Scale]] | ||
* | * [[Knee Injury and Osteoarthritis Outcome Score|KOOS Questionnaire]]: consists of 5 subscales (Pain, other Symptoms, Function in daily living ADL, Function in sport and recreation and knee-related quality of life). Each question gets a score from 0 to 4 and a normalized score is calculated for each subscale (100 = no symptoms and 0 = extreme symptoms). <ref name="p7">Peer M.A. et al., The Knee Injury and osteoarthritis Outcome Score (KOOS): A Review of its Psychometric Properties in People Undergoing Total Knee Arthroplasty. Journal of Orthopaedic and Sports Physicial Therapy 2013; (4057), 43 .</ref> | ||
* Anterior Knee Pain Scale: to measure the functions<ref name="p8">Panken AM. et al. Clinical Prognostic factors for patients with anterior knee pain in physical therapy: systematic review. int J sports Phys ther 2015; 929-945.</ref> | |||
* Anterior Knee Pain Scale: to measure the functions<ref name="p8">Panken AM. et al. Clinical Prognostic factors for patients with anterior knee pain in physical therapy: systematic review. int J sports Phys ther 2015; 929-945.</ref | |||
== Physical Examination == | == Physical Examination == | ||
| Line 76: | Line 58: | ||
* Pain | * Pain | ||
* Range of motion | * Range of motion | ||
When there is a limited range of motion or swells, a doctor may recommend using a needle and syringe to remove the fluid from the joint. This fluid can be send to labs for testing whether or not the bursa is infected. Common tests for infection are gram stain, white blood cell count (an elevated number of white blood cells in the [[Synovial Fluid Analysis|synovial fluid]] indicates infection) and glucose levels tests (when the levels are significantly lower than normal it may indicate an infection). Gram stain is used to determine if there are certain troublesome bacteria present. Not all bacteria’s can be identified. Even when the test comes back negative, septic bursitis cannot be completely ruled out. <ref name="p0" /> | |||
== Medical Management == | == Medical Management == | ||
The primary goal of treatment is to control the inflammation. | The treatment for prepatellar bursitis depends primarily on the cause of the bursitis and secondarily on the pathological changes in the bursa.<ref>Crenshaw AH. Campbells’s operative orthopaedics. St Louis: Mosby; 1992.</ref> The primary goal of treatment is to control the inflammation. | ||
* Conservatively, the [http://www.physio-pedia.com/RICE R.I.C.E regime] <ref name="p5" /> in the first 72 hours after the injury or when the first signs of inflammation appear. | |||
* Medications including non-steroidal anti-inflammatory drugs, topical medications- creams, sprays, gels and patches can provide pain relief when those are directly applied to the skin over the knee. To reduce the gastrointestinal side effects that can be caused by oral medications, topical medications may be a good choice. Also, for cases of septic prepatellar bursitis, antibiotics are used to treat the infection. | |||
* Corticosteroid injections | |||
== Surgical Management== | |||
When conservative treatments have failed for chronic/post-traumatic prepatellar bursitis, outpatient arthroscopic bursectomy under local anaesthesia is an effective procedure. Arthroscopic or endoscopic excision of the bursa has more recently been reported to have satisfactory results with less trauma than open excision.<ref>Huang YC, Yeh WL. Endoscopic treatment of prepatellar bursitis. ''Int Orthop''. 2011 Mar. 35(3):355-8. </ref><ref>Gendernalik JD, Sechriest VF 2nd. Prepatellar septic bursitis: a case report of skin necrosis associated with open bursectomy. ''Mil Med''. 2009 Jun. 174(6):666-9.</ref> | |||
=== Operative Technique === | |||
The patients are placed in a supine position and the tourniquet will be routinely applied on the thigh and not inflated until necessary. The skin will be prepared in an aseptic manner over the whole lower extremity. A solution will be infiltrated at the portal site and into the cavity, respectively a 1% xylocaine solution with a 1:100,000 epinephrine. For monitoring a 2.7-mm, 30-degree endoscope will be used and a 2.7-motorised shaver to remove thickened synovium. Two or three 2mm portals will be made; an anterior medial portal and anterior lateral portal are routinely used and if necessary a superior lateral portal. To make a 2mm incision for each portal, a no. 11 scalpel will be used. After this, the trochar will be inserted into the cavity and the other instruments will follow. The bursa cavity and synovial thickening are directly visible by the endoscopy. The motorized shaver inserts through the other portal and total synovectomy including the bursa will be performed until all the pathological lesions are removed. When all the procedures are completed, the portals will be closed with adhesive tape without any suture. The anterior knee area is dressed with loosely unfolded gauze, padding and bandage are applied. <ref name="p5" /> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
The | The Rest, Ice, Compression and Elevation method<ref>Michel P.J, et al., What Is the Evidence for Rest, Ice, Compression, and Elevation Therapy in the Treatment of Ankle Sprains in Adults?. Journal of Athletic Training 2012; 47(4): 435-443. (2)</ref> (level of evidence 2a) is commonly used treatment for prepatellar bursitis. The ‘rest-phase’ consists of a short period of immobilization. This period should be limited to the first days after the trauma. Resting will reduce the metabolic demands of the injured tissue and will avoid increased blood flow. The use of ice will cause a decrease of the temperature of the tissues in question, inducing vasoconstriction and a limitation of the bleeding. Also, the pain will decrease because cold will cause increasing threshold levels in the free nerve endings and at synapses. Don’t place the ice too long on your knee (maximum 20 minutes at a time with an interval of 30-60 minutes). The compression will decrease the intramuscular blood flow to the affected area and will also reduce the swelling. At lastly there is the elevation. This ensures that the hydrostatic pressure will decrease and it will also reduce the accumulation of interstitial fluid. This part of the Rice-principle also decreases the pressure in local blood vessels and helps to limit the bleeding. However, the effectiveness of this RICE-method has not been proven in any randomized clinical trial. <ref>Baoge L., et al. Treatment of Skeletal Muscle Injury: A Review. ISRN Orthop. 2012.(5)</ref> | ||
Once the initial inflammation has reduced a program of stretching and light strengthening will be initiated to restore full motion and improve strength to reduce stress on the tendons and [[Knee|knee joint]]. Therapeutic exercises to strengthen and stretch the muscles of the knee. This includes static contraction of the quadriceps<ref>SIP, W. Kracht- en stabiliteitstraining. BOSU, 2010. (5)</ref>. This should be an exercise that the patient can do at home 1 to 3 times a day. The objective of the rehabilitation is that the patient can resume their everyday activities. To see if the exercise is working you have to put your fingers on the inner side of the quadriceps, you will feel the muscle tighten during the contraction of the muscle. The patient has to hold his contraction for 5 seconds; the exercise can be repeated 10 times as hard as possible. It is important not to forget this exercise must be pain-free. | |||
Also, the stretching of the [[Quadriceps Muscle|quadriceps]] is a good exercise for the patient, it reduces the friction between the skin and the patella tendon. There is less friction when the patella tendon is more flexible. The physiotherapist can also help the patient by using electrotherapy modalities and patient education on the use of knee pads for kneeling activities. | |||
== Prevention == | == Prevention == | ||
In order to prevent | In order to prevent prepatellar bursitis you should avoid injury or an overload of your muscles. It is very important to do an appropriate warm-up and cool down, while playing sports. For example, if you play volleyball, it is advisable to wear knee pads. This will prevent falling on the kneecap. Also when you spent a lot of time on your knees is it advisable to wear knee pads. Another important thing to avoid prepatellar bursitis is to check if the flexibility of the knee and the strength and endurance of the leg muscles stays optimal. <ref name="p4" /> | ||
== Key Research == | == Key Research == | ||
* Yu-Chih H, et al. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011; 35(3): 355–358.(2) | * Yu-Chih H, et al. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011; 35(3): 355–358.(2) | ||
| Line 132: | Line 93: | ||
== Resources == | == Resources == | ||
• http://www.drlox.com/knee-pain-v2/knee-bursitis/<br>• http://www.houstonmethodist.org/orthopedics/where-does-it-hurt/knee/prepatellar-bursitis<br>• http://www.arthritis-health.com/types/bursitis/knee-prepatellar-bursitis | • http://www.drlox.com/knee-pain-v2/knee-bursitis/<br>• http://www.houstonmethodist.org/orthopedics/where-does-it-hurt/knee/prepatellar-bursitis<br>• http://www.arthritis-health.com/types/bursitis/knee-prepatellar-bursitis | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
The prepatellar bursa is located under the skin and occurs in most people. When a bursa is inflamed, it's called | The prepatellar bursa is located under the skin and occurs in most people. When a bursa is inflamed, it's called bursitis. The inflammation can be of an infectious nature or a non-infectious nature. Many different aetiologies have been proposed as the cause of prepatellar bursitis. Chronic inflammation of prepatellar bursa after repetitive minor trauma is called ‘housemaid’s knee’. It can be seen in those who have to kneel very often, such as carpet layers and housemaids. Also a fall directly on the patella, an acute trauma, may cause patellar bursitis. Treatment for prepatellar bursitis depends primarily on the cause of bursitis and secondarily on the pathological change in the bursa. A surgical procedure is in most cases not required, but if needed, the surgical procedures involved are (1) aspiration and irrigation with a suitable drug, (2) incision and drainage in cases of acute suppurative bursitis, and (3) excision of chronically infected and thickened bursa. <ref name="p5" /> | ||
== References == | == References == | ||
| Line 147: | Line 105: | ||
[[Category:Knee]] | [[Category:Knee]] | ||
[[Category: | [[Category:Conditions]] | ||
[[Category: | [[Category:Knee - Conditions]] | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Sports Injuries]] | [[Category:Sports Injuries]] | ||
[[Category:Bursitis]] | [[Category:Bursitis]] | ||
Latest revision as of 15:34, 19 October 2023
Original Editor Daan Vandebriel Top Contributors - Annelore Oyen, Simisola Ajeyalemi, Heleen Van Cleynenbreugel, Oyemi Sillo, Venus Pagare, Kim Jackson, Blessed Denzel Vhudzijena, WikiSysop, Roxane Ost, Wanda van Niekerk, Elodie Baele, Candace Goh, Claire Knott, 127.0.0.1, Admin, Tony Lowe and Daan Vandebriel
Definition/ Description [edit | edit source]
Prepatellar bursitis is also called housemaid's knee or carpenter's knee. A bursa is a fluid-filled sac which ensures there is less friction between body parts. The prepatellar bursa is located superficially between the skin and the patella. The inflammation of a bursa is called bursitis. This inflammation can take form by either an infectious nature (30%) or a non-infectious nature (70%). A direct fall on the patella, an acute trauma, repeated blows or friction on the knee may cause prepatellar bursitis. Other causes include infections or low-grade inflammatory conditions, such as gout, syphilis, tuberculosis or rheumatoid arthritis.[1] Prepatellar bursitis often occurs in specific jobs which involves a position where they work on their knees for a prolonged period of time such as miners, gardeners, carpet layers and mechanics.[1]
Clinically Relevant Anatomy[edit | edit source]
The patella is a triangular-shaped bone in front of the knee. It moves up and down in the groove of the femur when you bend and straighten your knee. The patellar tendon is a thick structure that connects the bottom of the patella with the tibia. The upper part of the patella is connected to the quadriceps, which allows the knee extension and moves the patella upwards. Bursae around the knee can be divided into two groups- those around the patella (suprapatellar bursa, the superficial and deep infrapatellar bursae & prepatellar bursa) and those that occur elsewhere (pes anserinus bursa and the iliotibial bursa) [2] [1]
Epidemiology[edit | edit source]
Prepatellar bursitis affects men more often than women and it can emerge at all ages. 80% of the people with prepatellar bursitis are men aged between 40 – 60 years. 1/3 of the prepatellar bursitis are septic and 2/3 are non-septic. [3] An infectious prepatellar bursitis emerges more often with children than grown-ups. Prepatellar bursitis occurs often, with at least an annual incidence of 10/100 000. The incidence of prepatellar bursa is probably underestimated because most of the case are non-septic and only patients with the most severe cases of prepatellar bursitis requires admission in the hospital. [4]
Etiology[edit | edit source]
- Direct trauma/blow to the anterior knee
- Frequent falls on the knee
- Constant friction between the skin and the patella [1] can be a cause of this condition. By the impact, the damaged blood vessels in the knee result in inflammation and swelling of the bursa. Actually, a bacterial seeding of the bursal sac caused by a hematoma is rare, because of the limited vascular supply of the bursal tissue.
- Infection:Typically for a septic prepatellar bursitis is a break in the skin near the bursa, which leads to swelling and pain around this area. This happens when a bacteria (for example S. Aureus, 80% of the cases) have passed across the soft tissues from a break in the skin and begins to multiply within the bursa. [2] When a bursa is infected it can probably cause pain, fever, tenderness and an elevated amount of white blood cells.
- Co-existing inflammatory disease- rheumatoid arthritis, gout etc.
Characteristics/Clinical Presentation[edit | edit source]
- Pain
- Swelling[5]
- Differential warmth around the knee
- Painful and limited ROM at the knee
- If bursitis is caused by an infection, pain is associated with fever and chills.
Differential Diagnosis[edit | edit source]
Prepatellar bursitis is often confused with other causes of knee pain including: [6]
- Medial Collateral Ligament Injury
- Lateral Collateral Ligament Injury
- Osteoarthritis
- Pes Anserinus bursitis
- Posterior Cruciate Ligament Injury
- Rheumatoid Arthritis
- Patellar tendon rupture
- Chondromalacia patellae
- Patellofemoral pain
Diagnostic Procedures[edit | edit source]
[7]Bursitis can be diagnosed through a detailed history (about the onset of symptoms, the pattern of knee pain and swelling and how the symptoms affect their lifestyle)[8] and a physical examination, however, X-ray, MRI and CT-scan can be done to rule out the possibility of a fracture or soft tissue injury. If it is uncertain whether or not the bursa is infected, an arthrocentesis can be done. It is typically done for three reasons: necessary information is needed to make a diagnose, to relieve the pressure in the joint and will help alleviate the pain and excess fluid also needs to be removed before a therapeutic injection is given. [9]
Outcome Measures[edit | edit source]
- Visual Analogue Scale
- KOOS Questionnaire: consists of 5 subscales (Pain, other Symptoms, Function in daily living ADL, Function in sport and recreation and knee-related quality of life). Each question gets a score from 0 to 4 and a normalized score is calculated for each subscale (100 = no symptoms and 0 = extreme symptoms). [10]
- Anterior Knee Pain Scale: to measure the functions[11]
Physical Examination[edit | edit source]
Physical examination involves checking for:
- Differential warmth around the knee
- Erythema
- Tenderness
- Swelling
- Pain
- Range of motion
When there is a limited range of motion or swells, a doctor may recommend using a needle and syringe to remove the fluid from the joint. This fluid can be send to labs for testing whether or not the bursa is infected. Common tests for infection are gram stain, white blood cell count (an elevated number of white blood cells in the synovial fluid indicates infection) and glucose levels tests (when the levels are significantly lower than normal it may indicate an infection). Gram stain is used to determine if there are certain troublesome bacteria present. Not all bacteria’s can be identified. Even when the test comes back negative, septic bursitis cannot be completely ruled out. [9]
Medical Management[edit | edit source]
The treatment for prepatellar bursitis depends primarily on the cause of the bursitis and secondarily on the pathological changes in the bursa.[12] The primary goal of treatment is to control the inflammation.
- Conservatively, the R.I.C.E regime [1] in the first 72 hours after the injury or when the first signs of inflammation appear.
- Medications including non-steroidal anti-inflammatory drugs, topical medications- creams, sprays, gels and patches can provide pain relief when those are directly applied to the skin over the knee. To reduce the gastrointestinal side effects that can be caused by oral medications, topical medications may be a good choice. Also, for cases of septic prepatellar bursitis, antibiotics are used to treat the infection.
- Corticosteroid injections
Surgical Management[edit | edit source]
When conservative treatments have failed for chronic/post-traumatic prepatellar bursitis, outpatient arthroscopic bursectomy under local anaesthesia is an effective procedure. Arthroscopic or endoscopic excision of the bursa has more recently been reported to have satisfactory results with less trauma than open excision.[13][14]
Operative Technique[edit | edit source]
The patients are placed in a supine position and the tourniquet will be routinely applied on the thigh and not inflated until necessary. The skin will be prepared in an aseptic manner over the whole lower extremity. A solution will be infiltrated at the portal site and into the cavity, respectively a 1% xylocaine solution with a 1:100,000 epinephrine. For monitoring a 2.7-mm, 30-degree endoscope will be used and a 2.7-motorised shaver to remove thickened synovium. Two or three 2mm portals will be made; an anterior medial portal and anterior lateral portal are routinely used and if necessary a superior lateral portal. To make a 2mm incision for each portal, a no. 11 scalpel will be used. After this, the trochar will be inserted into the cavity and the other instruments will follow. The bursa cavity and synovial thickening are directly visible by the endoscopy. The motorized shaver inserts through the other portal and total synovectomy including the bursa will be performed until all the pathological lesions are removed. When all the procedures are completed, the portals will be closed with adhesive tape without any suture. The anterior knee area is dressed with loosely unfolded gauze, padding and bandage are applied. [1]
Physical Therapy Management[edit | edit source]
The Rest, Ice, Compression and Elevation method[15] (level of evidence 2a) is commonly used treatment for prepatellar bursitis. The ‘rest-phase’ consists of a short period of immobilization. This period should be limited to the first days after the trauma. Resting will reduce the metabolic demands of the injured tissue and will avoid increased blood flow. The use of ice will cause a decrease of the temperature of the tissues in question, inducing vasoconstriction and a limitation of the bleeding. Also, the pain will decrease because cold will cause increasing threshold levels in the free nerve endings and at synapses. Don’t place the ice too long on your knee (maximum 20 minutes at a time with an interval of 30-60 minutes). The compression will decrease the intramuscular blood flow to the affected area and will also reduce the swelling. At lastly there is the elevation. This ensures that the hydrostatic pressure will decrease and it will also reduce the accumulation of interstitial fluid. This part of the Rice-principle also decreases the pressure in local blood vessels and helps to limit the bleeding. However, the effectiveness of this RICE-method has not been proven in any randomized clinical trial. [16]
Once the initial inflammation has reduced a program of stretching and light strengthening will be initiated to restore full motion and improve strength to reduce stress on the tendons and knee joint. Therapeutic exercises to strengthen and stretch the muscles of the knee. This includes static contraction of the quadriceps[17]. This should be an exercise that the patient can do at home 1 to 3 times a day. The objective of the rehabilitation is that the patient can resume their everyday activities. To see if the exercise is working you have to put your fingers on the inner side of the quadriceps, you will feel the muscle tighten during the contraction of the muscle. The patient has to hold his contraction for 5 seconds; the exercise can be repeated 10 times as hard as possible. It is important not to forget this exercise must be pain-free.
Also, the stretching of the quadriceps is a good exercise for the patient, it reduces the friction between the skin and the patella tendon. There is less friction when the patella tendon is more flexible. The physiotherapist can also help the patient by using electrotherapy modalities and patient education on the use of knee pads for kneeling activities.
Prevention[edit | edit source]
In order to prevent prepatellar bursitis you should avoid injury or an overload of your muscles. It is very important to do an appropriate warm-up and cool down, while playing sports. For example, if you play volleyball, it is advisable to wear knee pads. This will prevent falling on the kneecap. Also when you spent a lot of time on your knees is it advisable to wear knee pads. Another important thing to avoid prepatellar bursitis is to check if the flexibility of the knee and the strength and endurance of the leg muscles stays optimal. [2]
Key Research[edit | edit source]
- Yu-Chih H, et al. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011; 35(3): 355–358.(2)
- Hurkmans E.J., et al. KNGF-guideline for Physical Therapy in patients with rheumatoid arthritis. 2008; 118 (5): 13-16.(1)
- Infectious olecranon and patellar bursitis: short-course adjuvant antibiotic therapy is not a risk factor for recurrence in adult hospitalized patients http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=2&colname=WOS
- Cloxacillin-based therapy in severe septic bursitis: Retrospective study of 82 cases http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=3&colname=WOS
- Ossifying Bursitis Praepatellaris of the Knee Joint http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=4&colname=WOS
- Hemorrhagic prepatellar bursitis: a rare case report and review of the literature http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=8&colname=WOS
- Prepatellar Septic Bursitis: A Case Report of Skin Necrosis Associated With Open Bursectomy http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=7&colname=WOS
- Olecranon and prepatellar bursitis - Treating acute, chronic, and inflamed http://apps.isiknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=S24LCBd8ahiI4bB3hJ7&page=1&doc=30&colname=WOS
Resources[edit | edit source]
• http://www.drlox.com/knee-pain-v2/knee-bursitis/
• http://www.houstonmethodist.org/orthopedics/where-does-it-hurt/knee/prepatellar-bursitis
• http://www.arthritis-health.com/types/bursitis/knee-prepatellar-bursitis
Clinical Bottom Line[edit | edit source]
The prepatellar bursa is located under the skin and occurs in most people. When a bursa is inflamed, it's called bursitis. The inflammation can be of an infectious nature or a non-infectious nature. Many different aetiologies have been proposed as the cause of prepatellar bursitis. Chronic inflammation of prepatellar bursa after repetitive minor trauma is called ‘housemaid’s knee’. It can be seen in those who have to kneel very often, such as carpet layers and housemaids. Also a fall directly on the patella, an acute trauma, may cause patellar bursitis. Treatment for prepatellar bursitis depends primarily on the cause of bursitis and secondarily on the pathological change in the bursa. A surgical procedure is in most cases not required, but if needed, the surgical procedures involved are (1) aspiration and irrigation with a suitable drug, (2) incision and drainage in cases of acute suppurative bursitis, and (3) excision of chronically infected and thickened bursa. [1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Yu-Chih H, et al. Endoscopic treatment of prepatellar bursitis. Int Orthop 2011; 35(3): 355–358. (2)
- ↑ 2.0 2.1 2.2 Mcafee J.H. et al.. Olecranon and prepatellar bursitis: diagnosis and treatment. West Journal Medecine, 1988; 149: 607-610.
- ↑ Le Manac’h A.P. et al. Prevalence of knee bursitis in de workforce. Occupational medecine 2012; 62: 658-660
- ↑ Baumbach, S.F., et al. Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Archives of Orthopaedic and Trauma Surgery 2014; 134: 359.
- ↑ Rennie, WJ, Saifuddin, A. Pes anserine bursitis: incidence in symptomatic knees and clinical presentation. Skeletal Radiol 2005; 34:395.
- ↑ Cutbill JW et al., Anterior knee pain: a review. Clin J Sports Med 1997; 7:40-45
- ↑ van Everdingen, J.J.E. Diagnose en therapie. Bohn, Springer Uitgeverij, 2010, 943 pagina’s. (5)
- ↑ Housten Methodist, eOrthopod Medical Multimedia Group L.L.C. Prepatellar bursitis: A patient’s guide to prepatellar bursitis. http://www.houstonmethodist.org/orthopedics/where-does-it-hurt/knee/prepatellar-bursitis (accessed 5 November 2016). (5)
- ↑ 9.0 9.1 Dean Cole., J. MD, (2013), Knee (prepatellar) bursitis. http://www.arthritis-health.com/types/bursitis/knee-prepatellar-bursitis (accessed 5 November 2016). (5)
- ↑ Peer M.A. et al., The Knee Injury and osteoarthritis Outcome Score (KOOS): A Review of its Psychometric Properties in People Undergoing Total Knee Arthroplasty. Journal of Orthopaedic and Sports Physicial Therapy 2013; (4057), 43 .
- ↑ Panken AM. et al. Clinical Prognostic factors for patients with anterior knee pain in physical therapy: systematic review. int J sports Phys ther 2015; 929-945.
- ↑ Crenshaw AH. Campbells’s operative orthopaedics. St Louis: Mosby; 1992.
- ↑ Huang YC, Yeh WL. Endoscopic treatment of prepatellar bursitis. Int Orthop. 2011 Mar. 35(3):355-8.
- ↑ Gendernalik JD, Sechriest VF 2nd. Prepatellar septic bursitis: a case report of skin necrosis associated with open bursectomy. Mil Med. 2009 Jun. 174(6):666-9.
- ↑ Michel P.J, et al., What Is the Evidence for Rest, Ice, Compression, and Elevation Therapy in the Treatment of Ankle Sprains in Adults?. Journal of Athletic Training 2012; 47(4): 435-443. (2)
- ↑ Baoge L., et al. Treatment of Skeletal Muscle Injury: A Review. ISRN Orthop. 2012.(5)
- ↑ SIP, W. Kracht- en stabiliteitstraining. BOSU, 2010. (5)