Postural Principles Useful to Consider in Voice Production: Difference between revisions
(Created page with "Introduction Various healthcare disciplines may have a quite different approach to posture. Physiotherapists and other rehabilitation professionals consider overall body posit...") |
No edit summary |
||
| (48 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
Introduction | <div class="editorbox"> '''Original Editor '''- [https://members.physio-pedia.com/course_tutor/mauro-banfi/ Mauro Banfi] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
The relationship between posture and vocal quality is well known.<ref name=":10">Caçador M, Paço J. [https://www.gazetamedica.pt/index.php/gazeta/article/view/159 The influence of posture and balance on voice: a review: A influência da postura e do equilíbrio na voz: revisão]. Gaz Med [Internet]. 2018;5(2). </ref> Changes in posture can affect vocal performance and, similarly, changes to the voice production mechanism affect posture.<ref name=":10" /> Individuals with dysphonia (i.e. a difficulty or change in voice production<ref name=":11">Cardoso R, Lumini-Oliveira J, Meneses RF. [https://www.researchgate.net/publication/330293214_Associations_between_posture_voice_and_dysphonia_A_systematic_review Associations between posture, voice, and dysphonia: a systematic review]. J Voice. 2019 Jan;33(1):124.e1-124.e12. </ref>) may present with certain postural dysfunctions such as increased tension of their anterior muscular peri-laryngeal chain.<ref name=":1" /> These postural dysfunctions can, however, be improved with vocal rehabilitation.<ref name=":10" /> | |||
[[File:Complimentary techniques used by singers.jpg|thumb|Figure 1. Complementary Techniques Used by Singers|alt=]] | |||
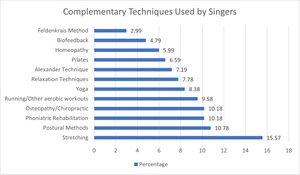
In a recent survey, singers from various disciplines (i.e. classical, pop etc.) were asked which complementary techniques they preferred to specifically address musculoskeletal dysfunctions. Many responded that they tended to choose interventions that focus on the body (see Figure 1), such as:<ref name=":1" /> | |||
* Stretching | |||
* Manual therapy | |||
* Re-education | |||
* Osteopathy / chiropractic care etc. | |||
This page, therefore, explores in detail specific postural approaches that may be useful for speech therapists and physiotherapists working in the performing arts. | |||
== Posture == | |||
<blockquote>“Posture is the position of the body in space, and [it] is controlled by a set of anatomical structures”<ref name=":0">Carini F, Mazzola M, Fici C, Palmeri S, Messina M, Damiani P et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166197/ Posture and posturology, anatomical and physiological profiles: overview and current state of art]. Acta Biomed. 2017;88(1):11-16.</ref></blockquote>Human posture refers to the relationship between body parts (e.g. head and neck, trunk, upper and lower limbs) in an upright position. Posture encompasses:<ref name=":0" /> | |||
* Position | |||
* Body shape | |||
* Neuromuscular mode of operation | |||
* Static and dynamic balance | |||
Considering these concepts separately can lead to therapeutic failures and misunderstandings between different healthcare professionals.<ref name=":1" /> | |||
There are three recognized reference planes when assessing posture:<ref name=":1">Banfi M. Introduction to Postural Principles for Speech Therapists and Physiotherapists. Plus. 2021.</ref> | |||
* Sagittal | |||
* Coronal | |||
* Transverse | |||
[[File:Spinal column curvature 2011.png|thumb|Figure 2. Physiological Spinal Curve|alt=|420x420px]] | |||
There are also three physiological curves that act to balance the human spine (see Figure 2):<ref name=":0" /> | |||
* Cervical lordosis | |||
* Thoracic kyphosis | |||
* Lumbar lordosis | |||
These curves form and stabilise once there is proprioceptive maturation of the foot, which occurs at around the age of 5 or 6 years.<ref name=":0" /> They help to:<ref name=":0" /> | |||
* Maintain balance | |||
* Provide support and resistance against longitudinal pressures | |||
=== "Good Posture" === | |||
As quoted in Czaprowski et al., Kendall and colleagues define "good posture" as:<blockquote>“That state of muscular and skeletal balance which protects the supporting structures of the body against the injury or progressive deformity, irrespective of the attitude (erect, lying, squatting or stooping) in which these structures are working or resting. Under such conditions, the muscles will function most efficiently, and the optimum positions are afforded for the thoracic and abdominal organs.”<ref name=":2">Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836359/#CR3 Non-structural misalignments of body posture in the sagittal plane]. ''Scoliosis Spinal Disord''. 2018;13:6.</ref></blockquote>Good posture is proposed to have certain benefits:<ref name=":2" /> | |||
* Enables effective movement | |||
* Supports the function of the internal organs | |||
* Ergonomic advantages while standing | |||
{{#ev:youtube|OyK0oE5rwFY}}<ref>TED-Ed. The benefits of good posture - Murat Dalkilinç. Available from: https://www.youtube.com/watch?v=OyK0oE5rwFY [last accessed 2/6/2021]</ref> | |||
[[File:Big Stock Image - Lateral Posture - ID348094975.jpg|thumb|400x400px|Figure 3. Lateral view. ]] | |||
The following alignment is considered ideal when observed from a lateral view (see Figure 3): | |||
* The head line begins at the external auditory meatus. It runs:<ref name=":2" /> | |||
** Vertically through the acromion, the lumbar vertebral bodies, and the promontory | |||
** Slightly posteriorly to the hip joint axis | |||
** Slightly anterior to the knee joint axis | |||
** And terminates at, or slightly anterior, to the lateral malleolus | |||
* Other points of reference: <ref name=":1" /> | |||
** The line of gravity should pass just anteriorly to the ear and C3 – C4, tangent to L3 - L4, cross the tibial plate and project centrally to the support polygon (i.e. slightly anterior to the line that connects the tibiotarsal joints) | |||
** Cervical lordosis should be around 60 mm | |||
** Dorsal kyphosis should be aligned with the gluteal muscles | |||
** Lumbar lordosis should be around 40mm | |||
[[File:Big Stock Image - Anterior Posture - ID348094975.jpg|thumb|350x350px|Figure 4. Frontal view. ]] | |||
From the frontal view, the flowing lines should be parallel and horizontal (see Figure 4):<ref name=":1" /> | |||
* Bi-pupilar line | |||
* Bi-condylar line | |||
* Bi-mammillary line | |||
* Bi-styloid line | |||
* Bi-iliac line | |||
* Bi-patellar line | |||
* Bi-malleolar line | |||
While few people adopt an ideal posture, it can be beneficial to observe the posture of clients with vocal or swallowing problems to detect any postural anomalies that may be contributing to their complaints.<ref name=":1" /> When considering the relationship with speech therapy in particular, it is important to remember that:<ref name=":1" /> | |||
* The neck, like the trunk, has many interdependent structures / viscera | |||
* The vocal system is intricately linked to all structures in the neck and skull, as well as the anatomical structures that underlie phonation and swallowing (e.g. the diaphragm, viscera) | |||
== Relationship Between Posture and Voice == | |||
A recent review by Cardoso and colleagues found specific associations between posture, voice and dysphonia, including:<ref name=":11" /> | |||
* Postural imbalances in the head and neck can lead to changes in the soft tissue of the pharynx and muscles that raise the larynx - this affects vocal control and resonance | |||
* The position of the cervical spine changes based on humming pitch - as an individual changes pitch from low to high, his / her cervical spine moves from lordosis to kyphosis, which means the airway becomes shorter. Other changes include: | |||
** Increased distance between the sternum and larynx | |||
** Decreased distance between the larynx and hyoid bone | |||
* A significant increase in tension in the extrinsic or (para)laryngeal muscles is associated with muscle tension dysphonia. This increased tension causes the larynx to elevate | |||
* Vocal quality decreases with forward head, backward head, and cervical extension positions when compared to a straight / neutral position | |||
* A backward head position and cervical extension is associated with increased volume | |||
* Posture can affect vocal effort - even small changes in head position / balance can significantly affect the efficacy of laryngeal movement | |||
== Approaches to Posture == | |||
The three most commonly used approaches to posture are:<ref name=":1" /> | |||
* Posturology | |||
* Global postural re-education | |||
* Osteopathy and manual therapy | |||
== Posturology == | |||
Posturology is the study of posture.<ref name=":0" /> It is an interdisciplinary method that evaluates the activity of postural control systems (e.g. the postural tonic system). It is measured in an upright position, in normalised situations, through specific evaluation tests.<ref name=":1" /> | |||
== The Fine Postural System == | |||
<blockquote>“The fine postural system (FPS) aims to maintain balance in the most economical way possible.”<ref>Milkov M, Stoykov M, Tsvetkova A, Petrova D. [https://journals.mu-varna.bg/index.php/orl/article/view/7734 Important relationships between posturology, vestibular disorders and dental medicine]. Laryngorhinootologie. 2021;100(S 02):S233-S234.</ref></blockquote>Postural receptors are found throughout the human body. They contribute to the creation of the body schema and conscious control of the postural state.<ref name=":1" /> There are three types:<ref name=":4">Marzvanyan A, Alhawaj AF. Physiology, Sensory Receptors. [Updated 2020 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539861/ </ref> | |||
# Exteroceptors: detect information about the world around us. Examples include: | |||
#* The retina - sight information | |||
#* Plantar receptors - touch information from the foot | |||
#* Inner ear - sound information | |||
# Interoceptors: detect information about the condition of our body from internal organs and processes.<ref name=":1" /> | |||
# Proprioceptors: detect information about body position and load.<ref name=":4" /> Examples include:<ref name=":1" /> | |||
#* Tendon organs | |||
#* Joint receptors | |||
#* Neuromuscular spindles | |||
#* Stomatognathic system | |||
{{#ev:youtube|AG7Ev2hJGFk}}<ref>Dr Matt & Dr Mike. Types of Sensory Receptors. Available from: https://www.youtube.com/watch?v=AG7Ev2hJGFk [last accessed 2/6/2021]</ref> | |||
=== Centres of Postural Control === | |||
All data collected by sensory receptors is received by [[The Postural Control System|postural control centres]] in the central nervous system. The upper centres are:<ref name=":1" /> | |||
* Spinoreticular centres | |||
* Vestibular nuclei | |||
* Basal nuclei | |||
* Precortical nuclei | |||
* Cerebellum | |||
* Cerebral cortex | |||
These structures interpret postural information and, accordingly, induce changes in our musculoskeletal system to ensure we can maintain the position of our body.<ref name=":1" /> | |||
=== Fine Postural Control === | |||
Standing upright is an inherently unstable,<ref>Peterka RJ. [https://journals.physiology.org/doi/full/10.1152/jn.2002.88.3.1097 Sensorimotor integration in human postural control]. J Neurophysiol. 2002;88(3):1097-118. </ref> dynamic activity<ref name=":5">Koltermann JJ, Beck H, Beck M. [https://www.mdpi.com/2076-3417/10/11/3741/htm Investigation of the correlation between factors influencing the spectrum of center of pressure measurements using dynamic controlled models of the upright stand and subject measurements]. Applied Sciences. 2020; 10(11):3741.</ref> - there will always be some motion even when an individual is standing still (i.e. body sway / oscillations). These oscillations are very small - around 0-4 degrees<ref name=":1" /> or 1-2 cm.<ref name=":3">Ivanenko Y, Gurfinkel VS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5869197/ Human postural control]. ''Front Neurosci''. 2018;12:171. </ref> In order to maintain balance, the central nervous system mediates changes in postural muscle tone.<ref name=":1" /> | |||
Postural tone is defined as:<blockquote>“the steady contraction of muscles that are necessary to hold different parts of the skeleton in proper relation to the various and constantly changing attitudes and postures of the body.”<ref>Gurfinkel VS. Postural muscle tone. In: Binder MD, Hirokawa N, Windhorst U. Editors. Encyclopedia of neuroscience. Berlin, Heidelberg: Springer, 2009.</ref></blockquote>Postural muscle tone is adjusted in response to the information provided by postural receptors. Information provided by the exteroceptors (like vision) is typically prioritised.<ref name=":1" /> | |||
=== Models of Postural Control === | |||
Various models have been proposed to explain postural control including the inverted pendulum and triple inverted pendulum models. | |||
==== Inverted Pendulum Model of Upright Posture ==== | |||
In the inverted pendulum model of upright posture, the human body is perceived as a rigid segment with the centre of mass (CoM) positioned about one metre above a point slightly anterior to the ankle.<ref>Pinter IJ, van Swigchem R, van Soest AJ, Rozendaal LA. [https://journals.physiology.org/doi/full/10.1152/jn.01312.2007 The dynamics of postural sway cannot be captured using a one-segment inverted pendulum model: a PCA on segment rotations during unperturbed stance]. J Neurophysiol. 2008;100(6):3197-208. </ref> | |||
In this model, the CoM is the sole controlled variable. In quiet standing, the centre of pressure (CoP) oscillates either side of the CoM to maintain a fairly consistent position between the feet.<ref name=":3" /> The natural frequency of the human body when oscillating around the ankle axis is between 0.2 and 0.3 Hz.<ref name=":5" /> | |||
However, there are various problems with this model:<ref name=":5" /> | |||
* The amplitude of the oscillation and the occurring frequency are independent of size and weight | |||
* Movements of the head can be assumed to be similar to those of the hip | |||
* The knees and hips are not static | |||
==== Triple Pendulum Model of Upright Posture ==== | |||
Thus, other models have been proposed including the inverted triple pendulum model. This model is considered more realistic as it considers movement at the hip, knee and ankle.<ref name=":1" /> | |||
The following video discusses these models (from 23 minutes onwards). *Optional | |||
{{#ev:youtube|hYqukY1BB2E}}<ref>Steven Harrison. DPT 5432 - Posture - Video 1. Available from: https://www.youtube.com/watch?v=hYqukY1BB2E [last accessed 2/6/2021]</ref> | |||
=== Diagnostic Techniques === | |||
==== Stabilometry ==== | |||
The main diagnostic technique used in posturology is stabilometry.<ref name=":0" /> Stabilometry is defined as: <blockquote>“the objective study of body sway during quiet standing, i.e., stance in the absence of any voluntary movements or external perturbations.”<ref name=":6">Chiari L. Stabilometry. In: Binder MD, Hirokawa N, Windhorst U. Editors. Encyclopedia of neuroscience. 2009. Berlin, Heidelberg: Springer, 2009.</ref></blockquote>It usually focuses on upright standing, but it can also be used to assess sitting. It provides information about the:<ref name=":6" /> | |||
* Steady-state functioning of the postural control system | |||
* Ability of the system to stabilise the body against gravity | |||
It looks at various parameters including:<ref name=":1" /> | |||
* Oscillation amplitude | |||
* Prevailing oscillation axes | |||
* Length and oscillation rate etc. | |||
==== Baropodometry ==== | |||
Baropodometry is an advanced force platform that is used to measure the distribution of load through the feet at rest and when walking.<ref name=":7">Baumfeld D, Baumfeld T, da Rocha RL, Macedo B, Raduan F, Zambelli R et al. [https://www.hindawi.com/journals/bmri/2017/5925137/ Reliability of baropodometry on the evaluation of plantar load distribution: A transversal study]. Biomed Res Int. 2017;2017:5925137. </ref> | |||
It provides information about:<ref name=":7" /> | |||
* The patient’s position in standing | |||
* Dynamic gait | |||
* Load distribution while walking | |||
* Peak pressure and ground contact time | |||
* Biomechanical abnormalities of the foot, spine and pelvis | |||
=== Posturology Syndromes === | |||
After assessing the client, it is possible to diagnose two specific syndromes in posturology:<ref name=":1" /> | |||
# Ascending Syndrome | |||
#* Perturbations are given by the podalic (i.e. foot) support system. Thus, the lower limb has an impact further up the kinetic chain, altering the amount of oscillation in order to maintain a state of equilibrium | |||
# Descending Syndrome | |||
#* Input from the mouth, skull and eye alter the neutral state of the body | |||
These conditions are discussed in more detail [[Postural Principles Useful in Speech Therapy - Part 2|here]]. | |||
=== Aim of Posturology === | |||
The aim of posturology is essentially to reprogramme the system and create balance. For example, muscle chains that are balanced with equal tone (right and left) are able to work effectively and will not overload muscular or structural systems. This enables the patient to stay in an upright position.<ref name=":1" /> | |||
=== Posturology Techniques === | |||
Different inputs can be introduced to affect postural change, particularly using the exteroceptors. Examples include:<ref name=":1" /> | |||
* Changes at the level of the podalic receptors using shoe insoles | |||
* Changes at the eye using [https://www.optometrists.org/vision-therapy/neuro-optometry/what-are-prism-lenses/ prism glasses] | |||
* Changes at the mandible with occlusal corrections | |||
It is also possible to apply manual techniques to the proprioceptors.<ref name=":1" /> | |||
== Global Postural Re-Education == | |||
Global postural re-education (GPR) is a method of postural correction that was first developed by a French physiotherapist, Philippe Souchard.<ref name=":8">Dimitrova E. Rohleva M. [https://www.researchgate.net/publication/344489733_GLOBAL_POSTURAL_REEDUCATION_IN_THE_TREATMENT_OF_POSTURAL_IMPAIRMENTS Global postural reeducation in the treatment of postural impairments]. Research in Kinesiology. 2014;4(1):72-5.</ref> There are three key principles of GPR:<ref name=":9">Ferreira GE, Barreto RG, Robinson CC, Plentz RD, Silva MF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4946835/ Global Postural Reeducation for patients with musculoskeletal conditions: a systematic review of randomized controlled trials]. ''Braz J Phys Ther''. 2016;20(3):194-205.</ref> | |||
# Each person / patient is unique | |||
# The underlying cause of a musculoskeletal complaint may originate at a site away from the location of pain | |||
# The body should be treated as a whole | |||
A key feature of GPR is that, like posturology, it focuses on specific muscle chains. The main muscle chains are the posterior static chain and the anterior inspiratory chain (see Table 1 for more detail). It is theorised that musculoskeletal conditions may develop because of retractions in these muscle chains. Each patient is, therefore, treated with static postures that aim to:<ref name=":9" /> | |||
* Stretch shortened muscle chains | |||
* Enhance co-contraction of antagonists | |||
* Ultimately improve postural symmetry (and, thus, reduce pain and disability) | |||
Each stretching session lasts 15 to 20 minutes<ref name=":8" /> and the overall approach includes:<ref name=":1" /> | |||
* Active correction (i.e. therapist assisted) | |||
* Static corrective postures in muscle self-elongation | |||
* Eccentric contractions to strengthen weak muscles | |||
{| class="wikitable" | |||
!Postural chains | |||
!Muscles included | |||
|- | |||
!Anterior postural chains | |||
| | |||
|- | |||
|Inspiratory muscle chain | |||
|Diaphragm, its suspensory apparatus, serratus anterior, scalenes, sternocleidomastoid and pectoralis minor | |||
|- | |||
|Antero-internal chain of the shoulder | |||
|Superficial part of the pectoral muscles, subscapularis, coracobrachialis | |||
|- | |||
|Anterior chain of the arm | |||
|Biceps, brachialis, coracobrachialis, supinator, flexors of the hand, thenar and hypothenar muscles | |||
|- | |||
|Antero-internal chain of the hip | |||
|Iliopsoas, adductors | |||
|- | |||
!Posterior postural chain | |||
|Para-vertebrals, gluteus maximus, external rotators of the hip, hamstrings, popliteus, soleus, plantar muscles | |||
|} | |||
Table 1. Postural Chains<ref name=":1" /> | |||
=== Postural Compensation === | |||
The aim of GPR is to correct any compensations that occur when a patient is attempting to correct his / her posture. Patients must attempt to hold a correction for a number of minutes during inspiration and exhalation.<ref name=":1" /> Breathing is an essential consideration in GPR because alterations in myofascial tension or spinal restriction can cause changes in breathing pattern (and vice versa).<ref>Grossi E. Global Postural Re-Education: Souchard method. Chaitow L, editor. Fascial dysfunction - manual therapy approaches. 2nd Edition. Handspring Publishing Limited. 2018. </ref> Thus, the impact of breath on GPR corrections must be considered.<ref name=":1" /> For the speech therapist, it is important to note that various compensations are possible in the peri-laryngeal zone.<ref name=":1" /> | |||
== Principles of Osteopathy == | |||
The cardinal principles of osteopathy are still based on those defined by Andrew Taylor Still in 1875: <ref name=":1" /> <ref name=":12">Licciardone JC, Schultz MJ, Amen B. [https://www.dovepress.com/osteopathic-manipulation-in-the-management-of-chronic-pain-current-per-peer-reviewed-fulltext-article-JPR Osteopathic manipulation in the management of chronic pain: current perspectives]. J Pain Res. 2020;13:1839-47. </ref> | |||
* Structure governs function | |||
* There is a close inter-relationship between systems - a dysfunction in one system induces compensations in another | |||
* There is an ability to self-regulate the body - if a biomechanical anomaly is normalised, the body itself can restore function | |||
Osteopathic evaluation includes:<ref name=":1" /> | |||
* Observation | |||
* Palpation | |||
* Specific mobility tests to assess restrictions of musculoskeletal, fascial and visceral structures | |||
Corrections rely on passive manipulative techniques.<ref name=":1" /> Manually guided forces are applied with the goal of improving physiological function and to help maintain homeostasis.<ref name=":12" /> | |||
Relevant points for speech therapy:<ref name=":1" /> | |||
* It is important to consider the laryngeal system as a set of structures with specific biomechanics, as well as its relationship to adjacent structures, such as the cervical spine, mandible and thorax | |||
* Osteopathic techniques can be an effective way of achieving myofascial normalisation of the peri-laryngeal muscles and laryngeal structures, such as the hyoid<ref name=":1" /><ref>Amorim CS, Gracitelli ME, Marques AP, Alves VL. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: a preliminary clinical trial. J Manipulative Physiol Ther. 2014;37(6):441-7.</ref> | |||
== Summary == | |||
* Posture and human alignment can have a significant impact on various conditions, including speech and swallowing issues | |||
* Posturology, GPR and osteopathy / manual therapy all consider the relationship of posture, muscle chains and musculoskeletal dysfunction | |||
* Speech-language therapists should consider overall body alignment to determine if any postural anomalies might be affecting their clients' function or performance | |||
== References == | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
<references /> | |||
[[Category:Speech Therapy]] | |||
Latest revision as of 23:48, 18 December 2023
Introduction[edit | edit source]
The relationship between posture and vocal quality is well known.[1] Changes in posture can affect vocal performance and, similarly, changes to the voice production mechanism affect posture.[1] Individuals with dysphonia (i.e. a difficulty or change in voice production[2]) may present with certain postural dysfunctions such as increased tension of their anterior muscular peri-laryngeal chain.[3] These postural dysfunctions can, however, be improved with vocal rehabilitation.[1]
In a recent survey, singers from various disciplines (i.e. classical, pop etc.) were asked which complementary techniques they preferred to specifically address musculoskeletal dysfunctions. Many responded that they tended to choose interventions that focus on the body (see Figure 1), such as:[3]
- Stretching
- Manual therapy
- Re-education
- Osteopathy / chiropractic care etc.
This page, therefore, explores in detail specific postural approaches that may be useful for speech therapists and physiotherapists working in the performing arts.
Posture[edit | edit source]
“Posture is the position of the body in space, and [it] is controlled by a set of anatomical structures”[4]
Human posture refers to the relationship between body parts (e.g. head and neck, trunk, upper and lower limbs) in an upright position. Posture encompasses:[4]
- Position
- Body shape
- Neuromuscular mode of operation
- Static and dynamic balance
Considering these concepts separately can lead to therapeutic failures and misunderstandings between different healthcare professionals.[3]
There are three recognized reference planes when assessing posture:[3]
- Sagittal
- Coronal
- Transverse
There are also three physiological curves that act to balance the human spine (see Figure 2):[4]
- Cervical lordosis
- Thoracic kyphosis
- Lumbar lordosis
These curves form and stabilise once there is proprioceptive maturation of the foot, which occurs at around the age of 5 or 6 years.[4] They help to:[4]
- Maintain balance
- Provide support and resistance against longitudinal pressures
"Good Posture"[edit | edit source]
As quoted in Czaprowski et al., Kendall and colleagues define "good posture" as:
“That state of muscular and skeletal balance which protects the supporting structures of the body against the injury or progressive deformity, irrespective of the attitude (erect, lying, squatting or stooping) in which these structures are working or resting. Under such conditions, the muscles will function most efficiently, and the optimum positions are afforded for the thoracic and abdominal organs.”[5]
Good posture is proposed to have certain benefits:[5]
- Enables effective movement
- Supports the function of the internal organs
- Ergonomic advantages while standing
The following alignment is considered ideal when observed from a lateral view (see Figure 3):
- The head line begins at the external auditory meatus. It runs:[5]
- Vertically through the acromion, the lumbar vertebral bodies, and the promontory
- Slightly posteriorly to the hip joint axis
- Slightly anterior to the knee joint axis
- And terminates at, or slightly anterior, to the lateral malleolus
- Other points of reference: [3]
- The line of gravity should pass just anteriorly to the ear and C3 – C4, tangent to L3 - L4, cross the tibial plate and project centrally to the support polygon (i.e. slightly anterior to the line that connects the tibiotarsal joints)
- Cervical lordosis should be around 60 mm
- Dorsal kyphosis should be aligned with the gluteal muscles
- Lumbar lordosis should be around 40mm
From the frontal view, the flowing lines should be parallel and horizontal (see Figure 4):[3]
- Bi-pupilar line
- Bi-condylar line
- Bi-mammillary line
- Bi-styloid line
- Bi-iliac line
- Bi-patellar line
- Bi-malleolar line
While few people adopt an ideal posture, it can be beneficial to observe the posture of clients with vocal or swallowing problems to detect any postural anomalies that may be contributing to their complaints.[3] When considering the relationship with speech therapy in particular, it is important to remember that:[3]
- The neck, like the trunk, has many interdependent structures / viscera
- The vocal system is intricately linked to all structures in the neck and skull, as well as the anatomical structures that underlie phonation and swallowing (e.g. the diaphragm, viscera)
Relationship Between Posture and Voice[edit | edit source]
A recent review by Cardoso and colleagues found specific associations between posture, voice and dysphonia, including:[2]
- Postural imbalances in the head and neck can lead to changes in the soft tissue of the pharynx and muscles that raise the larynx - this affects vocal control and resonance
- The position of the cervical spine changes based on humming pitch - as an individual changes pitch from low to high, his / her cervical spine moves from lordosis to kyphosis, which means the airway becomes shorter. Other changes include:
- Increased distance between the sternum and larynx
- Decreased distance between the larynx and hyoid bone
- A significant increase in tension in the extrinsic or (para)laryngeal muscles is associated with muscle tension dysphonia. This increased tension causes the larynx to elevate
- Vocal quality decreases with forward head, backward head, and cervical extension positions when compared to a straight / neutral position
- A backward head position and cervical extension is associated with increased volume
- Posture can affect vocal effort - even small changes in head position / balance can significantly affect the efficacy of laryngeal movement
Approaches to Posture[edit | edit source]
The three most commonly used approaches to posture are:[3]
- Posturology
- Global postural re-education
- Osteopathy and manual therapy
Posturology[edit | edit source]
Posturology is the study of posture.[4] It is an interdisciplinary method that evaluates the activity of postural control systems (e.g. the postural tonic system). It is measured in an upright position, in normalised situations, through specific evaluation tests.[3]
The Fine Postural System[edit | edit source]
“The fine postural system (FPS) aims to maintain balance in the most economical way possible.”[7]
Postural receptors are found throughout the human body. They contribute to the creation of the body schema and conscious control of the postural state.[3] There are three types:[8]
- Exteroceptors: detect information about the world around us. Examples include:
- The retina - sight information
- Plantar receptors - touch information from the foot
- Inner ear - sound information
- Interoceptors: detect information about the condition of our body from internal organs and processes.[3]
- Proprioceptors: detect information about body position and load.[8] Examples include:[3]
- Tendon organs
- Joint receptors
- Neuromuscular spindles
- Stomatognathic system
Centres of Postural Control[edit | edit source]
All data collected by sensory receptors is received by postural control centres in the central nervous system. The upper centres are:[3]
- Spinoreticular centres
- Vestibular nuclei
- Basal nuclei
- Precortical nuclei
- Cerebellum
- Cerebral cortex
These structures interpret postural information and, accordingly, induce changes in our musculoskeletal system to ensure we can maintain the position of our body.[3]
Fine Postural Control[edit | edit source]
Standing upright is an inherently unstable,[10] dynamic activity[11] - there will always be some motion even when an individual is standing still (i.e. body sway / oscillations). These oscillations are very small - around 0-4 degrees[3] or 1-2 cm.[12] In order to maintain balance, the central nervous system mediates changes in postural muscle tone.[3]
Postural tone is defined as:
“the steady contraction of muscles that are necessary to hold different parts of the skeleton in proper relation to the various and constantly changing attitudes and postures of the body.”[13]
Postural muscle tone is adjusted in response to the information provided by postural receptors. Information provided by the exteroceptors (like vision) is typically prioritised.[3]
Models of Postural Control[edit | edit source]
Various models have been proposed to explain postural control including the inverted pendulum and triple inverted pendulum models.
Inverted Pendulum Model of Upright Posture[edit | edit source]
In the inverted pendulum model of upright posture, the human body is perceived as a rigid segment with the centre of mass (CoM) positioned about one metre above a point slightly anterior to the ankle.[14]
In this model, the CoM is the sole controlled variable. In quiet standing, the centre of pressure (CoP) oscillates either side of the CoM to maintain a fairly consistent position between the feet.[12] The natural frequency of the human body when oscillating around the ankle axis is between 0.2 and 0.3 Hz.[11]
However, there are various problems with this model:[11]
- The amplitude of the oscillation and the occurring frequency are independent of size and weight
- Movements of the head can be assumed to be similar to those of the hip
- The knees and hips are not static
Triple Pendulum Model of Upright Posture[edit | edit source]
Thus, other models have been proposed including the inverted triple pendulum model. This model is considered more realistic as it considers movement at the hip, knee and ankle.[3]
The following video discusses these models (from 23 minutes onwards). *Optional
Diagnostic Techniques[edit | edit source]
Stabilometry[edit | edit source]
The main diagnostic technique used in posturology is stabilometry.[4] Stabilometry is defined as:
“the objective study of body sway during quiet standing, i.e., stance in the absence of any voluntary movements or external perturbations.”[16]
It usually focuses on upright standing, but it can also be used to assess sitting. It provides information about the:[16]
- Steady-state functioning of the postural control system
- Ability of the system to stabilise the body against gravity
It looks at various parameters including:[3]
- Oscillation amplitude
- Prevailing oscillation axes
- Length and oscillation rate etc.
Baropodometry[edit | edit source]
Baropodometry is an advanced force platform that is used to measure the distribution of load through the feet at rest and when walking.[17]
It provides information about:[17]
- The patient’s position in standing
- Dynamic gait
- Load distribution while walking
- Peak pressure and ground contact time
- Biomechanical abnormalities of the foot, spine and pelvis
Posturology Syndromes[edit | edit source]
After assessing the client, it is possible to diagnose two specific syndromes in posturology:[3]
- Ascending Syndrome
- Perturbations are given by the podalic (i.e. foot) support system. Thus, the lower limb has an impact further up the kinetic chain, altering the amount of oscillation in order to maintain a state of equilibrium
- Descending Syndrome
- Input from the mouth, skull and eye alter the neutral state of the body
These conditions are discussed in more detail here.
Aim of Posturology[edit | edit source]
The aim of posturology is essentially to reprogramme the system and create balance. For example, muscle chains that are balanced with equal tone (right and left) are able to work effectively and will not overload muscular or structural systems. This enables the patient to stay in an upright position.[3]
Posturology Techniques[edit | edit source]
Different inputs can be introduced to affect postural change, particularly using the exteroceptors. Examples include:[3]
- Changes at the level of the podalic receptors using shoe insoles
- Changes at the eye using prism glasses
- Changes at the mandible with occlusal corrections
It is also possible to apply manual techniques to the proprioceptors.[3]
Global Postural Re-Education[edit | edit source]
Global postural re-education (GPR) is a method of postural correction that was first developed by a French physiotherapist, Philippe Souchard.[18] There are three key principles of GPR:[19]
- Each person / patient is unique
- The underlying cause of a musculoskeletal complaint may originate at a site away from the location of pain
- The body should be treated as a whole
A key feature of GPR is that, like posturology, it focuses on specific muscle chains. The main muscle chains are the posterior static chain and the anterior inspiratory chain (see Table 1 for more detail). It is theorised that musculoskeletal conditions may develop because of retractions in these muscle chains. Each patient is, therefore, treated with static postures that aim to:[19]
- Stretch shortened muscle chains
- Enhance co-contraction of antagonists
- Ultimately improve postural symmetry (and, thus, reduce pain and disability)
Each stretching session lasts 15 to 20 minutes[18] and the overall approach includes:[3]
- Active correction (i.e. therapist assisted)
- Static corrective postures in muscle self-elongation
- Eccentric contractions to strengthen weak muscles
| Postural chains | Muscles included |
|---|---|
| Anterior postural chains | |
| Inspiratory muscle chain | Diaphragm, its suspensory apparatus, serratus anterior, scalenes, sternocleidomastoid and pectoralis minor |
| Antero-internal chain of the shoulder | Superficial part of the pectoral muscles, subscapularis, coracobrachialis |
| Anterior chain of the arm | Biceps, brachialis, coracobrachialis, supinator, flexors of the hand, thenar and hypothenar muscles |
| Antero-internal chain of the hip | Iliopsoas, adductors |
| Posterior postural chain | Para-vertebrals, gluteus maximus, external rotators of the hip, hamstrings, popliteus, soleus, plantar muscles |
Table 1. Postural Chains[3]
Postural Compensation[edit | edit source]
The aim of GPR is to correct any compensations that occur when a patient is attempting to correct his / her posture. Patients must attempt to hold a correction for a number of minutes during inspiration and exhalation.[3] Breathing is an essential consideration in GPR because alterations in myofascial tension or spinal restriction can cause changes in breathing pattern (and vice versa).[20] Thus, the impact of breath on GPR corrections must be considered.[3] For the speech therapist, it is important to note that various compensations are possible in the peri-laryngeal zone.[3]
Principles of Osteopathy[edit | edit source]
The cardinal principles of osteopathy are still based on those defined by Andrew Taylor Still in 1875: [3] [21]
- Structure governs function
- There is a close inter-relationship between systems - a dysfunction in one system induces compensations in another
- There is an ability to self-regulate the body - if a biomechanical anomaly is normalised, the body itself can restore function
Osteopathic evaluation includes:[3]
- Observation
- Palpation
- Specific mobility tests to assess restrictions of musculoskeletal, fascial and visceral structures
Corrections rely on passive manipulative techniques.[3] Manually guided forces are applied with the goal of improving physiological function and to help maintain homeostasis.[21]
Relevant points for speech therapy:[3]
- It is important to consider the laryngeal system as a set of structures with specific biomechanics, as well as its relationship to adjacent structures, such as the cervical spine, mandible and thorax
- Osteopathic techniques can be an effective way of achieving myofascial normalisation of the peri-laryngeal muscles and laryngeal structures, such as the hyoid[3][22]
Summary[edit | edit source]
- Posture and human alignment can have a significant impact on various conditions, including speech and swallowing issues
- Posturology, GPR and osteopathy / manual therapy all consider the relationship of posture, muscle chains and musculoskeletal dysfunction
- Speech-language therapists should consider overall body alignment to determine if any postural anomalies might be affecting their clients' function or performance
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Caçador M, Paço J. The influence of posture and balance on voice: a review: A influência da postura e do equilíbrio na voz: revisão. Gaz Med [Internet]. 2018;5(2).
- ↑ 2.0 2.1 Cardoso R, Lumini-Oliveira J, Meneses RF. Associations between posture, voice, and dysphonia: a systematic review. J Voice. 2019 Jan;33(1):124.e1-124.e12.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 3.28 3.29 3.30 3.31 3.32 3.33 Banfi M. Introduction to Postural Principles for Speech Therapists and Physiotherapists. Plus. 2021.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Carini F, Mazzola M, Fici C, Palmeri S, Messina M, Damiani P et al. Posture and posturology, anatomical and physiological profiles: overview and current state of art. Acta Biomed. 2017;88(1):11-16.
- ↑ 5.0 5.1 5.2 Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13:6.
- ↑ TED-Ed. The benefits of good posture - Murat Dalkilinç. Available from: https://www.youtube.com/watch?v=OyK0oE5rwFY [last accessed 2/6/2021]
- ↑ Milkov M, Stoykov M, Tsvetkova A, Petrova D. Important relationships between posturology, vestibular disorders and dental medicine. Laryngorhinootologie. 2021;100(S 02):S233-S234.
- ↑ 8.0 8.1 Marzvanyan A, Alhawaj AF. Physiology, Sensory Receptors. [Updated 2020 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539861/
- ↑ Dr Matt & Dr Mike. Types of Sensory Receptors. Available from: https://www.youtube.com/watch?v=AG7Ev2hJGFk [last accessed 2/6/2021]
- ↑ Peterka RJ. Sensorimotor integration in human postural control. J Neurophysiol. 2002;88(3):1097-118.
- ↑ 11.0 11.1 11.2 Koltermann JJ, Beck H, Beck M. Investigation of the correlation between factors influencing the spectrum of center of pressure measurements using dynamic controlled models of the upright stand and subject measurements. Applied Sciences. 2020; 10(11):3741.
- ↑ 12.0 12.1 Ivanenko Y, Gurfinkel VS. Human postural control. Front Neurosci. 2018;12:171.
- ↑ Gurfinkel VS. Postural muscle tone. In: Binder MD, Hirokawa N, Windhorst U. Editors. Encyclopedia of neuroscience. Berlin, Heidelberg: Springer, 2009.
- ↑ Pinter IJ, van Swigchem R, van Soest AJ, Rozendaal LA. The dynamics of postural sway cannot be captured using a one-segment inverted pendulum model: a PCA on segment rotations during unperturbed stance. J Neurophysiol. 2008;100(6):3197-208.
- ↑ Steven Harrison. DPT 5432 - Posture - Video 1. Available from: https://www.youtube.com/watch?v=hYqukY1BB2E [last accessed 2/6/2021]
- ↑ 16.0 16.1 Chiari L. Stabilometry. In: Binder MD, Hirokawa N, Windhorst U. Editors. Encyclopedia of neuroscience. 2009. Berlin, Heidelberg: Springer, 2009.
- ↑ 17.0 17.1 Baumfeld D, Baumfeld T, da Rocha RL, Macedo B, Raduan F, Zambelli R et al. Reliability of baropodometry on the evaluation of plantar load distribution: A transversal study. Biomed Res Int. 2017;2017:5925137.
- ↑ 18.0 18.1 Dimitrova E. Rohleva M. Global postural reeducation in the treatment of postural impairments. Research in Kinesiology. 2014;4(1):72-5.
- ↑ 19.0 19.1 Ferreira GE, Barreto RG, Robinson CC, Plentz RD, Silva MF. Global Postural Reeducation for patients with musculoskeletal conditions: a systematic review of randomized controlled trials. Braz J Phys Ther. 2016;20(3):194-205.
- ↑ Grossi E. Global Postural Re-Education: Souchard method. Chaitow L, editor. Fascial dysfunction - manual therapy approaches. 2nd Edition. Handspring Publishing Limited. 2018.
- ↑ 21.0 21.1 Licciardone JC, Schultz MJ, Amen B. Osteopathic manipulation in the management of chronic pain: current perspectives. J Pain Res. 2020;13:1839-47.
- ↑ Amorim CS, Gracitelli ME, Marques AP, Alves VL. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: a preliminary clinical trial. J Manipulative Physiol Ther. 2014;37(6):441-7.