Postural Changes Affecting Voice Production
Introduction[edit | edit source]
There are a number of common postural changes that can affect function, pain and disability levels and voice production.
In older adults, the following postural features are commonly observed:[1]
- Increased thoracic kyphosis
- Reduction in intervertebral disc height
- Loss of bone mass
- Forward head position (i.e. anteposition)
- Retraction of muscle chains
- Reduced elasticity and strength
- Cartilage ossification in the larynx
These postural changes can have a significant impact on speech and swallowing function.[1] Examples include:
- Lordosis of the cervical spine inhibits laryngeal elevation and affects swallowing - postural rehabilitation may be beneficial to manage this[2]
- Ossification of the anterior longitudinal ligament can lead to dysphagia - the extent of which is influenced by the thickness of osteophytes, cervical mobility, and cranio-cervical alignment[3]
When specific postural abnormalities are detected, it is important to determine if the client’s posture can be corrected, or if the postural condition is fixed.
Structured Posture[edit | edit source]
Structured posture describes postural disorders where there are underlying morphological abnormalities in the bone / soft tissues. Examples of a structured posture are:[4]
- Idiopathic scoliosis
- Scheuermann juvenile kyphosis
- Congenital vertebral malformation
- Sequels of spine osteomyelitis
- Spondylolisthesis
These conditions are more clinically significant as they are less flexible and can only be modified with difficulty.[1] They require a specific diagnosis and management.[4]
Non-Structured Posture[edit | edit source]
A non-structured posture is modifiable with the help of the therapist.[1] Individuals with non-structured postures may have similar clinical features as those with structural abnormalities.[4] For instance, scheuermann's disease is often mistaken for adolescent postural kyphosis, so it is necessary to differentiate the two conditions based on the physical examination and radiographic analysis.[5]
Antalgic Posture[edit | edit source]
Antalgic postures are technically modifiable but, if corrected, the patient complains of pain.[1]
Compensatory Posture[edit | edit source]
Compensatory postures can be actively and passively corrected, but the patient does not tend to stay in the corrected position. NB If the cause of the compensation is not treated, the postural destabilisation will return in time.[1]
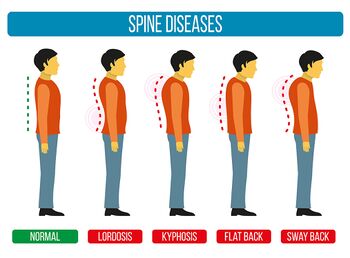
When observing patients, it is important to compare the patient's posture with "normal" posture.
Common Non-Structural Postures[edit | edit source]
Side View[edit | edit source]
Common postural deformities can be viewed from the side, as is seen in Figure 1.
Lordotic Posture:[4]
- Increased lumbar lordosis
- Increased pelvic anteversion (anterior tilt), which leads to increased hip flexion
- Knees may be hyperextended, which causes plantar flexion at the ankle
- The head line runs posteriorly to the lumbar vertebral bodies, and anteriorly to the knee joint axis
- Increased thoracic
- Head protraction
- Flattened or reversed lower cervical lordosis, with increased upper cervical lordosis
- Protraction of the shoulders
- Pronounced abdomen
- There may be deformation of the rib cage, which can affect inspiration
- There may be anteversion of the pelvis
- There may be cervical osteophytosis (i.e. the formation of bone spurs) and possible stress at the upper part of the oesophagus and dysphagia
- The head line is anteriorly to the thoracic spine, lumbar vertebral bodies, and hip and knee joint axis
- Loss of lumbar lordosis
- Flattened lower part of thoracic kyphosis, but increased upper thoracic region
- Potentially kyphotisation at the cervico-thoracic junction
- There may be a forward head position
- Either neutral pelvis or decreased anterior tilt
- Retraction of the hamstring muscles
- The head line and the base line usually overlap and pass anteriorly to the lumbar vertebral bodies and posterior to the hip joint axis. The head may be shifted anteriorly to the base line.
- Anterior pelvic shift
- Thoracic kyphosis, which extends into the upper lumbar spine
- Shorter lumbar lordosis
- Normal or slightly decreased anterior pelvic tilt
- The dorsal spine is displaced posteriorly while the head and pelvis are anterior to the plumb line
It is possible to observe changes in a client's posture during swallowing, phonation / singing. These changes will provide the therapist with information about patterns and compensatory movements.[1] If active correction is possible, while maintaining the correct posture it is advisable to encourage re-education techniques.[1] If active corrections are not easy or limited, it is advisable to treat the patient with passive manual techniques, elongation of retracted muscle chains and manual therapy.[1]
Posterior View[edit | edit source]
Four specific conditions related to the ascending or descending syndrome can be observed from a posterior view.[1]
Ascending postural syndrome:[1]
- Head and shoulder are in line with the plumb line
- Pelvis is displaced
Descending postural syndrome:[1]
- Head and shoulder are displaced
- Pelvis is central
Mixed ascending and descending postural syndrome:[1]
- The upper part is displaced in one direction and the lower part is displaced to the opposite side
Non-harmonic postural syndrome:[1]
- All sectors (head, shoulders and pelvis) are displaced to the same side
- This is a more common presentation after trauma
Muscle Chains[edit | edit source]
These postural syndromes are caused by abnormalities in muscle or myofascial chains. It is proposed that muscles do not function as independent units, but rather they are part of a "tensegrity-like, body-wide network, with fascial structures acting as linking components.”[6] Muscle chains are the functional anatomical expression of neuromuscular control and they:[1]
- Induce movement
- Facilitate cross movement
- Transmit mechanical tension to the postural system
Because the postural system has to compensate to maintain a static position or to support dynamic movement, muscle chains are part of the proprioceptive system.[1]
Proprioceptors (e.g. muscle spindles, golgi tendon organs) inform the upper control centres about the state of the body (e.g. limb position and movement, sense of tension or force, balance or effort[7]). They facilitate complex movement, but also cause remote compensations.[1]
Limitations:
- There is a lack of consistency in the literature about which muscles are included in each chains[8]
- It is difficult to describe in a reliable way the relationships between body parts that are further apart. It is easier to assess the effect of retractions that are in closer proximity (e.g. neck - shoulder - head - larynx – mandible)[1]
Trauma and the Compensatory Mechanism[edit | edit source]
It is possible to understand postural compensation by comparing it to the processes that occur after trauma, such as an ankle sprain.[1]
Acute phase[edit | edit source]
- The traumatic event destabilises the system
- There is pain and changes in the motor (e.g. gait) and postural patterns[1]
Post-acute phase[edit | edit source]
- Even without pain, postural changes occur during the acute phase
- These changes need to be re-educated in order to avoid alterations in tension in the postural muscle chains[1]
Forward Head Position[edit | edit source]
Abnormal posture of the head at the cervical and scapular level can be associated with several postural anomalies.
- Forward head posture is more pronounced in individuals with shoulder pain (associated with overuse syndrome of shoulders)[9]
- Shoulder injury can have a negative influence on neck alignment.[10] There can be alterations in trapezius kinematics in patients who have neck pain and shoulder dysfunctions[1]
- Increasing thoracic kyphosis results in an increased retraction and anterior tilt of the scapula[1][11]
- Increasing thoracic kyphosis has also been associated with decreased posterior tilt of scapula and increased elevation[1]
Forward head position can also cause:[1]
- Strain on the oesophagus due to its proximity to the cervical spine
- The oesophagus originates in the neck, at the pharyngoesophageal junction (i.e. the C5-6 vertebral interspace at the inferior border of the cricoid cartilage). It travels down anteriorly to the vertebral column[12]
- When there is extension of the upper part of the cervical spine associated with a forward head posture, there is elevation of the mandible.
- This can disturb the hyoid bone, which also influences the larynx[1]
- This posture also causes changes in the vocal tract, with associated alterations in the vocal spectrum and in the structures that produce sound
- When there is flexion of the upper cervical spine associated with a forward head position, the vocal tract will not be in an optimal position. Ideally, the vocal tract should be in a vertical position and the palatal line should be horizontal[1]
Stomatognathic System[edit | edit source]
The stomatognathic system is a functional unit which includes the maxilla and mandible, dental arches, soft tissues (salivary glands, nervous and vascular supplies), the temporomandibular joint (TMJ) and masticatory muscles.[13] It plays a significant role in postural control,[13] influencing the system through:[1]
- Muscle tension
- Fascial retractions
- Neurological stimulation
The TMJ has connections to the cervical spine via muscles and ligaments, forming a functional complex called the cranio-cervico-mandibular system.[13] The posterior system is, therefore, connected to the anterior muscle chains. Speaking and swallowing are related to the mandibular, pharyngeal and laryngeal system (pharingo-glosso chain) and occlusal stresses are applied to the maxillary bones. The styloid muscles (stylohyoid, stylopharyngeus, and styloglossus muscles[14]) act on the cranial system, tongue, pharynx and hyoid bone.[1]
The Larynx[edit | edit source]
The laryngeal structure, including the hyoid, is an important crossing point of myofascial tensions.[1]
The hyoid bone is positioned in the middle of the neck anteriorly at the base of the mandible and posteriorly, at C4.[15] It is just superior to the thyroid cartilage. While it does not connect to other bones, it is closely associated with an extended tendon-muscular complex. It is anchored by muscles from the larynx, pharynx, tongue, and the floor of the mouth.[15]
In a neutral position, the larynx should maintain its position in relation to the cervical spine and mandible, but this position often changes between people.[1]
When assessing the larynx, it is essential to note prevailing movement - in a normal condition, after moving, the larynx typically returns to a neutral position. If there are abnormal tensions, there will be a restriction of mobility in the opposite parameters. Examples of aberrant movement include:[1]
- Upward movement without returning to neutral
- Upward movement combined with a lateral movement
- Tilting position with a poor return
- Inefficient tilting or anterior tilting of the larynx
Laryngeal muscles are part of more global muscle chains and they can be affected by tensions from within these functional groups.[1]
Muscle Chains Associated with the Larynx[edit | edit source]
Posterior Cross Chain[edit | edit source]
The posterior cross chain is an extension chain. While it is not directly connected to the larynx, it includes muscles that attach to the cranium, the sub nuchal line and, thus, they affect the laryngeal tract.[1]
Anterior Bending Chain[edit | edit source]
Muscles in the anterior bending chain include:
- Digastric
- Mylohyoid muscle
- Geniohyoid muscle
- Thyrohyoid muscle
- Sternothyroid
- Sternohyoid muscle
Anterior Cross Chain[edit | edit source]
The anterior cross chain includes muscle layers that connect the left half of the trunk to the right half and vice versa. They include:
- Temporalis
- Masseters
- Internal and external pterygoids
It helps to stabilise the mandible through the bi-condylar axis.[1]
Rear Cross Chain[edit | edit source]
The rear cross chain crosses frontally with the hyoid and laryngeal fulcrum and inserts posteriorly at the contralateral scapula with the omohyoid.[1]
Pharyngo-Vertebral Chain (Deep Chain)[edit | edit source]
The pharyngo-vertebral chain is the myofascial system related to swallowing and breathing. It is connected to the vertebral tract and the cranial base. Muscles within this chain include:
- Pharyngeal constrictor muscles
- Styloid muscles
This chain is affected by problems of the cervical spine including forward head position and the formation of osteophytes.[1]
Summary[edit | edit source]
- There are specific postural changes that become more pronounced with age
- Common postural abnormalities can be viewed from the side or from the rear
- Some postural abnormalities are more amenable to physical correction than others, including non-structured postures
- Changes in posture can affect speech and swallowing, so they are highly relevant in the field of speech therapy
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 1.38 1.39 Banfi M. Postural Principles Useful in Speech Therapy. Physioplus. 2021.
- ↑ Sato K, Chitose SI, Sato K, Sato F, Ono T, Umeno H. Dysphagia precipitated by cervical lordosis in the aged. Ear Nose Throat J. 2020:145561320946644.
- ↑ Nishimura H, Endo K, Aihara T, Murata K, Suzuki H, Matsuoka Y et al. Risk factors of dysphagia in patients with ossification of the anterior longitudinal ligament. J Orthop Surg (Hong Kong). 2020;28(3):2309499020960564.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13:6.
- ↑ Horn SR, Poorman GW, Tishelman JC, Bortz CA, Segreto FA, Moon JY et al. Trends in treatment of scheuermann kyphosis: A study of 1,070 cases from 2003 to 2012. Spine Deform. 2019;7(1):100-106.
- ↑ Wilke J, Krause F, Vogt L, Banzer W. What Is evidence-based about myofascial chains: a systematic review. Arch Phys Med Rehabil. 2016;97(3):454-61.
- ↑ Proske U, Gandevia SC. The proprioceptive senses: their roles in signaling body shape, body position and movement, and muscle force. Physiol Rev. 2012;92(4):1651-97.
- ↑ Rosário JL. Understanding muscular chains – a review for clinical application of chain stretching exercises aimed to correct posture. EC Orthopaedics. 2017;5(6):209-34.
- ↑ Singla D, Veqar Z. Association between forward head, rounded shoulders, and increased thoracic kyphosis: a review of the literature. J Chiropr Med. 2017;16(3):220-9.
- ↑ Katsuura Y, Bruce J, Taylor S, Gullota L, Kim HJ. Overlapping, masquerading, and causative cervical spine and shoulder pathology: a systematic review. Global Spine J. 2020;10(2):195-208.
- ↑ Ludewig PM, Braman JP. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16(1):33-39. doi:10.1016/j.math.2010.08.004
- ↑ Kuo B. Urma D. Esophagus - anatomy and development. GI Motility Online. 2006.
- ↑ 13.0 13.1 13.2 Cuccia A, Caradonna C. The relationship between the stomatognathic system and body posture. Clinics (Sao Paulo). 2009;64(1):61-66.
- ↑ Abuhaimed AK, Alvarez R, Menezes RG. Anatomy, Head and Neck, Styloid Process. [Updated 2021 Jan 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540975/
- ↑ 15.0 15.1 AlJulaih GH, Menezes RG. Anatomy, Head and Neck, Hyoid Bone. [Updated 2020 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539726/