Postero-lateral Elbow Instability
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
add text here related to databases searched, keywords, and search timeline
Definition/Description[edit | edit source]
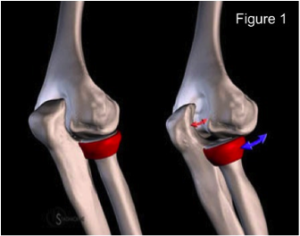
Posterolateral rotatory instability (PLRI) of the elbow was first described in 1991 by O’Driscoll et al. as a condition that is part of a spectrum of instability caused by persistent insufficiency of the lateral collateral ligament (LCL) complex, most notably the lateral ulnar collateral ligament (LUCL) (Sanchez-Sotelo-2005,O’Driscoll-1992). In 2008, Charalambous et al. reported,“PLRI is the most common type of symptomatic chronic instability of the elbow.” In PLRI, the proximal radius and ulna externally rotate together as a unit in relation to the humerus, causing posterior subluxation or dislocation of the radial head relative to the capitellum, without associated instability of the proximal radioulnar joint (Figure 1). (Charalambous-2008, Dunning-2001).
Epidemiology /Etiology[edit | edit source]
Anatomy[edit | edit source]
The LCL, radial head and coronoid process, and the common extensor origin all help prevent posterolateral laxity of the elbow. If a patient is deficient in one or more of these key supporting structures, they may be predisposed to PLRI. (Charalambous 2008)
- Ligamentous constraints: Injury to or laxity of the LUCL was initially thought to be the cause of PLRI, described by O’Driscoll in 1991 as the “critical portion of the ligament complex securing the ulna to the humerus” which helps prevent PLRI. However, in more recent research, the entire LCL complex and the surrounding tissues has been deemed responsible for contributing varus joint stability, limiting external rotation of the radius and ulna on the humerus, and preventing PLRI. (Dunning 2001***TONS MORE SAY THIS TOO) The LCL complex is comprised of the RCL, LUCL and annular ligament. (Charlambous-2008, Murthi 2010) In PLRI, the annular ligament usually remains intact as the proximal radioulnar joint does not dislocate. (O’Driscoll 1991) ***IMAGE OF LIGAMENTS
- Osseous constraints: The most fundamental element of stability in the elbow is attributed to the bony structure. (Savoi 2006) The radial head has been recognized as an important secondary elbow stabilizer due to the osseous congruency it contributes to the joint and the tension it provides to the LCL complex. (Murthi-2010, Charlambous 2008). Researchers have also recognized the coronoid process of the ulna as an important elbow stabilizer. The coronoid process helps to prevent posterior displacement of the ulna on the humerus during axial and varus loading. (Charlambous-2008)
- Muscular constraints: Muscular forces across the elbow joint enhance elbow stability and limit PLRI. The brachialis, biceps, and triceps increase osseous stability as they compress the joint and assist with varus and valgus stability. The common wrist extensors also have been shown to substantially enhance stability of the lateral elbow. (Murthi 2010)
Mechanism of Injury[edit | edit source]
Any condition that disrupts the LCL complex can predispose the elbow to PLRI. LCL disruption most commonly results from trauma causing elbow subluxation or dislocation. Additionally, attritional laxity or attenuation of the LCL, or iatrogenic and surgical issues may also lead to PLRI. (Mueller-2010, Murthi-2010, Charalambous-2008) In 75% of patients younger than 20 years old, PLRI is the result of an elbow dislocation that injures the LCL complex. In adults, PLRI is more commonly caused by a varus extension stress to the elbow without dislocation, often initially diagnosed as a sprain. (Johnston-1996, Bell 2008).
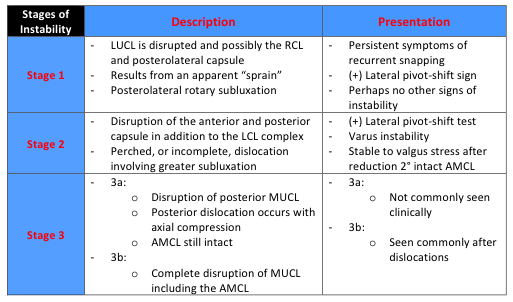
- Trauma/Dislocation: Elbow dislocations or subluxations are usually the result of a fall on the outstretched hand (FOOSH). Typically, a person will fall onto a slightly flexed elbow and pronated forearm as the hand initially contacts the ground. Then the humerus internally rotates with respect to the fixed forearm and a valgus or external rotation force is imparted to the elbow. (O’Driscoll 1999, Murthi 2010) This order of events will most commonly result in PLRI. Traumatic disruption of soft tissue generally starts with the LCL and progresses in a circular fashion, laterally to medially, as described by O’Driscoll’s spectrum of instability. (Table 1) The LCL is almost always disrupted in elbow dislocations from a traumatic fall. (O’Driscoll 1999) Elbow dislocations are estimated to occur in 6/100,000 people and are the most common cause of ligamentous injury that result in instability. Of those dislocations, greater than 95% occur in a posterolateral direction. (Eygendaal-2004) After dislocation, about 15 – 35% of people will experience a recurrence of instability.(Murthi 2010).
- Laxity/Attenuation of the LCL: Attritional laxity of the LCL can occur with chronic soft tissue overload. An example of this can be seen in elbows with a cubitus varus deformity which can be caused after malunion of a supracondylar humeral fracture in children. (Mueller 2010, Charalambous-2008) LCL insufficiency has also been reported in patients with lateral epicondylitis who received repetitive corticosteroid injections. (Mueller 2010) PLRI may also be seen in patients that require long-term upper extremity weight bearing through an assistive device. Patients with connective tissue disorders such as Ehlers-Danlos syndrome have also been noted to develop PLRI. (O’Driscoll 1999)
- Iatrogenic/Surgical Causes: Intensive debridement or an over-aggressive lateral epicondyle release for patients with lateral epicondylitis may cause iatrogenic PLRI. (Charalambous-2008, Bell-2008, Hickey-2006, Mueller 2010) Surgical procedures such as a radial head resection and other surgical approaches to the lateral side of the elbow joint have also been noted to predispose patients to PLRI. (Murthi-2010, Bell-2008, Charlambous-2008
Table 1: A Spectrum of Instability (O'Driscoll 1992)
Characteristics/Clinical Presentation[edit | edit source]
Patients with PLRI may present with a spectrum of different symptoms ranging from vague pain in the elbow to recurrent posterolateral dislocations. The most common patient complaints/symptoms are recurrent popping, clicking, clunking, or locking, accompanied by a sense of instability in the elbow. These symptoms occur during the act of extension and supination, especially when an axial load is applied through the upper extremity. (hickey 2006) (Bell 2008)(Eygendaal 2004) (Charalambous 2008) (Odriscoll 1999) (Murthi 2010) (Mueller 2010) Other symptoms consist of subluxation, a sense of weakness, and functional disability. (Muller 2010)(Bell 2008)Recurrent complete dislocations are rare. (Bell 2008) Pushing down with the upper extremity to rise from a seated position, performing press-up/push-up exercises, and pushing heavy objects with an extended arm are common activities that patients with PLRI report that reproduce their symptoms. (Hickey 2006) (Charalambous 2008)(Murthi 2010)
Differential Diagnosis[edit | edit source]
- Simple elbow sprain: Acutely misdiagnosed as a simple sprain when in fact, PLRI exists. (O’Driscoll 1992)
- Lateral epicondylitis : When lateral epicondylitis does not respond to conservative treatment it is often times the result an underlying LUCL injury. With MRI, LUCL abnormalities have been found in up to 63% of patients with lateral epicondylitis. (Bredella 1999)
- Radial tunnel syndrome (Bell 2008)
- Valgus instability (Bell 2008)
- Pure proximal radial head dislocation (Bell 2008)
Examination[edit | edit source]
An examination of a patient with PLRI may be unremarkable except for a positive posterolateral rotary pivot-shift test described by O’Driscoll. Range of motion is usually within normal limits, and varus and valgus stress tests are usually not provocative. (Savoi 2006)(O’Driscoll 1999)(Murthi 2010) Performing a valgus stress test with the forearm in supination stresses the posterolateral structures. It is possible for this to produce a palpable subluxation of the radial head, but this is uncommon.(Bell 2008)The posterolateral rotary pivot-shift test (described in Table 2) is considered positive when there is a subluxation of the radial head followed by a reduction at the end of the test. This is not always easy to perform on awake patients secondary to muscle guarding.(O’Driscoll 1999)(Bell 2008) The test is the most accurately and easiest to asses when the patient is under general anesthesia. (O’Driscoll 1999)(Bell 2008) For patients who are awake, feelings of apprehension or pain can be considered a positive test (Bell 2008). This is why the test is also known as the lateral pivot-shift apprehension test. Another clinical test that is less difficult to perform is the posterolateral drawer test, but it is not as sensitive as the pivot shift test.(O’Driscoll 1999) There are several functional tests that can be used clinically to test for PLRI. These tests include pushing up from a chair, attempting a push-up with the forearm supinated, and the tabletop test. (Murthi 2010) (Savoi 2006) Charalambous (2008)These tests impose an axial load through the arm while the patient is extending the elbow with the forearm supinated. The tests are considered to be positive if they recreate the patient’s symptoms of apprehension, instability or subluxation. (Murthi 2010) Descriptions of these tests can be found in Table 2. “The diagnosis of posterolateral instability is sometimes based only on a clinical impression because the patient cannot tolerate the subluxation of the elbow.” (Murthi 2010)
Table 2: Clinical Tests for Posterolateral Rotary Instability of the Elbow(Charalambous 2008)
Additional Examination Considerations[edit | edit source]
After an acute dislocation, it is important to remember to do a thorough neurovascular examination before and after reduction of the joint. The wrist and shoulder should also be examined for associated upper extremity injury. (Hickey 2006)
Imaging[edit | edit source]
For patients with PLRI, plain radiographs usually appear normal. Fluoroscopic evaluation performed during a pivot shift test is the preferable imaging method for diagnosing PLRI. Gravity- assisted stress radiographs also frequently demonstrate posterolateral instability.(Hickey 2006) The use of MRI to confirm a tear of the LUCL can be complex and even unreliable(Osborne 2008).
Medical Management (current best evidence)[edit | edit source]
Surgery is often indicated for PLRI, especially when conservative treatment is unsuccessful. (Savoi 2006). If the lateral ligament complex is suspected to be injured after an acute injury, stabilization of the elbow in pronation with a hinged brace should be implemented for 4-6 weeks (Bell 2008). The aim of bracing is to limit valgus loading and supination (Charalambous 2008). For patients who are able to modify their activities, surgery may not be necessary. However, for most patients with recurrent instability or those who have persistent symptoms, surgery is the treatment of choice (Savoi 2006) (Hickey 2006) (Bell 2008) (Eygendaal 2004), This is especially true when conservative treatment has failed to address pain and functional limitations. Time alone will not restabilize an incompetent LUCL. (Hickey 2006).
Surgery[edit | edit source]
Surgery aims to reconstruct the LUCL, thereby restoring rotational stability to the humeroulnar joint (Murthi 2010). A review of the literature shows that the vast majority of the time, surgical treatment has proven to provide successful results (Charalambous 2008). Patients who sustain PLRI through trauma tend to have better outcomes after surgery. The type of surgery depends on the underlying pathology. Most often, a tendon graft is used to reconstruct the incompetent lateral ligaments. This type of reconstruction has consistently provided better results than a ligamentous repair (Sanchez-Sotelo) (2005). Arthroscopy is the alternative (Charalambous 2008).
- Open graft reconstruction technique: Most often, a graft from the Palmaris or plantaris tendon is attached to the posterolateral aspect of the epiondyle and is passed through bone tunnels to the supinator crest of the ulna. The aconeus is first swept posteriorly to allow placement of the bone tunnels (Savoi 2006) (Murphy 2010). To avoid multiple incision sites, Olsen (Olsen 2003) suggests using a triceps tendon graft, which has proven to be reliable in stabilizing the elbow, preventing movement deficits, and eliminating pain (Olsen 2003). This technique also allows for an accelerated rehab program (Eygendaal 2004).
- Arthroscopic Surgical Technique: Sutures are used to plicate the lateral ligament complex and are then tied over or under the anconeus muscle. The entire complex is then sutured to the humerus (Savoi 2006).
Post-Surgical Care[edit | edit source]
The immobilization period after surgery varies depending on the technique. Most often, the elbow is positioned in 90 degrees of flexion and full pronation and is immobilized in a splint for 7 days to 2 weeks. (Bell 2008) (Murthi 2010) (Hickey 2008). The splint is then replaced with a hinged brace with a 30 degree extension block. Active assisted range of motion exercises are performed for the first six weeks, and at this point, the hinged brace is unlocked. The forearm remains in pronation for flexion and extension exercises. Supination and pronation exercises are done with the elbow at 90 degrees of flexion. These exercises are continued after the brace is unlocked, and are progressed to flexion and extension in neutral and eventually in supination. After 8 weeks, strengthening can begin, but may begin in as little as one week, depending on the surgeon and technique used (Evgendaal 2004). The brace is then removed between 8 and 12 weeks. Activity is no longer limited after four to six months, but varus stresses should be avoided. (Murthi 2010) (Hickey 2006).
Physical Therapy Management (current best evidence)[edit | edit source]
General[edit | edit source]
Evidence for non-surgical management of PLRI is scarce. Goals of treatment include patient education to avoid unstable positions of the arm, as well as motion restoration without compromising the stability of the elbow (Murthi 2010) (Ulh 2000). Much like treatment post surgery, immobilization after reduction in full pronation and 90-120 degrees of elbow flexion is encouraged to promote stability and restrict destabilizing forces on the elbow (Uhl 2000) (Wolf 2006). The period of immobilization depends on the level of stability and can last anywhere from three to four weeks (Murthi 2010). Clinicians must keep in mind that the longer the elbow is immobilized, the greater risk there is for adhesions and flexion contractures (Uhl 2000). After 10-14 days of immobilization in a posterior splint or cast, a hinged splint with an extension block is used (Uhl 2000). Mobilization should begin within a few days after the injury and must be protected and supervised (Wolf 2006). Early on, patients can safely begin active and passive mobilization with the use of a brace and the forearm in full pronation (Dunning 2001). Patients with PLRI should avoid placing the arm in abduction or internal rotation while performing elbow flexion and extension range of motion exercises.
Supination of the ulna away from the humerus is the main cause of instability. Therefore, treatment should be aimed at ensuring that the stabilizers of the humeroulnar joint are efficient (Murthi 2010). Muscle activity is a significant contributer to poterolateral stability of the elbow (Dunning 2001). The brachialis, brachioradialis, biceps, and triceps all act to compress joint surfaces together. Strengthening is a key component to increase stability in the lateral ulnar collateral ligament deficient elbow. However, evidence is lacking regarding how the strengthening of these muscles directly reduces instability. A randomized controlled trial by Ocarino et al. (Ocarino 2008), found that strengthening the elbow flexors throughout full range of motion significantly increased elbow stiffness compared to strengthening in a limited range. The authors also determined that both ranges of strengthening significantly modified the elbow’s resting position to a greater degree of flexion (Ocarino 2008). This last finding is especially significant, as a fully extended position of the elbow leaves the lateral ligaments most vulnerable to instability (Hickey 2006). Clinicians must consider each patient’s presentation and fine-tune their treatment in order to achieve the ideal balance of elbow stability and mobility.
Example of a Conservative Treatment Guideline[edit | edit source]
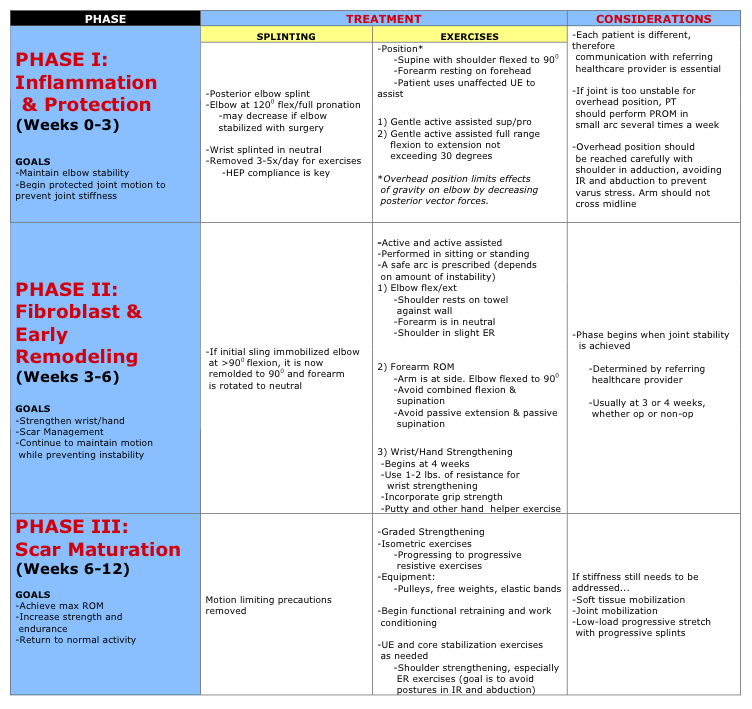
In 2006, Wolf et al. (Wolf 2006) published a treatment guideline which they found to be effective for managing lateral elbow instability. However, no patient outcomes are cited. These are clinical opinions. The author contends that further evidence is needed to study the outcome of certain rehabilitation techniques (Wolf 2006). These guidelines are broken up into three phases and apply to situations where the elbow was reduced operatively or non-operatively post injury. Clinicians can use this information as a guideline when treating patients with PLRI. They are summarized in Table 3:
Figures ____ depict the correct position to perform the exercises in Phase 1 (Wolf 2006)
Case Study [edit | edit source]
Other clinicians have published case studies with detailed descriptions of conservative treatment specific to a certain patient. An example of a much more aggressive rehabilitation program, as described by Uhl, et al. (Uhl 2000), can be found by following this link: Rehabilitation After PosterolateraI Dislocation of the Elbow in a Collegiate Football Player: A Case Report.
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
Low-level evidence exists regarding the physical therapy treatment of PLRI. Therapists must utilize clinical judgment and treat each case individually. Proficient communication with referring health care providers is essential, and a thorough understanding of the anatomy and biomechanics surrounding the condition is required. Using these tools, plus the available evidence, clinicians can successfully treat existing posterolateral rotary elbow instability and prevent the occurrence of it following elbow dislocation.
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.