Postero-lateral Elbow Instability
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
add text here related to databases searched, keywords, and search timeline
Definition/Description[edit | edit source]
Posterolateral rotatory instability (PLRI) of the elbow was first described in 1991 by O’Driscoll et al. as a condition that is part of a spectrum of instability caused by persistent insufficiency of the lateral collateral ligament (LCL) complex, most notably the lateral ulnar collateral ligament (LUCL). (Sanchez-Sotelo-2005, O’Driscoll-1992) In 2008, Charalambous et al. reported, “PLRI is the most common type of symptomatic chronic instability of the elbow.” In PLRI, the proximal radius and ulna externally rotate together as a unit in relation to the humerus, causing posterior subluxation or dislocation of the radial head relative to the capitellum, without associated instability of the proximal radioulnar joint. (Charalambous-2008, Dunning-2001).
Epidemiology /Etiology[edit | edit source]
Anatomy[edit | edit source]
The LCL, radial head and coronoid process, and the common extensor origin all help prevent posterolateral laxity of the elbow. If a patient is deficient in one or more of these key supporting structures, they may be predisposed to PLRI. (Charalambous 2008)
- Ligamentous constraints: Injury to or laxity of the LUCL was initially thought to be the cause of PLRI, described by O’Driscoll in 1991 as the “critical portion of the ligament complex securing the ulna to the humerus” which helps prevent PLRI. However, in more recent research, the entire LCL complex and the surrounding tissues has been deemed responsible for contributing varus joint stability, limiting external rotation of the radius and ulna on the humerus, and preventing PLRI. (Dunning 2001***TONS MORE SAY THIS TOO) The LCL complex is comprised of the RCL, LUCL and annular ligament. (Charlambous-2008, Murthi 2010) In PLRI, the annular ligament usually remains intact as the proximal radioulnar joint does not dislocate. (O’Driscoll 1991) ***IMAGE OF LIGAMENTS
- Osseous constraints: The most fundamental element of stability in the elbow is attributed to the bony structure. (Savoi 2006) The radial head has been recognized as an important secondary elbow stabilizer due to the osseous congruency it contributes to the joint and the tension it provides to the LCL complex. (Murthi-2010, Charlambous 2008). Researchers have also recognized the coronoid process of the ulna as an important elbow stabilizer. The coronoid process helps to prevent posterior displacement of the ulna on the humerus during axial and varus loading. (Charlambous-2008)
- Muscular constraints: Muscular forces across the elbow joint enhance elbow stability and limit PLRI. The brachialis, biceps, and triceps increase osseous stability as they compress the joint and assist with varus and valgus stability. The common wrist extensors also have been shown to substantially enhance stability of the lateral elbow. (Murthi 2010)
Mechanism of Injury[edit | edit source]
Any condition that disrupts the LCL complex can predispose the elbow to PLRI. LCL disruption most commonly results from trauma causing elbow subluxation or dislocation. Additionally, attritional laxity or attenuation of the LCL, or iatrogenic and surgical issues may also lead to PLRI. (Mueller-2010, Murthi-2010, Charalambous-2008) In 75% of patients younger than 20 years old, PLRI is the result of an elbow dislocation that injures the LCL complex. In adults, PLRI is more commonly caused by a varus extension stress to the elbow without dislocation, often initially diagnosed as a sprain. (Johnston-1996, Bell 2008).
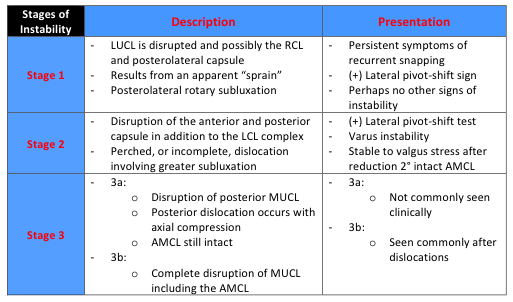
- Trauma/Dislocation: Elbow dislocations or subluxations are usually the result of a fall on the outstretched hand (FOOSH). Typically, a person will fall onto a slightly flexed elbow and pronated forearm as the hand initially contacts the ground. Then the humerus internally rotates with respect to the fixed forearm and a valgus or external rotation force is imparted to the elbow. (O’Driscoll 1999, Murthi 2010) This order of events will most commonly result in PLRI. Traumatic disruption of soft tissue generally starts with the LCL and progresses in a circular fashion, laterally to medially, as described by O’Driscoll’s spectrum of instability. (***TABLE 1***) The LCL is almost always disrupted in elbow dislocations from a traumatic fall. (O’Driscoll 1999) Elbow dislocations are estimated to occur in 6/100,000 people and are the most common cause of ligamentous injury that result in instability. Of those dislocations, greater than 95% occur in a posterolateral direction. (Eygendaal-2004) After dislocation, about 15 – 35% of people will experience a recurrence of instability.(Murthi 2010).
- Laxity/Attenuation of the LCL: Attritional laxity of the LCL can occur with chronic soft tissue overload. An example of this can be seen in elbows with a cubitus varus deformity which can be caused after malunion of a supracondylar humeral fracture in children. (Mueller 2010, Charalambous-2008) LCL insufficiency has also been reported in patients with lateral epicondylitis who received repetitive corticosteroid injections. (Mueller 2010) PLRI may also be seen in patients that require long-term upper extremity weight bearing through an assistive device. Patients with connective tissue disorders such as Ehlers-Danlos syndrome have also been noted to develop PLRI. (O’Driscoll 1999)
- Iatrogenic/Surgical Causes: Intensive debridement or an over-aggressive lateral epicondyle release for patients with lateral epicondylitis may cause iatrogenic PLRI. (Charalambous-2008, Bell-2008, Hickey-2006, Mueller 2010) Surgical procedures such as a radial head resection and other surgical approaches to the lateral side of the elbow joint have also been noted to predispose patients to PLRI. (Murthi-2010, Bell-2008, Charlambous-2008
Table 1: A Spectrum of Instability (O'Driscoll 1992)
Characteristics/Clinical Presentation[edit | edit source]
Patients with PLRI may present with a spectrum of different symptoms ranging from vague pain in the elbow to recurrent posterolateral dislocations. The most common patient complaints/symptoms are recurrent popping, clicking, clunking, or locking, accompanied by a sense of instability in the elbow. These symptoms occur during the act of extension and supination, especially when an axial load is applied through the upper extremity. (hickey 2006) (Bell 2008)(Eygendaal 2004) (Charalambous 2008) (Odriscoll 1999) (Murthi 2010) (Mueller 2010) Other symptoms consist of subluxation, a sense of weakness, and functional disability. (Muller 2010)(Bell 2008)Recurrent complete dislocations are rare. (Bell 2008) Pushing down with the upper extremity to rise from a seated position, performing press-up/push-up exercises, and pushing heavy objects with an extended arm are common activities that patients with PLRI report that reproduce their symptoms. (Hickey 2006) (Charalambous 2008)(Murthi 2010)
Differential Diagnosis[edit | edit source]
- Simple elbow sprain: Acutely misdiagnosed as a simple sprain when in fact, PLRI exists. (O’Driscoll 1992)
- Lateral epicondylitis : When lateral epicondylitis does not respond to conservative treatment it is often times the result an underlying LUCL injury. With MRI, LUCL abnormalities have been found in up to 63% of patients with lateral epicondylitis. (Bredella 1999)
- Radial tunnel syndrome
- Valgus instability (Bell 2008)
- Pure proximal radial head dislocation (Bell 2008)
Examination[edit | edit source]
An examination of a patient with PLRI may be unremarkable except for a positive posterolateral rotary pivot-shift test described by O’Driscoll. Range of motion is usually within normal limits, and varus and valgus stress tests are usually not provocative. (Savoi 2006)(O’Driscoll 1999)(Murthi 2010) Performing a valgus stress test with the forearm in supination stresses the posterolateral structures. It is possible for this to produce a palpable subluxation of the radial head, but this is uncommon.(Bell 2008)The posterolateral rotary pivot-shift test (described in Table 2) is considered positive when there is a subluxation of the radial head followed by a reduction at the end of the test. This is not always easy to perform on awake patients secondary to muscle guarding.(O’Driscoll 1999)(Bell 2008) The test is the most accurately and easiest to asses when the patient is under general anesthesia. (O’Driscoll 1999)(Bell 2008) For patients who are awake, feelings of apprehension or pain can be considered a positive test (Bell 2008). This is why the test is also known as the lateral pivot-shift apprehension test. Another clinical test that is less difficult to perform is the posterolateral drawer test, but it is not as sensitive as the pivot shift test.(O’Driscoll 1999) There are several functional tests that can be used clinically to test for PLRI. These tests include pushing up from a chair, attempting a push-up with the forearm supinated, and the tabletop test. (Murthi 2010) (Savoi 2006) Charalambous (2008)These tests impose an axial load through the arm while the patient is extending the elbow with the forearm supinated. The tests are considered to be positive if they recreate the patient’s symptoms of apprehension, instability or subluxation. (Murthi 2010) Descriptions of these tests can be found in Table 2. “The diagnosis of posterolateral instability is sometimes based only on a clinical impression because the patient cannot tolerate the subluxation of the elbow.” (Murthi 2010)
Table 2: Clinical Tests for Posterolateral Rotary Instability of the Elbow(Charalambous 2008)
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Key Research [edit | edit source]
add text here
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.