Posterior Tibial Tendon Dysfunction: Difference between revisions
Rachael Lowe (talk | contribs) No edit summary |
Rachael Lowe (talk | contribs) No edit summary |
||
| Line 150: | Line 150: | ||
== Medical Management == | == Medical Management == | ||
To decide whether patients need operative or non-operative treatment, different variables have to be taken into account by the attending physician. <ref name="Connor et al.">O'Connor K, Baumhauer J, Houck JR. Patient factors in the selection of operative versus nonoperative treatment for posterior tibial tendon dysfunction. Foot. Ankle International 2010;31(3): 197-202</ref> According to Alvarez et al. | To decide whether patients need operative or non-operative treatment, different variables have to be taken into account by the attending physician. <ref name="Connor et al.">O'Connor K, Baumhauer J, Houck JR. Patient factors in the selection of operative versus nonoperative treatment for posterior tibial tendon dysfunction. Foot. Ankle International 2010;31(3): 197-202</ref> According to Alvarez et al. non-evasive therapy, such as orthosis and physical therapy <ref name="Alvarez et al.">Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int 2006;27(1):2e8</ref> are preferable for they do not damage healthy surrounding tissue, but only when non-operative treatment fails, surgical treatment is required. <ref name="Connor et al." /> <ref name="Matthew D. Nielsen et al.">Nielssen M, Dodson E, Shadrick D, Catazariti A, Mendicino R, Malay S. Nonoperative Care for the Treatment of Adult-acquired Flatfoot Deformity. Foot and Ankle Surgery 2011. 50:311-314 </ref> Clear evidence exists that suggests that the quality of life for patients with posterior tibial tendon dysfunction is significantly affected. Furthermore, evidence suggests that early conservative intervention can significantly improve quality of life regarding disability, function, and pain... <ref name="Durrant B et al.">Durrant B, Chockalingam N, Hashmi F. Posterior tibial tendon dysfunction: a review. J Am Podiatr Med Assoc. 2011;101(2):176-86</ref><br> | ||
'''<u></u>'''Surgical treatment can be used according to the stage in which PTTD is present. | |||
'''<u> | |||
Stage I: <br> | Stage I: <br> | ||
Revision as of 17:29, 17 March 2017
Original Editor - Brian Duffy
Top Contributors - Max Louis, Lien Hennebel, Nele Postal, Admin, Rachael Lowe, Brian Duffy, Xiomara Hernandez, Kim Jackson, Shaimaa Eldib, Lucinda hampton, Tim Hendrikx, Simisola Ajeyalemi, Vidya Acharya, Jess Bell, Pinar Kisacik, Khloud Shreif, Michelle Lee, Kai A. Sigel, Emma Kunnen, 127.0.0.1, Rucha Gadgil and Wanda van Niekerk
Definition/Description[edit | edit source]
The Posterior Tibialis Tendon (Tibialis Posterior) has a leading role in the function of the foot and ankle joint: it plantar flexes the ankle, inverts at the subtalar joint and also has an important role in the function of the medial longitudinal arch. Changes in the posterior tibial tendon, ranging from degeneration to rupture, can lead to various symptoms. These symptoms can be classified into the four different stages of posterior tibial tendon dysfunction (PTTD).
PTTD is a progressive condition. In an early stage (stage I), there are not much symptoms in gait. Stage 1 is a running-related injury but it’s difficult to see related factors to the disease in gait. Other symptoms of PTTD in stage 1 are pain, the area may be red, warm and swollen. Later in stage 2, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle. [1]
Melissa Rabbito et al. investigated how arch structure may play a role in the progressive nature of PTTD. Runners with PTTD were compared with healthy runners. Runners with PTTD had an increased rearfoot pronation compared to the healthy runners, this pronation places greater strain on the tibialis posterior muscle which explains the progressive nature of PTTD. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot.[2]
Edwards et al. state that PTTD is considered to be the main cause of adult acquired flat foot. [3] Posterior tibial tendon dysfunction (PTTD) is according to some authors a synonym to adult acquired flatfoot deformity (AAFD). The treatment for both conditions is therefore similar.<
Clinically Relevant Anatomy
[edit | edit source]
The posterior tibial tendon runs posterior to the medial malleolus inserting into the navicular tuberosity and the plantar aspect of the tarsus. It is the primary stabilizer of the medial longitudinal arch, aiding in mid and hind foot locking during ambulation. If compromised, a resulting pes planus foot may develop and place greater stress on the surrounding ligaments and soft tissue[4]
The posterior tibial tendon during gait:
The functions of a healthy tendon are plantar flexion of the ankle, inversion of the foot and elevating the medial longitudinal arch of the foot (it appears as the primary stabilizer of this arch). This elevating of the medial longitudinal arch causes a locked entire of the mid-tarsal bones, so the midfoot and hindfoot are stiff. All of this allows the muscle gastrocnemius to act more efficiently during gait. When the tibial posterior tendon isn't in health anymore and he doesn't do his work, the other joint capsules and ligaments become weak. There is an eversion of the subtalar joint, abduction of the foot (talonavicular joint) and valgus of the heel. Also a flattened arch develops what can cause an adult acquired flatfoot. And the muscle gastrocnemius is unable to act without the posterior tibial tendon what results in affected balance and gait.
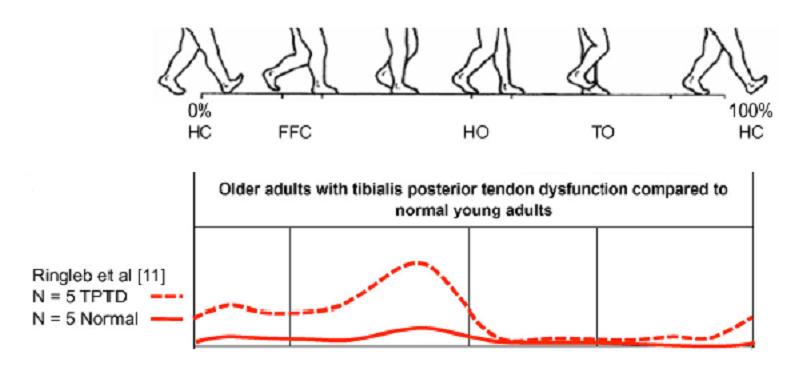
In this figure, they use 'tibialis posterior intramuscular EMG' to quantify the tibial posterior activation during walking. They used participants (female) with acute stage II PTTD. Differences in muscle activation: the participants with PTTD shows a significantly greater tibialis posterior EMG amplitude during the second half of stance phase. They walk with a pronated foot and exhibit an increased tibialis posterior activity compared to the participants without PTTD. [6]
Epidemiology /Etiology[edit | edit source]
Once thought to be a tendonitis, it is now commonly accepted the process is one of tendon degeneration or tendinosis. A poor blood supply has been identified as well as mechanical factors such as peroneal brevis overactivity or a pes planus foot. The latter will gradually place increased stress to the posterior tibial tendon causing early degeneration. Trauma ( ankle sprain, fracture) may also initiate the process[4]
Risk factors to get PTTD are:
- Elderly: especially middle aged women [7][8]
- Young athletes [7]
- Hypertension [7][8]
- Obesity [7][8]
- Diabetes mellitus [7][8]
- Seronegative arthropathies [7]
- Accessory navicular bone [7]
- Ligamentous laxity [8]
- Pes planus (flatfeet) [8]
- Steroid therapy [7][8]
- Accesory navicular: may interfere with posterior tibial tendon function [7]
- Overuse [1] [9]
- Previous trauma (certain types of ankle fracture) [10]
- Steroid injections[10]
- Psoriatic arthritis / Rheumatoid arthritis[10]
Characteristics / Clinical presentation[edit | edit source]
- Pain/swelling behind medial malleolus and along medial longitudinal arch
- Change in static/dynamic foot ( pes planus)
- Limited walking ability
- Impaired balance
- Impaired MMT PF/IV
- Difficulty/inability to perform unilateral heel raise. Limited calcaneal inversion upon ascent
- Impaired subtalar mobility
- Lateral ankle pain due to subfibular impingement is a late symptom [11]
Differential Diagnosis[edit | edit source]
- Degenerative arthritis of the ankle, talonavicular or tarsometatarsal joint [7][12]
- Neuropathies of the foot caused by diabetes mellitus or peripheral neuropathies (or leprosy) [7]
- Spring ligament dysfunction [7]
- Rupture of anterior tibial tendon [7]
- Tarsal coalition [7]
- Congenital vertical talus [7]
- Kholers disease [7]
- Tarsal tunnel syndrome [7]
Diagnostic Procedures[edit | edit source]
Besides the clinical diagnosis, radiographic evaluation ca be used to asses deformity and the possible presence of degenerative arthritis or other causes of pes planus. MRI has the highest sensitivity, specificity and accuracy, but ultrasound is less expensive and almost as sensitive and specific as MRI.
Clinical test (more information in Examination) [13]
- Too many toes sign [14]
- Double-limb heel rise
- Heel rise
- Single heel rise
- First metatarsal rise sign (Hintermann and Gachter)
- Plantar flexion and inversion of the foot against resistance
Stages of PTTD[edit | edit source]
As per Johnson and Strom[1][9][14] [14]:
- Stage I: Posterior tibial tendon intact and inflammed, no deformity, mild swelling
- Stage II: Posterior tibial tendon dysfunctional, acquired pes planus but passively correctable, commonly unable to perform a heel raise
- Stage III: Degenerative changes in the subtalar joint and the deformity is fixed
- Stage IV ( Myerson): Valgus tilt of talus leading to lateral tibiotalar degeneration
Stage I
- Deformity: tenosynovitis
- physical exam: single-leg toe raise test (+)
- radiography: normal
Stage IIA
- Deformity: Flatfoot deformity, flexible hindfoot, normal forefoot
- Physical exam: single-leg heel raise (-), mild sinus tarsi pain
- radiography: arch collapse deformity
Stage IIB
- Deformity: Flatfoot deformity, flexible hindfoot/rear foot, forefoot abduction
- physical exam: Same stage IIA
- radiography: same stage IIA
Stage III
- deformity in stage II becomes fixed, rigid or inflexible
- Deformity: flatfoot deformity, rigid forefoot abduction, rigid hindfoot/rearfoot valgus
- physical exam: sever sinus tarsi pain, single-leg heel raise test (-)
- radiography: arch collapse deformity (subtalar arthritis)
Stage IV
- deformity: flatfoot deformity, rigid forefoot abductin, rigid hindfoot/rearfoot valgus, deltoid ligament compromise
- physical exam: single-leg heel raise test (-), severe sinus tarsi pain, ankle pain
- radiography, arch collapse deformity, subtalar arthritis, talar tilt ankle mortise
Examination[edit | edit source]
Before a clinical examination is performed, the patient should be submitted to a series of questions. Based on the answers the physiotherapist can rule out other disorders. It is essential to diagnose posterior tibial tendon dysfunction (PTTD) in an early phase to prevent permanent deformities of the foot/ankle, and because of that a physical examination can be useful [7]. At first, look at the symptoms that can be caused by PTTD. There are many signs the physiotherapist can recognize according to the stage in which PTTD is presented. Additionally some tests can be performed.
It is important to examine the whole lower body and not just the foot, as valgus in the knees can accentuate the appearance of pes planus. The feet themselves should be examined from above, as well as from behind. A healthy person has a 5° valgus in his hindfoot, in patients with PTTD the valgus is increased and the abduction in the forefoot is also more pronounced. [15] The physiotherapist can palpate the posterior tibial tendon from above the medial malleolus to its insertion, to control the integrity and assess possible pain and swelling that are common for the first stages of PTTD. In the later stages the deformity can progress and pes planus may be visible. The physiotherapist can determine the severity of the pes planus by checking how many fingers can be passed underneath the midfoot. [7]
The diagnosis of posterior tibial tendon dysfunction can be made clinically based on history and objective testing.
The examination (objective testing) consists of several tests, namely:[16]
- the too many toes sign (Johnson): the foot should be inspected from behind and above. The too many toes sign is a manner of inspection from behind. At this manner they can establish if there is an abduction of the forefoot and a valgus angulation of the hindfoot. It is based on how many toes you can see from behind. By an affected foot it will be more than one and a half to two toes;
- the double-limb heel rise: one foot rise, while the other foot is lifted off the floor. The normal foot will stay into inversion while the affected hindfoot will stay in valgus;
- heel rise: to go with both feet from a flatfoot stance to standing on the toes. Patients in stage I dysfunction can do this, but it's painfull. Patients with stage II, III or IV dysfunction are unable to do an heel rise. When a patients stands on tiptoes the heel of the affected foot will not bend inwards;
- a single heel rise: patients can't do a single heel rise with the affected foot;
- the first metatarsal rise sign (Hintermann and Gachter): the patients stands on his both feet. The shin of the affected foot is taken with a hand and rotated externally. When the patient has PTTD, the head of metatarsal I is lifted, while normal metatarsal I stays on the ground;
- plantar flexion and inversion of the foot against resistance: to test the power of the tibialis posterior.
Outcome Measures[edit | edit source]
- Foot Function Index (FFI)[13]
- 5-Minute Walk Test [13]
- Instruments to record kinematics from tibia, calcaneus and first metatarsal: e.g. Milwaukee Foot Model [13][17]
Medical Management[edit | edit source]
To decide whether patients need operative or non-operative treatment, different variables have to be taken into account by the attending physician. [18] According to Alvarez et al. non-evasive therapy, such as orthosis and physical therapy [19] are preferable for they do not damage healthy surrounding tissue, but only when non-operative treatment fails, surgical treatment is required. [18] [20] Clear evidence exists that suggests that the quality of life for patients with posterior tibial tendon dysfunction is significantly affected. Furthermore, evidence suggests that early conservative intervention can significantly improve quality of life regarding disability, function, and pain... [21]
Surgical treatment can be used according to the stage in which PTTD is present.
Stage I:
- Decompression of tendon [7][22]
- Open synovectomy [7]
- Some suggest an augmentation of the abnormal tendon with flexor digitorum longus (FDL) tendon.[7]
Stage II: Not yet a preference to which technique should be used. Several interventions possible:
- FDL Transfer and medial displacement calcaneal osteotomy [7][22]
- Lateral column lengthening (e.g. calcaneo-cuboid distraction arthrodesis) [7][23]
- Medial column fusion (navicular-cuneiform or/or metatarsal- cuneiform joint) [7]
- Isolated hindfoot fusions [7]
- Arthroereisis [7][22][23]
Stage III:
- Triple arthrodesis (subtalar, calcaneocuboid and talonavicular fusion) [7]
- Isolated hindfoot fusions (eg. subtalar fusion) or medial column fusion [7]
Stage IV:
- Pan-talar arthrodesis [7]
Physical Therapy Management[edit | edit source]
Non-operative treatment
Treatment can begin in many cases with non-operative treatment that includes:
• Orthotic devices or bracing: to support the arch.
• Immobilization: a short-leg cast or boot, it allows the tendon to heal, or avoid all weight-bearing.
• Physical therapy: ultrasound therapy and exercises help rehabilitate the tendon and muscle following immobilization.
• Medications: nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
• Shoe modifications: advise changes such as special inserts designed to improve the arch support. [1](Level of evidence 5)
The key to a successful outcome is early detection of the dysfunction. A randomised controlled trial by Kornelia Kulig et al. shows us that orthoses use, static stretching of gastrocnemius and soleus muscle, concentric/eccentric training of the posterior tibialis have demonstrated success.
Participants were divided into three groups and in each group, pre- and post-intervention data (Foot Functional Index, distance traveled in the 5-Minute Walk Test and pain immediately after the 5-Minute Walk Test) were collected. The result was that concentric and eccentric progressive exercises improved perceptions of function and reduced pain (together with orthoses use and stretching). As per Kulig et al, orthoses use and eccentric training demonstrate the most improvement over a 12 week period. These results are significant (p<0,05), which means that they found a significant difference between the pre-intervention data and post-intervention data. There can be some doubt whether this is a clinically relevant study or not, because the number of participants is small.
Treatment options per stages of PTTD are determined on the basis of whether there is an acute inflammation and whether the foot deformity is fixed or flexible:
Stage I: Acute: 4-8 weeks immobilisation, RICE; Chronic: flat footwear and corrective orthose or ankle foot orthosis, lace-up
Stage II: Acute 4-8 weeks immobilisation, RICE; Chronic: lace-up, corrective orthosis and flat footwear
Stage III: Lace-up, customised footwear or semirigid shoes and accommodative orthosis
Stage IV: Lace-up, customised footwear or semirigid shoes and accommodative orthosis
The results of a retrospective investigation by Matthew D. Nielsen et al. support the use of a multifaceted conservative approach to the treatment of the AAFD with PTTD. This nonsurgical approach includes:
* initial immobilization
* anti-inflammatory medications
* physical therapy
* bracing
* in particular the construction of a LAFO
This aggressive nonoperative treatment regimen has been successful at alleviating symptoms in 87.5% of patients without the need for surgical intervention.
A prospective cohort study by Alvarez RG et al. teaches us that patients with stage I and stage II PTTD had a successful rehabilitation after:
- Wearing a short articulated ankle foot orthosis or foot orthosis
- High-repetition exercises: to train the muscles in an aerobic manner for
Long-term endurance. High-repetition exercises provide physiological - Aerobic training which decrease the symptoms as pain and impairment
- Aggressive plantair flexion activities
- An aggressive high-repetition home exercises program
- Gastrocsoleus tendon stretching
Criteria for inclusion are
- Palpable and painful posterior tibial tendon with or without swelling
- Movement of the tendon with passive and active non-weightbearing clinical examination: This can be tested by moving the foot from dorsiflexion to plantarflexion with elimination of gravity.
- Stage I or stage II posterior tibial tendon dysfunction
Isokinetic evaluations were done before and after the treatment. The evaluations consists of the comparison between the left and right side, antagonists and agonists and also the total strength generating of the muscle. It means that there is a contraction of the muscle with a constant speed, which is only possible with equipment and not manual. These evaluations compared inversion, eversion, plantairflexion and dorsiflexion strength in the involved and uninvolved sides. 83% had successful subjective and functional outcomes and 89% of the patients were satisfied. 5% failed to improve with this treatment and they required surgery. [19] (level of evidence 2C)
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources[edit | edit source]
Myerson MS. Adult acquired flat foot deformity. J Bone Joint Surg.1996;45A:780-92
Hintermann B, Gachter A. The first metatarsal rise sign: a simple, sensitive sign of tibialis posterior tendon dysfunction. Foot Ankle Int 1996; 17:236-41.
Clinical Bottom Line[edit | edit source]
Posterior tibial tendon dysfunction (PTTD) is one of the most common problems of the foot and ankle. The tendon provides stability for the medial longitudinal arch of the foot. Depending on the stage in which the patient is located, PTTD may result in a flatfoot (stage II, III and IV) due inflammation or strain of the posterior tibial tendon. According to Alvarez RG et al. surgical treatment is only needed when the conservative treatment fails. The symptoms depend on the stage in which the patient is. A good treatment for PTTD is: Orthosis use, Concentric and eccentric training of the tibialis posterior muscle, stretching of the soleus muscle and gastrocnemius muscle. According to a lot of authors, PTTD is one of the leading causes of acquired flatfoot deformity in the adults.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1vCeRl5tNk8Z6wu5F9OtxtyRcRX2OXJP58bBe_47LQlU00WkVm|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 The American College of Foot and Ankle Surgeons . www.acfas.org (Accessed 6 nov 2014) Cite error: Invalid
<ref>tag; name "ACFAS" defined multiple times with different content - ↑ Melissa Rabbito et al., Biomechanical and Clinical Factors Related to Stage I Posterior Tibial Tendon Dysfunction; Journal of Orthopaedic Sports Physical Therapy 2011;41: 776-784
- ↑ William M. Geideman, J. E. Posterior Tibial Tendon Dysfunction. Journal of Orthopedic. J Orthop Sports Phys Ther. 2000;30(2):68-77
- ↑ 4.0 4.1 Kohls-Gatzoulis J, Angel JC, Singh D, Haddad F, Livingstone J, Berry G. Tibialis posterior dysfunction: a common and treatable cause of adult acquired flatfoot. BMJ.2004;329:1328-1333 Cite error: Invalid
<ref>tag; name "Kohls" defined multiple times with different content - ↑ Anatomy Of The Tibialis Posterior Muscle - Everything You Need To Know - Dr. Nabil Ebraheim. Avalaible from: https://www.youtube.com/watch?v=9N_eR8Pojuw
- ↑ Semple R., Murley G., Woodburn J, Turner D. Tibialis posterior in health and disease: a review of structure and function with specific reference to electromyographic studies.Journal of foot and ankle research 2009; 2: 24.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 7.15 7.16 7.17 7.18 7.19 7.20 7.21 7.22 7.23 7.24 7.25 7.26 7.27 7.28 7.29 M.R. Edwards, C. Jack, S.K. Singh. Tibialis posterior dysfunction. Current Orthopaedics 2008; 22: 185 – 192
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Kong, A. Van der Vliet. Imaging of tibialis posterior dysfunction. The British Journal of Radiology, 2008 Oct;81 (970): 826–836
- ↑ 9.0 9.1 Tome J, Nawoczenski DA, Flemister A, Houck J. Comparison of Foot Kinematics Between Subjects With Posterior Tibialis Tendon Dysfunction and Healthy Controls, Journal of Orthopaedic Sports Physical Therapy 36(12):986. http://www.jospt.org/doi/pdf/10.2519/jospt.2006.2293?code=jospt-site (Accesed 24 nov 2006))
- ↑ 10.0 10.1 10.2 Posterior Tibial Tendon Dysfunction. Northwest Foot and Ankle. https://nwfootankle.com/foot-health/drill/3-problems/33-posterior-tibial-tendon-dysfunction (Accessed 12 nov 2014)
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedDeborah Allen - ↑ William M. Geideman, Jeffrey E. Johnson. Posterior Tibial Tendon Dysfunction. Journal of Orthopaedic Sports Physical Therapy 2000;30 (2):68-77
- ↑ 13.0 13.1 13.2 13.3 Kornelia Kulig, Stephen F Reisch I. Nonsurgical Management of Posterior Tibial Tendon Dysfunction With Orthoses and Resistive Exercise: A Randomized Controlled Trial. Physical Therapy 2009;89:26-37
- ↑ 14.0 14.1 14.2 Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Rel Res 1989;239:196-206
- ↑ David B. Thordarson. Foot and ankle. Philadelphia: Lippincott Williams Wilkins, 2004: p. 174-181
- ↑ Trnka, H.-J. Dysfunction of the tendon of tibialis posterior. The journal of bone and joint surgery 2004; 86B:939-946
- ↑ Richard M. Marks, Jason T. Long. Surgical reconstruction of posterior tibial tendon dysfunction: Prospective comparison of flexor digitorum longus substitution combined with lateral column lengthening or medial displacement calcaneal osteotomy. Gait Posture, 2009;29:17-22
- ↑ 18.0 18.1 O'Connor K, Baumhauer J, Houck JR. Patient factors in the selection of operative versus nonoperative treatment for posterior tibial tendon dysfunction. Foot. Ankle International 2010;31(3): 197-202
- ↑ 19.0 19.1 Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int 2006;27(1):2e8
- ↑ Nielssen M, Dodson E, Shadrick D, Catazariti A, Mendicino R, Malay S. Nonoperative Care for the Treatment of Adult-acquired Flatfoot Deformity. Foot and Ankle Surgery 2011. 50:311-314
- ↑ Durrant B, Chockalingam N, Hashmi F. Posterior tibial tendon dysfunction: a review. J Am Podiatr Med Assoc. 2011;101(2):176-86
- ↑ 22.0 22.1 22.2 Parsons S, Naim S. Correction and Prevention of Deformity in Type II Tibialis Posterior Dysfunction. Clinical Orthopaedics and Related Research 2010;468(4):1025-32
- ↑ 23.0 23.1 George A. Arangio , Eric P. Salathe. A biomechanical analysis of posterior tibial tendon dysfunction, medial displacement calcaneal osteotomy and flexor digitorum longus transfer in adult acquired flat foot. Clinical Biomechanics 2009;24(4):385-90