Pivot Shift
Original Editor - Beth Barrett, Heleen Van Cleynenbreugel
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
add text here related to databases searched, keywords, and search timeline
Definition/Description[edit | edit source]
The pivot shift is a dynamic but passive test of knee stability, carried out by the examiner without any activity of the patient. It shows a dysregulation between rolling and gliding in the kneejoint. The patient lies in supine. The movement is a combination of axial load and valgus force, applied by the examiner, during a knee flexion from an extended position. When the test is positive, it indicates an injury of the anterior cruciate ligament. [1](A2)[2](B)
Clinically Relevant Anatomy [edit | edit source]
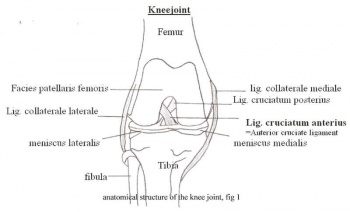
The kneejoint or articulatio genus is the biggest and most complicated synovial joint in the human body. It’s formed by the distal end of the femur and the proximal end of the tibia. Between these two, the medial and lateral meniscus are located. The anterior part of the femur (facies patellaris femoris) articulates with the patella which forms the patellofemoral joint. The cruciate ligaments, situated in the intercondylair space, and the collateral ligaments are important ligaments in the knee.
The anterior cruciate ligament (ACL) joins the area intercondylaris anterior with the medial aspect of the lateral condyle. This ligament extends upwards, dorsally and laterally from the tibial plateau. It prevents the tibia from moving ventrally.
The posterior cruciate ligament (PCL) joins the area intercondylaris posterior with the lateral apect of the medial femurcondyle. The ligament runs medially, straight up and slightly forward. The PCL prevents posterior instability in the knee joint, this means that the tibia doesn’t displace to posteriorly. (Fig 1) [3]
The PCL is stronger than the ACL. Both cruciate ligaments run in a torsion. They stabilize the knee in the sagittal plane. When the knee is in endorotation, the cruciate ligaments are strongly crossed. When in exorotation, they run more parallel. The cruciate ligaments are primarily located in the posterior part of the joint capsule, so the flexion and extension aren’t hampered.[4][5]
Purpose
[edit | edit source]
The purpose of this test is to detect anterolateral rotary instability of the knee. The structures that could be compromised if this test is positive are the ACL, LCL, posterolateral capsule, arcuate complex and ITB.
Technique
[edit | edit source]
The patient lies supine with legs relaxed. The examiner grasps the heel of the involved leg with examiners opposite hand placed laterally on the proximal tibia just distal to the knee. The examiner then applies a valgus stress and an axial load while internally rotating the tibia as the knee is moved into flexion from a fully extended position. [6] A positive test is indicated by subluxation of the tibia while the femur rotates externally followed by a reduction of the tibia at 30-40 degrees of flexion.
Key Research[edit | edit source]
Is the pivot shift test a reliable test?
The Pivot Shift test attempts to reproduce the rotary and transalatory instability in an ACL deficient knee. [7] The test has a sensitivity from 0.18 to 0.48 and a specificity from 0.97 to 0.99 for diagnosing an ACL tear. The mean sensitivity and specificity are respectively 0.32 and 0.98. [8] (A1) [9] (A1) [10] (A1) [11] (A1) [12] (A1) Although the test is clinically relevant and reproduces a functional movement of the knee joint, it is difficult to quantify. Recently a study was done using a navigation system to quantify measurements of knee laxity in individuals who underwent ACL reconstruction. The Pivot shift test was reliable with both patient self-assessment of laxity and with surgical performance. [13] This highlights the clinical relevance of the test. Traditionally, the Lachman was used more often to measure knee laxity due to its quantifiability, however recent advances in technology have allowed for more objective and measurable observations of the motions involved in the pivot shift and may lead to the ability to make the test quanitifiable for research. [14]
(For more information about the accuracy of certain test, in case of an acute knee injury, such as the pivot shift and the lachman test: http://www.aafp.org/afp/2005/0315/p1169.html#afp20050315p1169-t1)
Grading the pivot shift [2] [15]
“A number of variations of the basic pivot shift test also have been described (Hugston et al. 1976; Slocum et al. 1976; Losee, Johnson and Southwick 1978; Galaway and MacIntosh 1980). All these variations indicate anterior translation and rotational subluxation of the tibia on the femur.” [2]
For the pivot shift test, the examiner applies with one hand an axial and valgus load. This hand is also going to control the rotational position of the tibia during the test. With the other hand, the foot is held firmly against the examiner.
The test can be carried out in three positions of rotation: medial, neutral and lateral rotation of the tibia. (Figs 1,2,3) [2]
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1houoX_LGC3R5rodk9lCaF7S5evZ4MXBE6rFjh2K9YsNYupEmB|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Musahl V., Citak M., O’Loughlin PF., Choi D., Bedi A., Pearle AD. The effect of medial versus lateral menisectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2010;38(8):1591-7. http://www.ncbi.nlm.nih.gov/pubmed/20530720?dopt=AbstractPlus full text: http://ajs.sagepub.com.ezproxy.vub.ac.be:2048/content/38/8/1591.full.pdf+htmlfckLR(accessed 19 Nov 2010). Level of evidence: A2
- ↑ 2.0 2.1 2.2 2.3 Jakob RP., Staubli HU., Deland JT. Grading the pivot shift, objective tests with implications for treatment. VOL 69-B, No.2 1987. http://web.jbjs.org.uk/cgi/reprint/69-B/2/294.pdf (accessed 16 Nov 2010). Level of evidence: B
- ↑ http://www.taosortho.com/patientinfo/Medical/knees/ACL.htm (figure 1)
- ↑ Schünke M., Schulte E., Schumacher U., Voll M., Wesker K., Anatomische atlas Prometheus, Algemene anatomie en bewegingsapparaat. Onderste extemiteit: Botten, banden en gewrichten. Houten, 2008.p394, 396.
- ↑ Kapandji IA. Bewegingsleer, de onderste extremiteit deel 2. De functie van de kruisbanden. Houten, 2009. p135.
- ↑ Baxter R. Pocket guide to musculoskeletal assessment, second edition. Elsevier Science 2003.
- ↑ Lane CG, Warren R, Pearl AD. The pivot shift. J Am Acad Orthop Surg. 2008 Dec;16(12):679-88.
- ↑ Scholten RJPM, Opstelten W, van der Plas CG, Bijl D, Deville WLJM, Bouter LM (2003)fckLRAccuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament:fckLRa meta-analysis. J Fam Pract 52:689-94 http://www.ncbi.nlm.nih.gov/pubmed/12967539fckLRfull text: http://web.ebscohost.com.ezproxy.vub.ac.be:2048/ehost/pdfviewer/pdfviewer?hid=18&sid=25c1a906-13aa-4c59-ba43-a64e200c3c12%40sessionmgr13&vid=2 (accessed 18 Nov 2010. Level of evidence: A1
- ↑ Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) ThefckLRreliability, validity, and responsiveness of the Lysholm score and Tegner activity scale forfckLRanterior cruciate ligament injuries of the knee: 25 years later. The American journal of sportsfckLRmedicine 37:890-897 http://ajs.sagepub.com.ezproxy.vub.ac.be:2048/content/37/5/890.full.pdf+html (accessed 18 Nov 2010). Level of evidence: A1
- ↑ Prins M. The lachman test is the most sensitive and the pivot shift the most specific test for the diagnosis of ACL rupture. Fysiotherapeuten nr 8, 2006. http://www.fysioterapeuten.no/xp/pub/mx/filer/0806_Cap.pdf (accessed 17 Nov 2010). Level of evidence: A1
- ↑ Van der Plas CG., Opstelten W., Devillé WLJM., et al. Fysische diagnostiek - de waarde van enkele gebruikelijke tests voor het aantonen van een voorstekruisbandruptuur: meta-analyse. Ned Tijdschr Geneeskd. 2005;149:83-8. http://www.ntvg.nl/publicatie/fysische-diagnostiek-de-waarde-van-enkele-gebruikelijke-tests-voor-het-aantonen-van-een-v/volledig (accessed 16 Nov 2010) Level of evidence: A1
- ↑ Ostrowski JA. Accuracy of 3 Diagnostic Tests for Anterior Cruciate Ligament Tears.J Athl Train 2006; 41(1): 120–121. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421494/ (accessed 16 Nov 2010) Level of evidence: A1
- ↑ Lopomo N, Zaffagnini N, Bignozzi S, Visani A, Marcacci M. Pivot Shift Test: Analysis and Quantification of Knee Laxity Parameters using a Navigaion System. J Orthop Res. 2009 July 29.
- ↑ Katz JW, Fingeroth RJ. The Diagnostic Accuracy of Ruptures of the Anterior Cruciate Ligament comparing the Lachman Test, the Anterior Drawer Sign, and the Pivot Shift Test in Acute and Chronic Knee Injuries. Am J Sports Med. 1986 Jan-Feb;14(1): 88-91.
- ↑ Heijboer MP. Indicatie, fysische diagnostiek van de knie. Chronische knieklachten. Universiteit van Utrecht 2004. p5 and 7 (http://www.scopie.info/files/Website-elementen/kniecursus2004.pdf (accessed 20 Nov 2010)