Physiotherapy Treatment Approaches for Individuals with Cerebral Palsy
Original Editor - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Kim Jackson, Vidya Acharya, Simisola Ajeyalemi, 127.0.0.1, Tarina van der Stockt, WikiSysop, Amanda Ager, Jess Bell, Shreya Pavaskar, Cindy John-Chu and Olajumoke Ogunleye
Inroduction[edit | edit source]
As highlighted by Gunel (2011) Pediatric Rehabilitation requires a Multidisciplianary (MDT) Approach in order to promote the indpendance of the child with an impairment, both functionally and psychologically and increase the quality of life of both the child and their family. Physiotherapists, viewed as the 'movement expert', play a key role within this MDT. The main aim of Physiotherapy, as identified by Gunel (2011), is to support the child with Cerebral Palsy to achieve their potential for physical independence and fitness levels within their community, by minimising the effect of their physical impairments, and to improve the quality of life of the child and their family who have major role to play in the process. [1]
Physiotherapy focuses on function, movement, and optimal use of the child's potential and uses physical approaches to promote, maintain and restore physical, psychological and social well-being within all environments of the child including home, school, recreation, and community environments. [1]
Gross motor skills, functional mobility in the management for the motor deficits, positioning, sitting, transition from sitting to standing, walking with or without assistive devices and orthoses, wheelchair use and transfers, are all areas that the physiotherapist works on using a wide range of physiotherapeutic approaches to infuence functional ability of the child, which we will review. [1] [2]
Treatment Approaches[edit | edit source]
According to Patel (2005) a wide range of therapeutic interventions have been used in the treatment and management of children with cerebral palsy. They show that there is evidence to support the use and effectiveness of neuromuscular electrical stimulation, while evidence in support of the effectiveness of the neurodevelopmental treatment is equivocal at best. The effectiveness of many other interventions, including include: sensory integration, body-weight support treadmill training, conductive education, constraint-induced therapy, hyperbaric oxygen therapy used in the treatment of cerebral palsy have not been clearly established based on well-controlled trials. We provides an overview of salient aspects of popular approaches and interventions used in the management of children with Cerebral Palsy. [2] [3]
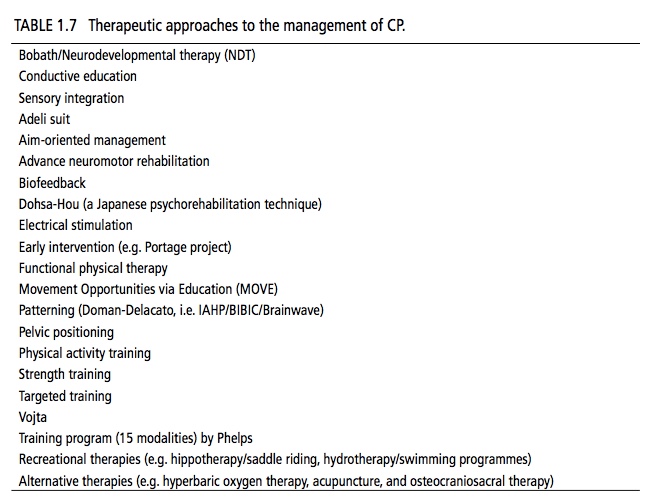
Antilla (2008) identifies a wide range of choices and availability of various techniques which may vary both between therapists and from country to country. Table 1.7 below lists many of the most common physiotherapy and physiotherapy-related approaches utilised in the management of Cerebral Palsy during the past few decades. [4]
Neurodevelopmental Treatment (NDT) [edit | edit source]
One of the more popular approaches utilised in the management of cerebral palsy, the NDT Approach also know as Bobath Approach, was developed in the 1940's by Berta and Karl Bobath, based on their personal observations working with children with cerebral palsy. The basis of this approach is that motor abnormalities seen in children with Cerebral Palsy are due to atypical development in relation to postural control and reflexes because of the underlying dysfunction of the central nervous system. This approach aims to facilitate typical motor development and function and to prevent development of secondary impairments due to muscle contractures and joint and limb deformities. Although the effectiveness of NDT in CP has been questioned by some published reports, there are some studies suggesting its effectiveness.[2]
Constraint-Induced Movement Therapy (CIMT)[edit | edit source]
Constraint-induced Movement therapy is used predominantly in the individual with Hemiplegic Cerebral Palsy to improve the use of the affected upper imb. The stronger or non-impairmed upper limb is immobilized for a variable duration in order to Force Use of the impried upper limb over time [2]. Antilla et al (2008) [3] identified one high and one lower-quality trials which measured both body functions and structures, and activity and participation outcomes through use of CIMT. Use of a cast with CIMT showed positive effects in the amount and quality of functional hand use in th eimpaired limb and new emerging behavior as compared to the no-therapy group, but no effects were found on QUEST. Use of sling during CIMT also had positive effects on functional hand use on teh impaired upper limb, time to complete tasks, and speed and dexterity, but no effects on sensibility, handgrip force, or spasticity. Thus Antilla et al (2005) found there is moderate evidence for the effectiveness of CIMT therapy on functional hand use in th eimpaired upper limb [3]. According to Patel (2005) the efficacy of this approach has not been established, in particular in relation to the adverse effects of prolonged immobilization of the normally developing upper limb [2].
Patterning
[edit | edit source]
The concept of patterning is based on theories developed by Fay, Delacato, and Doman in the 1950s and 1960s. Patterning is based on the principle that typical development of the infant and child progresses through a well–established, pre-determined sequence; and failure to normally complete one stage of development therefore impairs or inhibits the development of the subsequent stage.
It was hypothesized that typical motor development can be facilitated in the brain injured children by passively repeating the sequential steps of typical development, a process called patterning. Parents and other care givers are taught to carry out patterning at home. This approach is labor intensive and time consuming as it requires multiple sessions every day. Effectiveness of patterning has not been established and its use in children with CP is not recommended. [2]
Therapeutic Interventions[edit | edit source]
Passive Stretching[edit | edit source]
It is a manual application for spastic muscles to relieve soft tissue tightness. Manual stretching may increase range of movements, reduce spasticity, or improve walking ef ciency in children with spasticity. [5]
Static Weight-bearing Exercises[edit | edit source]
They are com- monly used in order to stimulate antigravity muscle strength, prevent hip dislocation, improve bone min- eral density, improve self-con dence, reduce spastic- ity, and improve ne motor function. [5]
Muscle Strengthening Exercises[edit | edit source]
It aims to increase the power of weak antagonist muscles and of the corre- sponding spastic agonists and to provide the functional bene ts of strengthening in children with CP. [5]
Functional Exercises[edit | edit source]
They combine aerobic and anaerobic capacity and strength training in ambulato- ry children, and signi cantly improve physical tness, the intensity of activities, and quality of life. Training programs on static bicycles or treadmill are bene cial for gait and gross motor development without enhanc- ing spasticity and abnormal movement patterns. [5]
Body Weight Supported Threadmill Training[edit | edit source]
Stepping movements (or reflex stepping reactions) are normally present in newborns and infants, before the infant starts to bear weight, stand and walk. In treadmill training, the child is supported in a harness on the treadmill in an upright posture limiting weight bearing. The child then attempts to walk on the slowly moving treadmill, eliciting the stepping movements. Treadmill training, thus allows development of stepping movements needed for ambulation. Studies using 3-4 sessions per week lasting for 3-4 months have shown improvement in lower extremity movements and gait patterns in children with cerebral palsy. [2]
Electrical Stimulation[edit | edit source]
It is proposed as a useful modality in CP due to the lack of selective muscle con- trol required for speci c strengthening programs. In par- ticular, neuromuscular and threshold electrical stimula- tion is used for strengthening the quadriceps muscles in ambulatory diplegic children with CP, who nd resistive strength training dif cult. [5]
The goal of the electrical stimulation is to increase muscle strength and motor function. Electrical stimulation is provided by TENS (transcutaneous electrical nerve stimulation) unit which is portable, non-invasive and can be used in the home–setting by parents or the patient.
Neuromuscular electrical stimulation (NMES) involves application of transcutaneous electrical current that results in muscle contraction. NMES has been postulated to increase muscle strength by increasing the cross-sectional area of the muscle and by increased recruitment of type 2 muscle fibers. Functional electrical stimulation (FES) refers to the application of electrical stimulation during a given task or activity when a specific muscle is expected to be contracting. There is evidence to support the use and effectiveness of NMES in children with CP. However, studies are limited by many confounding variables including concomitant use of other therapies, wide variation in methods of application, heterogeneity of subjects, difficulty in measuring functional outcomes and lack of control subjects. [2]
Hippotherapy
[edit | edit source]
Therapeutic horse-back riding has been shown to improve muscle tone, balance, and postural control in children with CP. Children with CP enjoy horse riding and it also provides a setting for increased social interaction and psychosocial development. [2]
Hippotherapy has been shown to improve gross motor function (tone, ROM, strength, coordination, and balance) in children with CP, which may reduce the degree of motor disability. Hippotherapy offers many potential cognitive, physical, and emotional benefits. We have noted satisfactory results with Hippotherapy in Bangalore, especially in post-surgical rehabilitation. [6]
Two lower-quality trials on saddle riding on a horse found no between-group differences in muscle sym- metry or in any of the seven different outcome measures, except on a sub-item of grasping (limited evidence). [3]
State of the Evidence[edit | edit source]
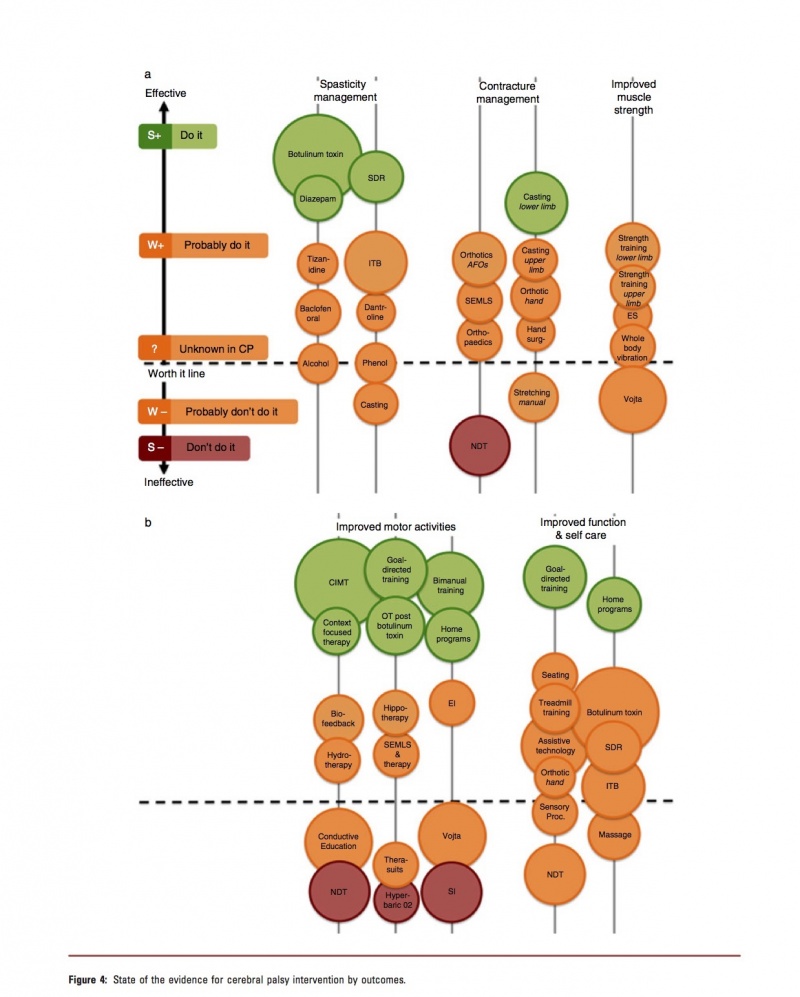
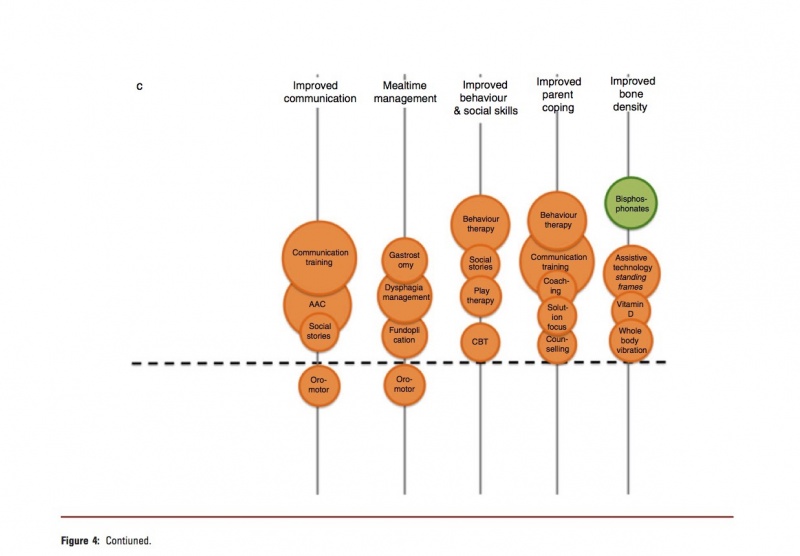
Novak et al (2013) have developed a chart based on their Systamatic Review, which looked at the State of the Evidence in relation to Interventions for the management of children with Cerebral Palsy, to assist with comparative clinical decision-making amongst intervention options for the same desired outcome. They mapped the interventions using bubble charts, with the the size of the circle correlated to the volume of published evidence. [7]
The circle size was calculated using;
- Number of published papers on the topic;
- Total score for the level of evidence (calculated by reverse coding of the Oxford Levels of Evidence, i.e. expert opinion=1, randomized controlled trial [RCT]=5).
- Location of the circle on the Y-Axis of the graph corresponds to the GRADE System Rating.
- Colour of the circle correlates to the Evidence Alert System (Fig. 4). [7]
You can review the article and more detail on their mechanism for rating the interventions at Novak I, Mcintyre S, Morgan C, Campbell L, Dark L, Morton N, Stumbles E, Wilson SA, Goldsmith S. A systematic review of interventions for children with cerebral palsy: state of the evidence. Developmental Medicine & Child Neurology. 2013 Oct 1;55(10):885-910.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1TaNXb18Y5jpzcDrSH3rPKgtDE33ORu7_rPYhd7hr7_DWI_gYf|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 Günel MK. Physiotherapy for children with cerebral palsy. INTECH Open Access Publisher; 2011.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Patel DR. Therapeutic interventions in cerebral palsy. The Indian Journal of Pediatrics. 2005 Nov 1;72(11):979-83.
- ↑ 3.0 3.1 3.2 3.3 Anttila H, Autti-Rämö I, Suoranta J, Mäkelä M, Malmivaara A. Effectiveness of physical therapy interventions for children with cerebral palsy: a systematic review. BMC pediatrics. 2008 Apr 24;8(1):1.
- ↑ Anttila H. Evidence-based perspective on CP rehabilitation: Reviews on physiotherapy, physiotherapy-related motor-based interventions and orthotic devices.
- ↑ 5.0 5.1 5.2 5.3 5.4 Mintaze Kerem G. Rehabilitation of children with cerebral palsy from a physiotherapist’s perspective. Acta Orthop Traumatol Turc. 2009;34(2):173-80.
- ↑ Sharan D. Recent advances in management of cerebral palsy. The Indian Journal of Pediatrics. 2005 Nov 1;72(11):969-73.
- ↑ 7.0 7.1 7.2 7.3 Novak I, Mcintyre S, Morgan C, Campbell L, Dark L, Morton N, Stumbles E, Wilson SA, Goldsmith S. A systematic review of interventions for children with cerebral palsy: state of the evidence. Developmental Medicine & Child Neurology. 2013 Oct 1;55(10):885-910.