Peripheral Sensitisation
Original Editor - Michelle Lee
Top Contributors - Michelle Lee, Shaimaa Eldib, Melissa Coetsee, Admin, Jo Etherton, Bruno Serra, Khloud Shreif and Mathius Kassagga
Physiological Process of Peripheral Sensitization[edit | edit source]
Following an injury or cell damage two main things can occur. Primary hyperalgesia and secondary hyperalgesia. Secondary hyperalgesia is indicative of central sensitization. [1]
Peripheral sensitization is an increased sensitivity to an afferent nerve stimuli. This occurs after there has been an injury or cell damage to the area, and produces a flare response due to nocioceptors producing lots of neuropeptides, which results in an increased sensitivity to heat and touch stimuli which is referred to as primary hyperalgesia or primary allodynia if the stimulus was not a painful one prior to the injury. For example, a gentle stroke to the skin which before the injury is not painful but after is interpreted as pain.[2][3]
Up-regulation of existing receptors:[edit | edit source]
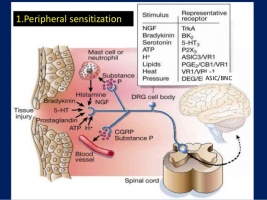
This can occur as a result of inflammation. Chemical mediators of inflammation such as histamine, bradykinn, acids and seratonin are released and can either stimulate them making them depolorize or sensitize them (bringing the membrane potential closer to the depolorization threshold).This influences the threshold is known as peripheral sensitization. This occurs when the chemical mediators stimulate the receptors on the nocioceptive terminals. This then influences the protein enzyme cascade which then up-regulates the ion channels and sodium specific nocioceptive channels.This then results in them becoming more sensitive to the chemical mediators and causes an influx of ions. This influx of ions then cause the stimulation of action potentials which then in turn produces 'pain.' [2][4][5]
In summary the nocioceptor terminals become more sensitive to the same quantity of the chemical mediators.
Up-regulation of new receptors:[edit | edit source]
The cell body which is located in the dorsal root ganglia sensory nerves produces protein channels and transmits signals to the nocioceptive terminals. When there is inflammation present as described above we also get the Nerve Growth Factor produced which transmits up tot he cell body in the dorsal root ganglia. This then also stimulates the production of ions, which as described above, stimulates the receptors on the nocioceptive terminals. Now the nociceptive terminals have a greater quantity of the 'chemical mediator' stimulating the sensation of pain more frequently.
The difference between central and peripheral sensitization can be identified quite easily, as peripheral sensitization become heat sensitive whereas central sensitization does not. Lorimer Moseley explains this in more detail in the video below.[2][6]
Take a look at these two videos. The video on the right explains peripheral and central sensitization, but first 10 minutes of the video concentrates on peripheral sensitization.
What does this Mean?[edit | edit source]
Hypersensitivity following an injury is an important self preservation mechanism, which allows the injured tissue to heal and to continuously warn / remind the brain to avoid further injury to this area. When this hypersensitivity becomes prolonged and develops into peripheral sensitization be it through either; increased sensitivity to the chemical modulators or a decreased threshold to the stimulus provides the body with no benefit. peripheral sensitization is important to identify in patients as this can have an impact on treatment and their experience of pain as assessment through touch or movement may stimulate an unexpected level of pain. Peripheral sensitization manifests it's symptoms similarly to central sensitization. [7]
References[edit | edit source]
- ↑ Pezet S, McMahon SB. Neurotrophins: mediators and modulators of pain. Annu. Rev. Neurosci.. 2006 Jul 21;29:507-38..
- ↑ 2.0 2.1 2.2 Bolay H, Moskowitz MA. Mechanisms of pain modulation in chronic syndromes. Neurology. 2002 Sep 10;59(5 suppl 2):S2-7.
- ↑ Graven-Nielsen T, Arendt-Nielsen L. Peripheral and central sensitization in musculoskeletal pain disorders: an experimental approach. Current rheumatology reports. 2002 Aug 1;4(4):313-21.
- ↑ Staud R, Smitherman ML. Peripheral and central sensitization in fibromyalgia: pathogenetic role. Current pain and headache reports. 2002 Aug 1;6(4):259-66.
- ↑ Van Griensven H, Strong J, Unruh A. Pain: a textbook for health professionals. Churchill Livingstone; 2013 Nov 1.
- ↑ Mizumura KA. Peripheral mechanism of hyperalgesia-sensitization of nociceptors. Nagoya journal of medical science. 1997 Nov 1;60:69-88.
- ↑ Van Griensven H, Strong J, Unruh A. Pain: a textbook for health professionals. Churchill Livingstone; 2013 Nov 1.