Pelvic Floor Anatomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
= The Pelvic Floor - Overview and Function = | = The Pelvic Floor - Overview and Function <ref name="Wiki">Wikipedia. Pelvic floor. http://en.wikipedia.org/wiki/Pelvic_floor. (accessed 6 April 2014).</ref> = | ||
The pelvic floor is an area of muscle and connective tissue that spans the area underneath the pelvis, separating the pelvic cavity above from the perineal region below. It provides support to the pelvic viscera including the bladder, intestines and uterus (in females). It also assists with continence through control of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. Finally , it helps to maintain optimal intraabdominal pressure. | The pelvic floor is an area of muscle and connective tissue that spans the area underneath the pelvis, separating the pelvic cavity above from the perineal region below. It provides support to the pelvic viscera including the bladder, intestines and uterus (in females). It also assists with continence through control of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. Finally , it helps to maintain optimal intraabdominal pressure. | ||
| Line 37: | Line 37: | ||
*Rectovaginal septum | *Rectovaginal septum | ||
== Pelvic Floor Myology <ref name="Netter" /> == | == Pelvic Floor Myology <ref name="Netter" /><ref name="Wiki" /> == | ||
[[Image:Pelvic floor.png|thumb|right|300px|Pelvic Floor]] | [[Image:Pelvic floor.png|thumb|right|300px|Pelvic Floor]] | ||
| Line 124: | Line 124: | ||
|} | |} | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 19:23, 6 April 2014
The Pelvic Floor - Overview and Function [1][edit | edit source]
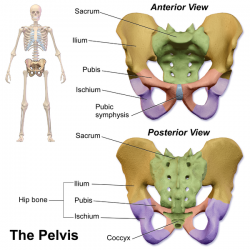
The pelvic floor is an area of muscle and connective tissue that spans the area underneath the pelvis, separating the pelvic cavity above from the perineal region below. It provides support to the pelvic viscera including the bladder, intestines and uterus (in females). It also assists with continence through control of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. Finally , it helps to maintain optimal intraabdominal pressure.
Osteology, Ligaments and Fascia
[edit | edit source]
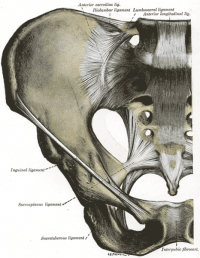
Ligaments[2]
Puboprostatic ligament
Pubovesical ligament
Sacrogenital ligaments
Pelvic Fascia[2]
Parietal pelvic fascia - lines the internal surface of the muscles of the pelvic floor and walls
Visceral pelvic fascia - invests each pelvic organ
The parietal and visceral fascia are continuous where organs penetrate the pelvic floor. They thicken to form the arcus tendineus, arches of fascia running adjacent to the viscera from the pubis to the sacrum.
Endopelvic fascia - "filler" material lying bewteen the parietal and visceral fascia, sometimes condensing to form fibrous fascial septa which separate the organs.
- Hypogastric sheath - separates retropubic space from presacral space; conduit for vessels and nerves
- Transverse cerical (cardinal) ligaments - part of hypogastric sheath; runs from lateral pelvic wall to uterine cervix and vagina; transmits uterine artery and provides passive support for the uterus
- Vesicovaginal septum
- Rectovesical septum
- Rectovaginal septum
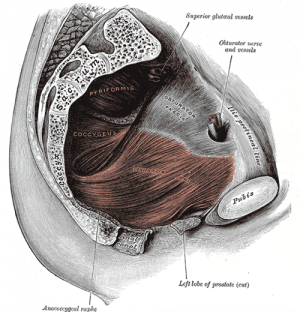
Pelvic Floor Myology [2][1][edit | edit source]
Pelvic diaphragm
- Levator ani - pubococcygeus, puborectalis, iliococcygeus
- Ischiococcygeus (Coccygeus)
Sphincter urethrae
Perineal membrane
Superficial genital muscles;
- Bulbocavernosus (bulbospongiosus in men)
- Ischiocavernosus
- Superficial transverse perineal
Associated muscles;
- Piriformis
- Obturator internus
- Adductors
- Gluteals
- Transverse abdominus
- Multifidus
- Respiratory diaphragm
| Muscle | Origin | Insertion | Action | Innervation |
| Levator Ani (Pubococcygeus) | Posterior aspect of body of pubis and anterior part of arcus tendineus | Coccyx and anococcygeal ligament | Helps to support pelvic viscera and resists increase in intra-abdominal pressure | Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus
|
| Levator Ani (Iliococcygeus) | Posterior aspect of arcus tendineus and the ischial spine | Anococcygeal raphe and the coccyx | Helps to support pelvic viscera and resists increase in intra-abdominal pressure | Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus
|
| Levator Ani (Puborectalis) | Lower part of pubic symphysis and superior fascia of urogenital diaphragm | Unites with its partner to make a U-shaped sling around the rectum | Controls defecation by pulling anorectal junction forward | Nerve to levator ani (branches of S4), branch of pudendal nerve (S2-4)
|
| Ischiococcygeus (Coccygeus) | Ischial Spine | Lower two sacral and upper two coccygeal spinal segments, blends with sacrospinous ligament on its external surface | Supports pelvic viscera, flexion of coccyx | Anterior rami of S4 and S5 |
| Sphincter urethrae | Controls flow of urine through urethra | |||
References[edit | edit source]
- ↑ 1.0 1.1 Wikipedia. Pelvic floor. http://en.wikipedia.org/wiki/Pelvic_floor. (accessed 6 April 2014).
- ↑ 2.0 2.1 2.2 Netter Anatomy. Pelvis and perineum: pelvic floor and contents. http://www.netteranatomy.com/anatomylab/subregions.cfm?subregionID=R53. (accessed 6 April 2014).