Parkinson's Lifestyle Medicine - Wellness and Lifestyle Strategies
Original Editor - Thomas Longbottom based on the course by Z Altug
Top Contributors - Thomas Longbottom, Kim Jackson, Wanda van Niekerk, Jess Bell, Tarina van der Stockt and Jorge Rodríguez Palomino
Introduction[edit | edit source]
Approximately 10 million people around the world are currently living with Parkinson’s Disease.[1] Meta-analysis of worldwide data reveals that the prevalence of Parkinson’s Disease increases with age, quadrupling from a level of almost 0.5% in the seventh decade of life to approximately 2% for those over the age of 80.[2] Other sources report that Parkinson's affects 1.5-2% of the population over the age of 60.[3] Parkinson’s is associated with the loss of dopamine-producing neurons in the substantia nigra of the midbrain, and it is typified clinically by resting tremor, rigidity, and bradykinesia along with a number of non-motor features such as anosmia, sleep behaviour disorder, depression, autonomic dysfunction, and cognitive dysfunction.[4] The aetiology of this disease is not fully understood, but there is some combination of environmental and genetic factors presumed to be causative.[4] Among these are various lifestyle factors such as tobacco use, dietary intake, and physical activity.[5][6]
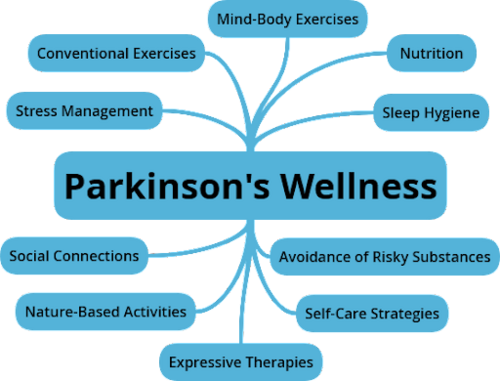
According to the Lifestyle Medicine Handbook, Lifestyle Medicine involves the use of evidence-based lifestyle therapeutic approaches to treat, reverse, and prevent lifestyle-related chronic disease.[8] These include:
- A predominantly whole food, plant-based diet
- Regular physical activity
- Adequate sleep
- Stress management
- Social connections
- Avoidance of risky substance abuse[8]
The aim of Lifestyle Medicine is to treat the underlying causes of disease rather than just addressing the symptoms. This involves helping patients learn and adopt healthy behaviours. Lifestyle interventions have the potential to impact the prognosis of many chronic diseases, leading not only to better quality of life for many but also potentially reducing their costs to the healthcare system.[9] While a tendency to think of Lifestyle Medicine as being the domain of the physician is understandable, other providers such as dietitians, social workers, behavioural therapists and lifestyle coaches are also integral.[9] It is also well within the scope of the physiotherapist, with diet and nutrition being key elements in many of the conditions managed by physiotherapists, with physiotherapists poised as experts in exercise and movement, and with prevention, health promotion, fitness and wellness being crucial aspects of physiotherapy care.[10]
The focus of this module will be on discussing strategies for persons with Parkinson's related to stress management, the avoidance of risky substance abuse, and the improvement of social connections, along with the benefits of being in outdoor environments.
Strategies for Stress Management[edit | edit source]
What is stress? Per Taber's Cyclopedic Medical Dictionary, it is "any physical, physiological or psychological force that disturbs equilibrium."[3] These disturbances in a person with Parkinson's Disease can have some particular effects. Stress can reduce the effectiveness of levodopa in the medical management of persons with Parkinson's Disease.[11] The ability to cope with stress may help prevent exacerbations of parkinsonian tremors caused by the stress.[12] Chronic stress also has the potential to increase susceptibility to depression and anxiety in persons with Parkinson's.[13] Strategies for stress management can thus be impactful for the person with Parkinson's.
What causes stress? Determining the factors creating stress can be the first step in managing it. Consider the following potential causes of stress:
- Financial concerns
- Family matters
- Work matters, including long commutes to work
- Medical concerns, including lack of quality information regarding the medical condition
- Personal relationships
- Lack of socialization
- Pressure while studying or preparing for a career
- Facing major life changes, such as losing a loved one, changing jobs, or moving to another location
- Times of uncertainty, such as a living during a global pandemic
What are some strategies to manage stress? Once the source of the stress is identified, select strategies may be applied to manage that stress. However, it is important to realize that not all approaches will be appropriate for every person.
Sample patient education strategies to help manage stress:
- Try conventional exercise such as walking, biking, hiking, swimming, etc.
- Try mind body exercise such as tai chi, qigong, or yoga.
- Try engaging in more outdoor activities.
- Try various types of meditation.
- Try progressive muscle relaxation techniques.
- Try massage therapy.
- Try listening to music.
- Try guided imagery with music.
- Try painting or drawing.
- Try including more laughter into daily life through television, books, or other media.
- Try singing, whistling, or humming.
- Try dancing.
- Try participating in a drama class at a local school or community theatre.
- Try a weighted blanket.
- Try playing with pets.
Reducing Risky Substance Abuse[edit | edit source]
Improving Social Connections[edit | edit source]
Benefits of Outdoor Environments[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Statistics [Internet]. Parkinson's Foundation. [cited 2021Dec28]. Available from: https://www.parkinson.org/Understanding-Parkinsons/Statistics
- ↑ Pringsheim T, Jette N, Frolkis A, Steeves TDL. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Movement Disorders 2014;29(13):1583–90.
- ↑ 3.0 3.1 Venes D, Taber CW. Taber's Cyclopedic Medical Dictionary. Philadelphia, PA: F.A. Davis; 2021.
- ↑ 4.0 4.1 Simon DK, Tanner CM, Brundin P. Parkinson Disease Epidemiology, Pathology, Genetics, and Pathophysiology. Clinics in Geriatric Medicine 2020;36(1):1–2.
- ↑ Ritz B, Ascherio A, Checkoway H, Marder KS, Nelson LM, Rocca WA, et al.. Pooled Analysis of Tobacco Use and Risk of Parkinson Disease. Archives of Neurology [Internet] 2007;64(7):990.
- ↑ Paul KC, Chuang Y, Shih I, Keener A, Bordelon Y, Bronstein JM, et al.. The association between lifestyle factors and Parkinson's disease progression and mortality. Movement Disorders 2019;34(1):58–66.
- ↑ Z Altug. Parkinson's Lifestyle Medicine - Nutrition and Sleep Hygiene. Physioplus Course. 2021.
- ↑ 8.0 8.1 Frates B, Bonnet JP, Joseph R, Peterson JA. Lifestyle Medicine Handbook: An introduction to the power of Healthy Habits. Monterey, CA: Healthy Learning; 2021.
- ↑ 9.0 9.1 1. Bodai B. Lifestyle Medicine: A Brief Review of Its Dramatic Impact on Health and Survival. The Permanente Journal 2017;22(1).
- ↑ Worman R. Lifestyle medicine: The role of the physical therapist. The Permanente Journal. 2020;24:18.192.
- ↑ 1. Zach H, Dirkx MF, Pasman JW, Bloem BR, Helmich RC. Cognitive Stress Reduces the Effect of Levodopa on Parkinson's Resting Tremor. CNS Neuroscience & Therapeutics 2017;23(3):209–15.
- ↑ Jankovic Joseph. Physiologic and pathologic tremors. Annals of Internal Medicine. 1980;93(3):460.
- ↑ Heide A, Meinders MJ, Speckens AEM, Peerbolte TF, Bloem BR, Helmich RC. Stress and mindfulness in parkinson's disease: Clinical effects and potential underlying mechanisms. Movement Disorders. 2020;36(1):64–70.







