Parkinson's Lifestyle Medicine - Wellness and Lifestyle Strategies: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Approximately 10 million people around the world are currently living with Parkinson’s Disease.<ref>Statistics [Internet]. Parkinson's Foundation. [cited 2021Dec28]. Available from: https://www.parkinson.org/Understanding-Parkinsons/Statistics</ref> Meta-analysis of worldwide data reveals that the prevalence of Parkinson’s Disease increases with age, quadrupling from a level of almost 0.5% in the seventh decade of life to approximately 2% for those over the age of 80.<ref>Pringsheim T, Jette N, Frolkis A, Steeves TDL. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Movement Disorders 2014;29(13):1583–90.</ref> Other sources report that Parkinson's affects 1.5-2% of the population over the age of 60.<ref>Venes D, Taber CW. Taber's Cyclopedic Medical Dictionary. Philadelphia, PA: F.A. Davis; 2021.</ref> Parkinson’s is associated with the loss of dopamine-producing neurons in the substantia nigra of the midbrain, and it is typified clinically by resting tremor, rigidity, and bradykinesia along with a number of non-motor features such as anosmia, sleep behaviour disorder, depression, autonomic dysfunction, and cognitive dysfunction.<ref name=":0">Simon DK, Tanner CM, Brundin P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6544143/?report=classic Parkinson Disease Epidemiology, Pathology, Genetics, and Pathophysiology]. Clinics in Geriatric Medicine 2020;36(1):1–2.</ref> The aetiology of this disease is not fully understood, but there is some combination of environmental and genetic factors presumed to be causative.<ref name=":0" /> Among these are various lifestyle factors such as tobacco use, dietary intake, and physical activity.<ref>Ritz B, Ascherio A, Checkoway H, Marder KS, Nelson LM, Rocca WA, et al.. [https://jamanetwork.com/journals/jamaneurology/fullarticle/794179 Pooled Analysis of Tobacco Use and Risk of Parkinson Disease]. Archives of Neurology [Internet] 2007;64(7):990.</ref><ref>Paul KC, Chuang Y, Shih I, Keener A, Bordelon Y, Bronstein JM, et al.. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6544143/?report=classic The association between lifestyle factors and Parkinson's disease progression and mortality]. Movement Disorders 2019;34(1):58–66.</ref> | |||
== | == Lifestyle Medicine == | ||
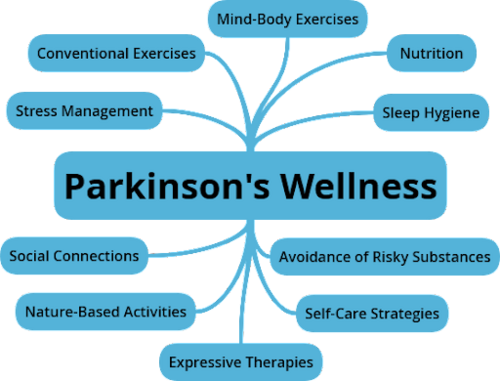
[[File:Parkinsons Wellness Diagram.png|alt=Components of Parkinson's Lifestyle Wellness: Stress Management, Conventional Exercise, Mind-Body Exercise, Nutrition, Sleep Hygiene, Avoidance of Risky Substances, Self-Care Strategies, Expressive Therapies, Nature-Based Activities, and Social Connections|thumb|500x500px|Components of Parkinson's Lifestyle Wellness<ref name=":2">Z Altug. Parkinson's Lifestyle Medicine - Nutrition and Sleep Hygiene. Physioplus Course. 2021.</ref>]] | |||
According to the Lifestyle Medicine Handbook, Lifestyle Medicine involves the use of evidence-based lifestyle therapeutic approaches to treat, reverse, and prevent lifestyle-related chronic disease.<ref name=":1">Frates B, Bonnet JP, Joseph R, Peterson JA. Lifestyle Medicine Handbook: An introduction to the power of Healthy Habits. Monterey, CA: Healthy Learning; 2021.</ref> These include: | |||
#A predominantly whole food, plant-based diet | |||
#Regular physical activity | |||
#Adequate sleep | |||
#Stress management | |||
#Social connections | |||
#Avoidance of risky substance abuse<ref name=":1" /> | |||
The aim of Lifestyle Medicine is to treat the underlying causes of disease rather than just addressing the symptoms. This involves helping patients learn and adopt healthy behaviours. Lifestyle interventions have the potential to impact the prognosis of many chronic diseases, leading not only to better quality of life for many but also potentially reducing their costs to the healthcare system.<ref name=":4">1. Bodai B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5638636/ Lifestyle Medicine: A Brief Review of Its Dramatic Impact on Health and Survival]. The Permanente Journal 2017;22(1).</ref> While a tendency to think of Lifestyle Medicine as being the domain of the physician is understandable, other providers such as dietitians, social workers, behavioural therapists and lifestyle coaches are also integral.<ref name=":4" /> It is also well within the scope of the physiotherapist, with diet and nutrition being key elements in many of the conditions managed by physiotherapists, with physiotherapists poised as experts in exercise and movement, and with prevention, health promotion, fitness and wellness being crucial aspects of physiotherapy care.<ref>Worman R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7015533/ Lifestyle medicine: The role of the physical therapist]. The Permanente Journal. 2020;24:18.192.</ref> | |||
The focus of this module will be on discussing strategies for persons with Parkinson's related to '''stress management''', the '''avoidance of risky substance abuse''', and the '''improvement of social connections''', along with the '''benefits of being in outdoor environments'''. | |||
== Sub Heading 3 == | == Sub Heading 3 == | ||
Revision as of 02:58, 30 December 2021
Original Editor - Thomas Longbottom based on the course by Z Altug
Top Contributors - Thomas Longbottom, Kim Jackson, Wanda van Niekerk, Jess Bell, Tarina van der Stockt and Jorge Rodríguez Palomino
Introduction[edit | edit source]
Approximately 10 million people around the world are currently living with Parkinson’s Disease.[1] Meta-analysis of worldwide data reveals that the prevalence of Parkinson’s Disease increases with age, quadrupling from a level of almost 0.5% in the seventh decade of life to approximately 2% for those over the age of 80.[2] Other sources report that Parkinson's affects 1.5-2% of the population over the age of 60.[3] Parkinson’s is associated with the loss of dopamine-producing neurons in the substantia nigra of the midbrain, and it is typified clinically by resting tremor, rigidity, and bradykinesia along with a number of non-motor features such as anosmia, sleep behaviour disorder, depression, autonomic dysfunction, and cognitive dysfunction.[4] The aetiology of this disease is not fully understood, but there is some combination of environmental and genetic factors presumed to be causative.[4] Among these are various lifestyle factors such as tobacco use, dietary intake, and physical activity.[5][6]
Lifestyle Medicine[edit | edit source]
According to the Lifestyle Medicine Handbook, Lifestyle Medicine involves the use of evidence-based lifestyle therapeutic approaches to treat, reverse, and prevent lifestyle-related chronic disease.[8] These include:
- A predominantly whole food, plant-based diet
- Regular physical activity
- Adequate sleep
- Stress management
- Social connections
- Avoidance of risky substance abuse[8]
The aim of Lifestyle Medicine is to treat the underlying causes of disease rather than just addressing the symptoms. This involves helping patients learn and adopt healthy behaviours. Lifestyle interventions have the potential to impact the prognosis of many chronic diseases, leading not only to better quality of life for many but also potentially reducing their costs to the healthcare system.[9] While a tendency to think of Lifestyle Medicine as being the domain of the physician is understandable, other providers such as dietitians, social workers, behavioural therapists and lifestyle coaches are also integral.[9] It is also well within the scope of the physiotherapist, with diet and nutrition being key elements in many of the conditions managed by physiotherapists, with physiotherapists poised as experts in exercise and movement, and with prevention, health promotion, fitness and wellness being crucial aspects of physiotherapy care.[10]
The focus of this module will be on discussing strategies for persons with Parkinson's related to stress management, the avoidance of risky substance abuse, and the improvement of social connections, along with the benefits of being in outdoor environments.
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Statistics [Internet]. Parkinson's Foundation. [cited 2021Dec28]. Available from: https://www.parkinson.org/Understanding-Parkinsons/Statistics
- ↑ Pringsheim T, Jette N, Frolkis A, Steeves TDL. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Movement Disorders 2014;29(13):1583–90.
- ↑ Venes D, Taber CW. Taber's Cyclopedic Medical Dictionary. Philadelphia, PA: F.A. Davis; 2021.
- ↑ 4.0 4.1 Simon DK, Tanner CM, Brundin P. Parkinson Disease Epidemiology, Pathology, Genetics, and Pathophysiology. Clinics in Geriatric Medicine 2020;36(1):1–2.
- ↑ Ritz B, Ascherio A, Checkoway H, Marder KS, Nelson LM, Rocca WA, et al.. Pooled Analysis of Tobacco Use and Risk of Parkinson Disease. Archives of Neurology [Internet] 2007;64(7):990.
- ↑ Paul KC, Chuang Y, Shih I, Keener A, Bordelon Y, Bronstein JM, et al.. The association between lifestyle factors and Parkinson's disease progression and mortality. Movement Disorders 2019;34(1):58–66.
- ↑ Z Altug. Parkinson's Lifestyle Medicine - Nutrition and Sleep Hygiene. Physioplus Course. 2021.
- ↑ 8.0 8.1 Frates B, Bonnet JP, Joseph R, Peterson JA. Lifestyle Medicine Handbook: An introduction to the power of Healthy Habits. Monterey, CA: Healthy Learning; 2021.
- ↑ 9.0 9.1 1. Bodai B. Lifestyle Medicine: A Brief Review of Its Dramatic Impact on Health and Survival. The Permanente Journal 2017;22(1).
- ↑ Worman R. Lifestyle medicine: The role of the physical therapist. The Permanente Journal. 2020;24:18.192.






