Parkinson's - Physiotherapy Referral and Assessment
Original Editor - Bhanu Ramaswamy as part of the APPDE Project
Top Contributors - Kim Jackson, Mariam Hashem, Wendy Walker, Laura Ritchie, Rachael Lowe, Tarina van der Stockt, Stacy Schiurring, Oyemi Sillo, Lauren Lopez, Jess Bell, Chelsea Mclene, 127.0.0.1, Tony Lowe, Leana Louw, Admin, Naomi O'Reilly and WikiSysop
Introduction[edit | edit source]
Physiotherapists play a vital role in supporting people with Parkinson’s Disease to choose management strategies, prioritise and address the challenges they face over the course of the condition. Improving movement and safety is usually the main focus of physiotherapy in light of the progressive pathology and the disability and participation restrictions this can cause.
Referral[edit | edit source]
The American Academy of Neurology recommend the clinicians discuss the clinical presentations of the individual with Parkinson’s at least once yearly with a physiotherapist to consider when would be an optimal time to refer the person for physiotherapy services. An ideal best practice standard would be for the physiotherapist to have Parkinson’s expertise, and to be involved at the point of diagnosis. This does not always occur and until such time as we are referred all people with Parkinson’s, some referral criteria have been agreed.
Assessment[edit | edit source]
Physiotherapy assessment considers ways in which the condition is affecting the individual with Parkinson’s, whilst being aware of the impact on close carers and relatives, especially when someone is newly diagnosed or has been diagnosed for some time.
The history taking and physical assessment aspects of the assessment enable an honest discussion of what is realistic of the things the person wants to do. The core areas of physiotherapy interventions for which there is evidence of effectiveness for people with Parkinson’s are:
Physical capacity[edit | edit source]
It is known that people with Parkinson’s are less active than their peers as the condition progresses, resulting in muscle weakness and power, increased falls risk and reduced walking speed, itself an indication of reduced life expectancy. Physiotherapist must understand the importance of education on staying active and develop a management plan that tackles all physical problems that result in reduced activity levels.
Transfers[edit | edit source]
Difficulties arise for people with Parkinson’s due to the complexity of changing position – e.g. rising from lying or sitting, turning activities
Manual activities[edit | edit source]
These become difficulty due to the combination of sequential sub-tasks, dexterity and co-ordination requirements
Quality of Movement[edit | edit source]
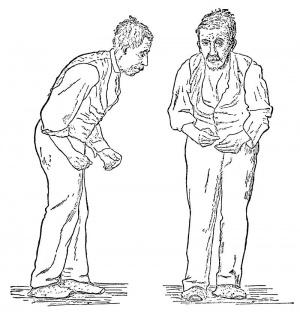
Parkinson's is associated with different movement patterns which are associated with functional decline on the long-term:
- Dyskinesia : rapid, random, jerky movement
- Freezing: where the person cannot move – either to start a movement (or speech), or where they come to a halt
- Festnaton: involuntary gait quickening
- Dystonia: sustained muscle contractions (can cause abnormal postures and be painful)
- Falling: often during complex movement e.g.turning, or misjudging clearance.
- Bradykinesia: longer latencies for muscle force production and relaxation, initially affecting power and strength
Posture[edit | edit source]
Varied postural changes are common among people with PD including:
- Camptocormia: an involuntary forward flexion (usually greater than 45°) when person is upright, that reduces/ disappears when the person lies down.
- Antecollis: forward flexion of head and neck
- Pisa syndrome: a sustained lateral flexion of the trunk; not necessarily to the Parkinson’s dominant side
postural flexion changes affect the quality of life and make people more prone to vertebral fractures.
Balance & Falls[edit | edit source]
| [1] |
Balance impairment and falls (30-70% of people with PD experience falls) are common problems for people with Parkinson’s; these problems often start after about 5 years of diagnosis due to worsening of the systems that maintain body position, the progressive slowness of movement, trunk rigidity and reduced proprioception.
The following factors are considered to be risk factors and predictors of falls in PD[2]:
- Age
- Length since Parkinson’s onset,
- Associated neuro-musculo-skeletal changes
- Reduced leg muscle strength
- Proprioception and gait speed changes
- Increased gait variability
- Freezing of gait
A thorough assessment of each possible factor contributing to the likelihood of falls is essential, putting in mind other factors such as cognition and strategy selection, quality of life misjudgment and distraction, fear of falling, personal factors and environment[3]. Considering different factors when designing a rehabilitation program should yield positive outcomes and reduce the risk of falls[3].
Falling has wide ranging impact including risk of fractures (especially hips and wrist), carer stress and fear of movement.
Gait[edit | edit source]
People with Parkinson's Disease require assessment of continuous or episodic problems with gait.
Impaired speed-distance and amplitude scaling; inadequate burst duration and reduced burst amplitude result in walking slower
Disease Progression[edit | edit source]
As the condition progresses, the individual’s needs, and our physiotherapy goals will alter; it is essential that the person is reviewed regularly.
Early Stages[edit | edit source]
In the early stages of the condition, physiotherapy assessment should aim to support educational needs e.g. about keeping fit, active and healthy, and on minimising the impact Parkinson’s on people’s lives. As Parkinson’s progresses and the individual experiences problems with their movement, the assessment focus moves towards a review of physical activity and mobility, possibly assessing for the optimal movement and cognitive strategies.
Late Stages[edit | edit source]
In the later stages, as the condition progresses, many of the symptoms of Parkinson’s have a bigger impact on daily life, often mixing with other medical conditions. Physiotherapy assessment focuses on decisions about how to cope with these changes with an emphasis on a support network to best keep the person active and safe when moving.
Other issues physiotherapists should assess for are pain and respiratory problems.
Associated respiratory problems with Parkinson's require acute care intervention[4]. Shortness of breath on exertion is reported by 35.8%Patients, cough and sputum production were reported by 17. 9% and 13% respectively[5]. Whenever a symptoms of ventilatory dysfunction is present, pulmonary function test is recommended to identify the dimensions of the problem and tackle it with a proper care plan[4].
Pain is a multi-dimensional phenomenon and could be assessed using different measuring scales and questionnaires to include in the management plan. 30 to 50% of PD patients experience pain[6] mainly musculoskeletal pain in the neck, arm, paraspinal or calf muscles. MSK pain is more likely to be caused by rigidity. Radicular and neuropathic pain are experienced by 5-20% of PD patients. Dystonic pain, restless leg syndrome and akathitic. discomfort were reported to be associated with PD.
Physiotherapy Guidelines[edit | edit source]
In terms of an easy access on-line resource, we advise to you to read the Review version of the European Physiotherapy Guideline for Parkinson’s Disease. Although the title intimates ‘European’, the evidence informing the document is taken from international studies and input from worldwide experts. The Guideline is an update of the first evidence-based guideline with practice recommendations for physiotherapy in Parkinsons’s was published by the Royal Dutch society for Physical Therapy (KNGF), the ‘Dutch Guidelines’..
The Association of Physiotherapists in Parkinson's Europe (APPDE) requested the update, the KNGF agreed with ParkinsonNet (a community of healthcare professionals specialised in Parkinson's) to update and adapt the guideline into a European guideline for physiotherapy in Parkinson’s. The development is endorsed by the APPDE, the European Region of the World Confederation for Physical Therapy (ER-WCPT) the European Parkinson’s Disease Association (EPDA). Nineteen member organisations of the ER-WCPT, as well as people with Parkinson’s and their representatives participated in the development process of the European Guideline. The classification system of the International Classification of Functioning, Disability and Health (ICF classification) is used. This framework provides a common language and basis for understanding and describing health and health-related problems. The aim of using this common language is to improve communication about functioning of individuals with Parkinson’s between health and social care workers, researchers and social policy makers.
The Guideline is intended to be helpful to “all involved in Parkinson care who, supporting evidence-based, patient centred care", and therefore has beendivided into four parts:
- The Guideline, mainly for physiotherapists. This is the one we refer to in this Project and included the background on Parkinson's disease and health management, physiotherapy core areas and rationale and evidence for categories of interventions
- Information for people with Parkinson's: Includes self-management support and how to get the best out of physiotherapy care
- Information for clinicians: when to refer to physiotherapy and what to expect
- Information to the development and scientific justification of the Guideline: insight in the barriers and facilitators of current care and details to measurement tools and the GRADE-based recommendations
In the Guideline:
- Appendix 4 on page 103 provides an ICF assessment and report form; Appendix 9 on page 155 provides a list of Parkinson’s-related ICF domains, and Appendix 10 on page 156 provides the most appropriate measurement tools validated with Parkinson’s populations according to the ICF domains.
- Chapter 4 (pages 32 - 41) concentrates on the core areas of physiotherapy for people with Parkinson’s
- Chapter 5 (pages 42 - 63) is on history taking and physical examination
- Chapter 6 (pages 64 – 91) provides ideas on the rationale and evidence for physiotherapy interventions
Medication[edit | edit source]
Understanding the impact of medication on both the movement and thought quality of people with Parkinson’s will help set goals and plans for physiotherapy intervention. Individual Parkinson’s Associations provide country-specific information about medications prescribed. E.g. In the UK, where physiotherapists can train to prescribe medication, a good summary of drug therapies can be found on the Parkinson’s UK site and in the US, the National Parkinson’s Foundation provides advice.
Physiotherapeutic treatment techniques[edit | edit source]
Look at various videos demonstrating different physical therapies:
| [7] | [8] | [9] |
| [10] | [11] | [12] |
| [13] | [14] | [15] |
Related pages[edit | edit source]
- Parkinson's Disease
- Parkinson's Disease - Clinical Presentation
- Parkinson's Disease - Anatomy, Pathology, Prognosis and Diagnosis
- Physiotherapy - Management and Interventions
- Outcome Measures
- Key Evidence and resources
References[edit | edit source]
- ↑ UMHealthSystem. Parkinson's Disease - Balance, Falls & Cognition: Roger Albin. Available from: http://www.youtube.com/watch?v=NtMri6DzltU [last accessed 29/09/16]
- ↑ Paul SS, Allen NE, Sherrington C, Heller G, Fung VS, Close JC, Lord SR, Canning CG. Risk factors for frequent falls in people with Parkinson's disease. Journal of Parkinson's disease. 2014 Jan 1;4(4):699-703.
- ↑ 3.0 3.1 Hulbert S, Rochester L, Nieuwboer A, Goodwin V, Fitton C, Chivers-Seymour K, Ashburn A. Staying safe”–a narrative review of falls prevention in people with Parkinson’s–“PDSAFE. Disability and rehabilitation. 2018 May 11:1-0.
- ↑ 4.0 4.1 O’Callaghan A, Walker R. A review of pulmonary function in Parkinson’s disease. Journal of Parkinsonism and Restless Legs Syndrome. 2018 Jan 1;8:13-23.
- ↑ Lee MA, Prentice WM, Hildreth AJ, Walker RW. Measuring symptom load in Idiopathic Parkinson's disease. Parkinsonism & related disorders. 2007 Jul 1;13(5):284-9.
- ↑ Beiske AG, Loge JH, Rønningen A, Svensson E. Pain in Parkinson’s disease: prevalence and characteristics. Pain 2009;141:173e7.
- ↑ TouroInfirmary. LSVT Big & Loud Parkinson's Therapy at Touro Neuro Rehab Center. Available from: http://www.youtube.com/watch?v=9fUQ6jptaBY [last accessed 29/09/16]
- ↑ Advance Rehab Centre. LSVT Big. Available from: http://www.youtube.com/watch?v=3jPEtanYmI0 [last accessed 29/09/16]
- ↑ UStepWalker. The U-Step 2 Walker, a Parkinson's Therapy Aid. Available from: http://www.youtube.com/watch?v=mirtZhHJSB4 [last accessed 29/09/16]
- ↑ **. Available from: http://www.youtube.com/watch?v=pL_LZgAEsnM [last accessed 29/09/16]
- ↑ SusieG5678. Dancing Feet Help Defeat Parkinson's. Available from: http://www.youtube.com/watch?v=koaA1T0MynM [last accessed 29/09/16]
- ↑ Tom Anthony. Dancing helps Parkinson's Patients. Available from: http://www.youtube.com/watch?v=UEAaWPHDRbk [last accessed 29/09/16]
- ↑ 205beers. Exercise program for Parkinson disease. Available from: http://www.youtube.com/watch?v=YEiupqJDugA [last accessed 29/09/16]
- ↑ captainpat. Parkinson's Disease - Vigorous Exercise. Neil Sligar June 2011. Available from: http://www.youtube.com/watch?v=R_-nRQmO8ko [last accessed 29/09/16]
- ↑ Polestar Pilates. Polestar Pilates for Parkinson's Disease Patients. Available from: http://www.youtube.com/watch?v=yWBn0Ozt2fU [last accessed 29/09/16]