Parkinson's - Physiotherapy Management and Interventions: Difference between revisions
Wendy Walker (talk | contribs) No edit summary |
Wendy Walker (talk | contribs) No edit summary |
||
| Line 30: | Line 30: | ||
We can see immediately the effects of external cueing and attention on improving step length, freezing and turning during walking tasks, and in activities of daily living. | We can see immediately the effects of external cueing and attention on improving step length, freezing and turning during walking tasks, and in activities of daily living. | ||
Depending on the cognitive state of the individual, they may be able to learn how to self-instruct in the use of an internal cue or strategy. If less able, the cue or strategy has to come from an external source e.g. a visual strip on the ground, the rhythmic beat of a metronome. <br><br>Depending on the stage of the condition, the rationale for intervention choices will differ: | Depending on the cognitive state of the individual, they may be able to learn how to self-instruct in the use of an internal cue or strategy. If less able, the cue or strategy has to come from an external source e.g. a visual strip on the ground, the rhythmic beat of a metronome. <br><br>Depending on the stage of the condition, the rationale for intervention choices will differ: | ||
[[Image: | [[Image:Parkinsons Interventions Chart.png|600px]]<br> | ||
This figure has been copied with permission of Lynn Rochester on behalf of Rochester, Nieuwboer and Lord (2011).<br> | This figure has been copied with permission of Lynn Rochester on behalf of Rochester, Nieuwboer and Lord (2011).<br> | ||
As mentioned in the subsection on Physiotherapy for Parkinson’s: [[ | As mentioned in the subsection on Physiotherapy for Parkinson’s: [[Parkinsons Physiotherapy - Referral and Assessment|Referral and assessment]], during the earlier stages of diagnosis, greater emphasis is placed on education and self-management. The individual should be encouraged to continue being active and participate in physical exercise for as long as possible. Significant respiratory complications develop in many people as their Parkinson’s progresses, so attention should be paid to monitor and manage encroaching weakness of respiratory muscles and rigidity of the thoracic cage.<br>The European Guideline provides a section that describes the use of motor learning (pages 52 – 55), expectations if practiced and executed as a strategy to train improvements in movement. It takes the form of cued functional and dual task training, compensatory strategy training uses external cues, self-instruction and attention. Examples include: | ||
*Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing | *Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing | ||
*Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk | *Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk | ||
*Attention – Thinking about taking a big step; making a wider arc turn | *Attention – Thinking about taking a big step; making a wider arc turn | ||
*Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backwards as a cue ready to then walk forwards | *Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backwards as a cue ready to then walk forwards | ||
Most people who are diagnosed with Parkinson’s are aged 50 or over, but 1 in 20 of those diagnosed are younger than this. Those with young onset Parkinson’s are more likely to exhibit early dystonia and motor fluctuations and dyskinesias, caused by prolonged use of dopaminergic treatment. | Most people who are diagnosed with Parkinson’s are aged 50 or over, but 1 in 20 of those diagnosed are younger than this. Those with young onset Parkinson’s are more likely to exhibit early dystonia and motor fluctuations and dyskinesias, caused by prolonged use of dopaminergic treatment. | ||
=== Get to know more about interventions for people with Parkinson’s using complimentary technology === | === Get to know more about interventions for people with Parkinson’s using complimentary technology === | ||
#Example of a man using visual cues to improve his walking | |||
{{#ev:youtube|idjOuw35-7uPw|300}} | |||
#The phenomena of using blue tints for dyskinesia | |||
{{#ev:youtube|OrcO2oRv75I|300}} | |||
#Using GaitAid | |||
{{#ev:youtube|id6XoHBqw8GnI|300}} | |||
<br><br> | <br><br> | ||
<br><br> | <br><br> | ||
Revision as of 00:21, 19 February 2014
A person with Parkinson’s may be experiencing several symptoms at the same time; your history taking and physical assessment should elicit the main issue(s) to prioritise as part of the management strategy. Whilst physiotherapy concentrates on the physical manifestations of a disorder, don’t forget to pay attention to how their other symptoms impact on the person’s lifestyle.
Remember also that optimal outcome is achieved through the collaboration with others from a team of health and social care professionals with expertise in other domains of Parkinson’s, from volunteers, family and friends.
Aims of Physiotherapy[edit | edit source]
- Maintain and improve levels of function and independence, which will help to improve a person’s quality of life
- Use exercise and movement strategies to improve mobility
- Correct and improve abnormal movement patterns and posture, where possible
- Maximise muscle strength and joint flexibility
- Correct and improve posture and balance, and minimise risks of falls
- Maintain a good breathing pattern and effective cough
- Educate the person with Parkinson’s and their carer or family members
- Enhance the effects of drug therapy
Physiotherapy Intervention[edit | edit source]
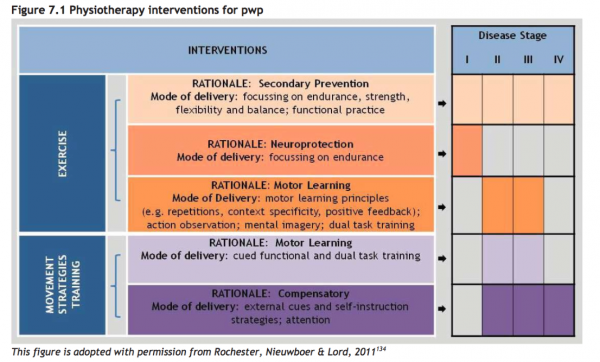
The Review version of the European Physiotherapy Guideline divides physiotherapy intervention for Parkinson’s into exercise and movement strategy training.
Exercise[edit | edit source]
Increasingly being proven to maintain health and well-being in more than just Parkinson’s – exercise can address secondary prevention (focusing on strength, endurance, flexibility, functional practice and balance); exercise for neuroprotection focuses on endurance; and exercise using motor learning principles uses approaches, such as mental imagery and dual task training.
Exercise undertaken in a group setting has the added value of providing a social connection to those becoming increasingly isolated as the condition progresses, or for those who are newly diagnosed, so they can see the benefits of maintaining exercise and activity. A group environment also permits time for people to ask questions and discuss their symptoms and own management strategies with one another.
Movement Strategy Training[edit | edit source]
Basal ganglia disorders cause deficits in the generation of internal (automatic) behaviour.
Strategies (physical or attentional cues and combined strategies) can help overcome some of the resultant problems, hence have become an increasingly utilised method of intervention for people with Parkinson’s.
We can see immediately the effects of external cueing and attention on improving step length, freezing and turning during walking tasks, and in activities of daily living.
Depending on the cognitive state of the individual, they may be able to learn how to self-instruct in the use of an internal cue or strategy. If less able, the cue or strategy has to come from an external source e.g. a visual strip on the ground, the rhythmic beat of a metronome.
Depending on the stage of the condition, the rationale for intervention choices will differ:
This figure has been copied with permission of Lynn Rochester on behalf of Rochester, Nieuwboer and Lord (2011).
As mentioned in the subsection on Physiotherapy for Parkinson’s: Referral and assessment, during the earlier stages of diagnosis, greater emphasis is placed on education and self-management. The individual should be encouraged to continue being active and participate in physical exercise for as long as possible. Significant respiratory complications develop in many people as their Parkinson’s progresses, so attention should be paid to monitor and manage encroaching weakness of respiratory muscles and rigidity of the thoracic cage.
The European Guideline provides a section that describes the use of motor learning (pages 52 – 55), expectations if practiced and executed as a strategy to train improvements in movement. It takes the form of cued functional and dual task training, compensatory strategy training uses external cues, self-instruction and attention. Examples include:
- Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing
- Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk
- Attention – Thinking about taking a big step; making a wider arc turn
- Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backwards as a cue ready to then walk forwards
Most people who are diagnosed with Parkinson’s are aged 50 or over, but 1 in 20 of those diagnosed are younger than this. Those with young onset Parkinson’s are more likely to exhibit early dystonia and motor fluctuations and dyskinesias, caused by prolonged use of dopaminergic treatment.
Get to know more about interventions for people with Parkinson’s using complimentary technology[edit | edit source]
- Example of a man using visual cues to improve his walking
- The phenomena of using blue tints for dyskinesia
- Using GaitAid