Parkinson's - Clinical Presentation
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Basal Ganglia Function[edit | edit source]
Pre-movement planning and preparation
Initiation of movement
Sequencing and timing of movement
Maintaining cortically selected movement amplitude i.e. the frontal cortex is involved in the choice of movement, after which the basal ganglia take over and communicate with the other areas of the brain. The scale of a required movement is then calibrated the through sensorimotor integration. For example, a person may start to walk with normal step length, but if amplitude is incorrectly executed, their steps soon become shorten, progressing to a shuffling gait.
Basal Ganglia Dysfunction[edit | edit source]
Basal ganglia dysfunction affects the automatic nature of our movements. This includes:
Impaired performance of well-learnt motor skills and movement sequences
Problems maintaining sufficient movement amplitude
Difficulty in performing more than one task simultaneously (dual-tasking)
Difficulty in shifting motor and cognitive sets
Slower mental processing
Perseveration (repetition) in thought and action
For a person to perform activities of daily living, the basal ganglia need to be working properly. Impairment affects both mental and physical agility as described by motor and non-motor symptoms.
Clinical Presentation[edit | edit source]
The main motor (movement) symptoms of Parkinson’s are:
- Tremor (involuntary shaking of parts of the body) www.epda.eu.com/en/parkinsons/in-depth/pdsymptoms/tremor/tremor-parkinsons/
- Rigidity (experienced as muscle stiffness) www.epda.eu.com/en/parkinsons/in-depth/pdsymptoms/rigidity/rigidity-and-parkinsons/
- Bradykinesia (experienced as slow movement) www.epda.eu.com/en/parkinsons/in-depth/pdsymptoms/bradykinesia/bradykinesia-and-parkinsons/
Progression of Parkinsons[edit | edit source]
Hoehn and Yahr Scale [edit | edit source]
The Hoehn and Yahr scale is commonly used to describe how the motor symptoms of Parkinson’s progress.
The original scale was published in a 1967 article by Melvin Yahr and Margaret Hoehn, and included stages 1 to 5.
Since then, a modified Hoehn and Yahr scale has been proposed with the addition of stages 1.5 and 2.5 to help describe the intermediate course of the disease.
As noted in the H&Y scale, at diagnosis, these signs are usually unilateral, but they become bilateral as the condition progresses. Later in the course of the Parkinson’s additional signs may be present including postural instability (e.g. tendency to fall backwards after a sharp pull from the examiner - the ‘pull test’) and orthostatic hypotension (OH).
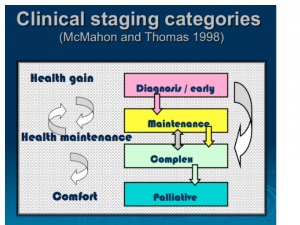
MacMahon and Thomas Scale[edit | edit source]
MacMahon and Thomas (1998) have provided a clinical staging classification. The model is based on four stages of progression from a state of gaining best health, through to the requirement of support and comfort - diagnosis, maintenance, complex and palliative.
Unlike the H&Y scale, there is more fluidity with this model, allowing for periods when the person might deteriorate during an illness, whether related to Parkinson’s or not e.g. chest infection, rehabilitation, post fall and fracture, but regains prior ability on recovery.
Non-motor Symptoms[edit | edit source]
Non-dopaminergic and non-motor symptoms often present before diagnosis of Parkinson’s, and almost inevitably emerge as the condition progresses. They often dominate the clinical picture of advanced Parkinson's, contributing to disability, impaired quality of life, and shortened life expectancy.
Non-motor symptoms are often inadequately treated despite increased attention on the recognition and quantitation of symptoms. Commonly experienced non-motor symptoms include:
- depression
- constipation
- pain
- genitourinary problems
- sleep disorders.
As these can be improved with available treatments, it is important to elicit from the individual whether they have any such (or other) symptoms. The Non-motor symptom questionnaire [hyperlink to the Chaudhuri Non-motor symptoms questionnaire
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.