Pancoast Tumor: Difference between revisions
No edit summary |
No edit summary |
||
| Line 142: | Line 142: | ||
Complete resection of these tumors is a necessity for long term survival and this is made complicated due to their complexity and involvement of the structures around them that include the brachial plexus, subclavian vessels and the spine. Because of this, a multimodal approach is often needed to ensure removal while minimizing any further complications or recurrences [13]. | Complete resection of these tumors is a necessity for long term survival and this is made complicated due to their complexity and involvement of the structures around them that include the brachial plexus, subclavian vessels and the spine. Because of this, a multimodal approach is often needed to ensure removal while minimizing any further complications or recurrences [13]. | ||
Initially pancoast tumors were viewed as inoperable and incurable and treatment for them was radiotherapy with a palliative intent. It wasn’t until 1956 when resection with radiotherapy was attempted by Chardack and MacCallum which consisted of an upper lobe lobectomy with en-bloc chest wall and nerve root resection followed by adjuvant chemotherapy. This patient lived for 5 years without recurrence and further trials of induction radiotherapy and en-bloc resection conducted by Shaw & Paulson in 1961, confirmed a 5 year survival rate of 30% with complete resection in about 60% of patients.[13,10] Preoperative radiation followed by surgery became the standard of care [9] for the next 30 years until more and more complications were starting to be seen and other surgical techniques began developing in the late 80s and early 90s to addressed tumors invading the spine and the subclavian vessels. The first was the anterior (Anterior transclavicular approach) approach developed by Dartevelle which was later modified by Grunenwald who developed an anterior clavicular sparring approach (hemi-clamshell incision with supraclavicular extension). Its purpose was to optimize exposure by providing direct visualization of vascular structures, brachial plexus, sympathetic chain and stellate ganglion [15]. This became very popular yet 5 year survival rates still remained around 30% and local recurrence was observed in 40% of all operated patients. The posterior approach was later developed by Shaw-Paulson to target tumors situated in the posterior superior sulcus that did not invade the anterior structures of the thoracic inlet but may invade the vertebral bodies or the brachial plexus (C8 and T1 nerve roots are most common).[15,13]<br> The multimodal treatment approach (chemoradiation followed by surgical resection) became the standard during this time and resulted in much improved outcomes as can be seen by the studies listed below [13]. However, due to poor performance status and advanced tumor stages, only 30-40% of patients are eligible for multimodal treatment. [18]<br> | Initially pancoast tumors were viewed as inoperable and incurable and treatment for them was radiotherapy with a palliative intent. It wasn’t until 1956 when resection with radiotherapy was attempted by Chardack and MacCallum which consisted of an upper lobe lobectomy with en-bloc chest wall and nerve root resection followed by adjuvant chemotherapy. This patient lived for 5 years without recurrence and further trials of induction radiotherapy and en-bloc resection conducted by Shaw & Paulson in 1961, confirmed a 5 year survival rate of 30% with complete resection in about 60% of patients.[13,10] Preoperative radiation followed by surgery became the standard of care [9] for the next 30 years until more and more complications were starting to be seen and other surgical techniques began developing in the late 80s and early 90s to addressed tumors invading the spine and the subclavian vessels. The first was the anterior (Anterior transclavicular approach) approach developed by Dartevelle which was later modified by Grunenwald who developed an anterior clavicular sparring approach (hemi-clamshell incision with supraclavicular extension). Its purpose was to optimize exposure by providing direct visualization of vascular structures, brachial plexus, sympathetic chain and stellate ganglion [15]. This became very popular yet 5 year survival rates still remained around 30% and local recurrence was observed in 40% of all operated patients. The posterior approach was later developed by Shaw-Paulson to target tumors situated in the posterior superior sulcus that did not invade the anterior structures of the thoracic inlet but may invade the vertebral bodies or the brachial plexus (C8 and T1 nerve roots are most common).[15,13]<br> The multimodal treatment approach (chemoradiation followed by surgical resection) became the standard during this time and resulted in much improved outcomes as can be seen by the studies listed below [13]. However, due to poor performance status and advanced tumor stages, only 30-40% of patients are eligible for multimodal treatment. [18]<br> | ||
<br> | <br> | ||
Other surgical approaches include…<br> | Other surgical approaches include…<br> | ||
<br> | |||
'''Surgical limitations:''' Neural, vascular, vertebral body and lymph node invasion <br> | |||
Contraindications to surgery: presence of extra-thoracic sites of metastasis, histologically confirmed N2 disease, extensive invasion of the cervical trachea, esophagus and the brachial plexus above the C7 nerve root (indicates that the tumor is locally too extensive to achieve a complete resection or that limb amputation is necessary), massive vertebral invasion that’s diagnosed preoperatively. [17] | |||
'''Surgical complications: '''Spinal fluid leakage, Horner’s syndrome and nerve deficits, Hemothorax, Chylothorax & Prolonged ventilator support [17] | |||
<br> The current treatment of choice is complete removal of the tumor by en bloc chest wall resection combined with lobectomy and node staging and it may include resection of the paravertebral sympathetic chain, stellate ganglion, lower trunks of the brachial plexus, subclavian artery, or portions of the thoracic vertebrae depending on its involvement. Radiation and chemotherapy can address individual adverse findings and for local and systemic control and induction chemoradiotherapy is used with potentially resectable tumors and surgery is undertaken 2-4 weeks after radiation therapy. A combined thoracic-nonsurgical approach is used for tumors invading the brachial plexus and/or the spine. [9]<br> | |||
<br> The current treatment of choice is complete removal of the tumor by en bloc chest wall resection combined with lobectomy and node staging and it may include resection of the paravertebral sympathetic chain, stellate ganglion, lower trunks of the brachial plexus, subclavian artery, or portions of the thoracic vertebrae depending on its involvement. Radiation and chemotherapy can address individual adverse findings and for local and systemic control and induction chemoradiotherapy is used with potentially resectable tumors and surgery is undertaken 2-4 weeks after radiation therapy. A combined thoracic-nonsurgical approach is used for tumors invading the brachial plexus and/or the spine. [9]<br> | |||
'''Brachial Plexus block:''' Used in combination with local anesthetics and steroids as an adjunct to drug treatment for rapid relief of pain or to control breakthrough pain [8]. A study don’t by Peláez and colleagues purpose that in aggressive tumors compressing the brachial plexus that do not respond to conventional treatment or regional anaesthesia, utilizing the addition of a paravertebral nerve block to the plexus could substantially reduce the patients pain without impacting longevity [20]. This is also supported in a study by Vranken and colleagues who purposed a reversible, non destructive, continuous nerve blocking technique involving administration of local antsthetics through an axillary cathter into the brachial plexus. This resulted in a significant decrease in the patients visual analog pain score and an increase in performance skills and QOL without any side effects in 4 patients [22]. | '''Brachial Plexus block:''' Used in combination with local anesthetics and steroids as an adjunct to drug treatment for rapid relief of pain or to control breakthrough pain [8]. A study don’t by Peláez and colleagues purpose that in aggressive tumors compressing the brachial plexus that do not respond to conventional treatment or regional anaesthesia, utilizing the addition of a paravertebral nerve block to the plexus could substantially reduce the patients pain without impacting longevity [20]. This is also supported in a study by Vranken and colleagues who purposed a reversible, non destructive, continuous nerve blocking technique involving administration of local antsthetics through an axillary cathter into the brachial plexus. This resulted in a significant decrease in the patients visual analog pain score and an increase in performance skills and QOL without any side effects in 4 patients [22]. | ||
<br>'''Radiofrequency Destruction of the Brachial Plexus:''' Last resort treatment involving destruction of the brachial plexus via a radiofrequency lesion under biplanar fluoroscopic guidance. [8] | <br>'''Radiofrequency Destruction of the Brachial Plexus:''' Last resort treatment involving destruction of the brachial plexus via a radiofrequency lesion under biplanar fluoroscopic guidance. [8] | ||
<br>'''Dorsal Root Entry Zone Lesioning (DREZ):''' Major neurosurgical procedure used as a last resort when all other branchial plexopathy treatments have failed [8]<br> | <br>'''Dorsal Root Entry Zone Lesioning (DREZ):''' Major neurosurgical procedure used as a last resort when all other branchial plexopathy treatments have failed [8]<br> | ||
<br> | <br> | ||
''' '''<u>'''Pharmacological management:'''</u> | ''' '''<u>'''Pharmacological management:'''</u> | ||
Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications [9]<br> | Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications [9]<br> | ||
Revision as of 07:33, 3 April 2012
Original Editors - Paul Clark & Sam Holzknecht from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
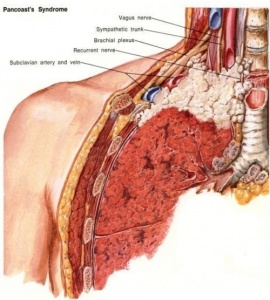
Pancoast tumor is an uncommon lung cancer that arises at the level of the superior sulcus and is limited to the apical segment of either lung. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleThis is a form of non-small-cell carcinomas (NSCLCs) that are very difficult to treat because of their proximity and frequent metastasis to adjactent structures such as the subclavian vessels, lymphatic system, brachial plexus, spine, second and third ribs, stellate ganglion, and the sympathetic nervous system. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleNSCLCs generally grow and spread slower and are divided into three different forms of cancer: squamous cell carcinomas (45-50%), adenocarcinomas (36-38%), or undifferentiated large-cell carcinomas (11-13%). Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleRather than invading underlying lung tissue, this tumor presents as a abnormal patch of tissue over the lung apex and initially involves the chest wall strucutures. This can be treated if caught early on before it spreads and moves to the lymph nodes. Pancoast tumors are often mis-diagnosed and/or diagnosed too late.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Tumor located at the apex of the lungs.
Pancoast tumors may occur in the three compartments of the thoracic inlet and symptoms are related to the location.
File:Pancoast tumor Anterior.png File:Pancoast tumor middle.png
File:Pancoast tumor posterior.png
Prevalence[edit | edit source]
"Lung cancers are the leading cause of death in both men and women in North American."Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In 2011, there was an estimated new diagnosis of 221,130 new cases of lung cancer with 156,940 deaths relating to lung cancer. Lung cancer accounts for more deaths when compared to prostate/breast, colon, and pancreatic cancer combined.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Of the number of new lung cancer diagnosis, approximately 5% can be attributed to pancoast tumors.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The highest occurence is found in men between the ages of 40 and 60 with a history of smoking.
Characteristics/Clinical Presentation[edit | edit source]
Pancoast tumors are very difficult to diagnosis early on. This is based on their low prevalence rate and many differential diagnosis'. "Typical" symptoms of lung cancer such as cough, dyspnea, and haemoptysis are less frequent.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Common presentations include:
referred pain over the scapula to the shoulderCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
pain is relieved by propping up arm on table or holding with other arm
radiating pain to the ulnar side of the arm and hand (55-60%)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Horner's syndrome (30%)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
atrophy of the arm, forearm, and handCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
parasthesias of the handCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
between the ages of 40-60Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
men > femaleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Associated Co-morbidities[edit | edit source]
muscle atrophy
cervical radiculopathy
Horner's Syndrome
COPD
vertebrae compression
bone cancer
Medications[edit | edit source]
Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications [2]
Opioid Analgesics: Primary treatment of pain that can be combined with NSAIDs and may be a short-acting potent opioid such as oxycodone or an immediate-release morphine or methadone [1].
Antineoplastic agents: Inhibit cell growth and proliferation and are used in a variety of different cancers including head, neck, breast, testicular and ovarian cancer [2].
Cisplatin (Platinol): Alkylating agent causing intrastrand and interstrand cross-linking of DNA that leads to strand breakage. It has a broad range of antitumor activity and forms backbone of currently available approved combination chemotherapy regimens that cause Pancoast syndrome. Its administered via IV in isotonic sodium chloride solution (0.9%) or sodium chloride and glucose. Adequate hydration must be maintained up to 24 hours after a dose and Renal, hematological, auditory, and neurological function must be monitored [2].
Etoposide (Toposar, VePesid): Semisynthetic derivative of podophyllotoxin with antineoplastic properties interferes with topoisomerase II function thus inhibiting DNA synthesis [2].
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Diagnosis is often difficult and delayed due to the typical absence of lung cancer symptoms and includes a combination of CT scans and MRI followed by a biopsy confirmation [12].
Chest x-ray: Difficult early detection due to limited visualization of the top of the lung but may reveal asymmetries like a small, uniform patch of tissue or pleural thickening on the apex of one lung, invasion of the ribs or vertebrae and enlargement of the mediastinum [11] (Apical lordotic films may be more revealing) [9].
MRI: Most accurate at displaying the extent of the involvement and invasion of nearby structures including the brachial plexus, subclavian vessels, spine, and neural foramina. Contrast can be used to better display the local extent of the damage [10,11].
CT scan: Displays involvement of the brachial plexus, chest wall, mediastinum, liver, adrenal glands, pulmonary nodules, vertebra, vena cava, trachea, and esophagus and contrast can be utilized to see involvement of blood vessels under the clavicle. CT scan is less expensive, more available and more effective than the MRI at assessing the mediastinum to determine if the tumor has involved the lymph nodes [10,11]. This is essential in detecting N2 mediastinal lymphadenopathy which has a significant adverse effect on survival but only present in 20% of cases [9,13].
(MRI and CT scan of the brain is often performed at the initial evaluation to check for distant metastases to the brain)
Arteriogram or a venogram: Look at the involvement of the subclavian artery/vein under the clavicle [11]
Bronchoscopy: Involvement of the tracheal and bronchial cavities and used in excluding unsuspected concurrent endobronchial lesions [11,12]
Biopsy: 90% of patients can be correctly diagnosed based on clinical and radiological findings alone but 95% can be diagnosed through percutaneous, supraclavicular fine-needle aspiration biopsy that’s fluoroscopy or CT guided [11,9]. Transthoracic needle biopsy with CT guidance has a high yield of 95% and some tumors maybe only evaluated by open or video assisted thoracotomy.
Mediastinoscopy: Samples of lymph nodes are taken at the lowest part of the neck behind the breastbone to determine if the tumor has spread into the mediastinum.
Sputum cytology: results are positive in fewer than 15% of patients [9].
PET scans: Help identify involved lymph nodes and the distant spread of cancer [11] and is used in staging non–small cell lung cancer [12].
Liver and bone scans: determine if the cancer has spread [11].
Staging: Based on scalene node biopsy results of palpable lymph nodes or mediastinoscopy findings [11]. American Joint Committee on Cancer (AJCC) and the Union Internationale Contre le Cancer (UICC) have adopted the International System for Staging Lung Cancer that’s based on characteristics and distribution of the tumor… [9]
• T describes the size and invasiveness of the primary tumor
o T3 = tumor of any size that invades the chest wall (parietal pleura).
o T4 = tumor of any size that invades the vertebral body, neural or vascular structure, mediastinum, esophagus, or trachea.
• N describes the distribution of positive lymph nodes:
o N1 = metastasis to ipsilateral peribronchial or hilar nodes
o N2 = spread to ipsilateral mediastinal and/or subcarinal nodes
o N3 = metastasis to nodes of the contralateral hilar and mediastinal areas or scalene or supraclavicular nodes, either ipsilateral or contralateral.
• M describes the extent of distant metastasis:
o M0 = no identifiable metastatic disease
o M1 = (Stage IV) designates the presence of distant metastasis (brain, bone, liver)
The amount of nerve-root involvement and careful neurological investigation of the arm and shoulder function is also important and very informative [10].
Etiology/Causes[edit | edit source]
Common risk factors include (similar to lung cancer):
smoking
secondhand smoke
asbestos exposure
exposure to industrial elements like gold or nickel
diesel exhaust
Systemic Involvement[edit | edit source]
Pancoast tumors are often mis-diagnosed or diagnosed too late to prevent metastasis to adjoining structures. This form of lung cancer is very dangerous because of its close proximity to other structures that include:
brachial plexus- this is commonly invaded at the ulnar distribution (C8-T1), thus atrohpy/parasthesia of the ulnar distribution is reported. This is often the patient's primary complaint/presentation to therapy with shoulder pain that radiates down to the 4th and 5th digit.
subclavian vessels- metastasis to the subclavian artery or adjoining structure may lead to deterioration or compression of blood vessels.
stellate ganglion- This is a large ganglion located at the bottom of the cervical spine in connetion with the thoracic spine and is related to the sympathetic nervous system. Invasion of this may result in Horner's Syndrome.
adjacent vertebral bodies- If the tumor is able to metastasize the vertebral bodies, this may lead to permanent paralysis of the affected area.
Medical Management (current best evidence)[edit | edit source]
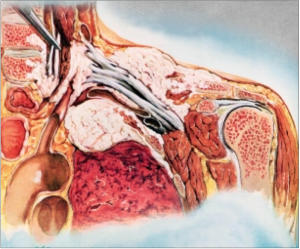
Complete resection of these tumors is a necessity for long term survival and this is made complicated due to their complexity and involvement of the structures around them that include the brachial plexus, subclavian vessels and the spine. Because of this, a multimodal approach is often needed to ensure removal while minimizing any further complications or recurrences [13].
Initially pancoast tumors were viewed as inoperable and incurable and treatment for them was radiotherapy with a palliative intent. It wasn’t until 1956 when resection with radiotherapy was attempted by Chardack and MacCallum which consisted of an upper lobe lobectomy with en-bloc chest wall and nerve root resection followed by adjuvant chemotherapy. This patient lived for 5 years without recurrence and further trials of induction radiotherapy and en-bloc resection conducted by Shaw & Paulson in 1961, confirmed a 5 year survival rate of 30% with complete resection in about 60% of patients.[13,10] Preoperative radiation followed by surgery became the standard of care [9] for the next 30 years until more and more complications were starting to be seen and other surgical techniques began developing in the late 80s and early 90s to addressed tumors invading the spine and the subclavian vessels. The first was the anterior (Anterior transclavicular approach) approach developed by Dartevelle which was later modified by Grunenwald who developed an anterior clavicular sparring approach (hemi-clamshell incision with supraclavicular extension). Its purpose was to optimize exposure by providing direct visualization of vascular structures, brachial plexus, sympathetic chain and stellate ganglion [15]. This became very popular yet 5 year survival rates still remained around 30% and local recurrence was observed in 40% of all operated patients. The posterior approach was later developed by Shaw-Paulson to target tumors situated in the posterior superior sulcus that did not invade the anterior structures of the thoracic inlet but may invade the vertebral bodies or the brachial plexus (C8 and T1 nerve roots are most common).[15,13]
The multimodal treatment approach (chemoradiation followed by surgical resection) became the standard during this time and resulted in much improved outcomes as can be seen by the studies listed below [13]. However, due to poor performance status and advanced tumor stages, only 30-40% of patients are eligible for multimodal treatment. [18]
Other surgical approaches include…
Surgical limitations: Neural, vascular, vertebral body and lymph node invasion
Contraindications to surgery: presence of extra-thoracic sites of metastasis, histologically confirmed N2 disease, extensive invasion of the cervical trachea, esophagus and the brachial plexus above the C7 nerve root (indicates that the tumor is locally too extensive to achieve a complete resection or that limb amputation is necessary), massive vertebral invasion that’s diagnosed preoperatively. [17]
Surgical complications: Spinal fluid leakage, Horner’s syndrome and nerve deficits, Hemothorax, Chylothorax & Prolonged ventilator support [17]
The current treatment of choice is complete removal of the tumor by en bloc chest wall resection combined with lobectomy and node staging and it may include resection of the paravertebral sympathetic chain, stellate ganglion, lower trunks of the brachial plexus, subclavian artery, or portions of the thoracic vertebrae depending on its involvement. Radiation and chemotherapy can address individual adverse findings and for local and systemic control and induction chemoradiotherapy is used with potentially resectable tumors and surgery is undertaken 2-4 weeks after radiation therapy. A combined thoracic-nonsurgical approach is used for tumors invading the brachial plexus and/or the spine. [9]
Brachial Plexus block: Used in combination with local anesthetics and steroids as an adjunct to drug treatment for rapid relief of pain or to control breakthrough pain [8]. A study don’t by Peláez and colleagues purpose that in aggressive tumors compressing the brachial plexus that do not respond to conventional treatment or regional anaesthesia, utilizing the addition of a paravertebral nerve block to the plexus could substantially reduce the patients pain without impacting longevity [20]. This is also supported in a study by Vranken and colleagues who purposed a reversible, non destructive, continuous nerve blocking technique involving administration of local antsthetics through an axillary cathter into the brachial plexus. This resulted in a significant decrease in the patients visual analog pain score and an increase in performance skills and QOL without any side effects in 4 patients [22].
Radiofrequency Destruction of the Brachial Plexus: Last resort treatment involving destruction of the brachial plexus via a radiofrequency lesion under biplanar fluoroscopic guidance. [8]
Dorsal Root Entry Zone Lesioning (DREZ): Major neurosurgical procedure used as a last resort when all other branchial plexopathy treatments have failed [8]
Pharmacological management:
Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications [9]
Opioid Analgesics: Primary treatment of pain that can be combined with NSAIDs and may be a short-acting potent opioid such as oxycodone or an immediate-release morphine or methadone [8].
Antineoplastic agents: Inhibit cell growth and proliferation and are used in a variety of different cancers including head, neck, breast, testicular and ovarian cancer [9].
Cisplatin (Platinol): Alkylating agent causing intrastrand and interstrand cross-linking of DNA that leads to strand breakage. It has a broad range of antitumor activity and forms backbone of currently available approved combination chemotherapy regimens that cause Pancoast syndrome. Its administered via IV in isotonic sodium chloride solution (0.9%) or sodium chloride and glucose. Adequate hydration must be maintained up to 24 hours after a dose and Renal, hematological, auditory, and neurological function must be monitored [9].
Etoposide (Toposar, VePesid): Semisynthetic derivative of podophyllotoxin with antineoplastic properties interferes with topoisomerase II function thus inhibiting DNA synthesis [9].
Physical Therapy Management (current best evidence)[edit | edit source]
When it comes to pancoast tumors, the primary role of the Physical Therapist is post operative treatment to prevent respiratory complications including atelectasis and pneumonia, and control the patient’s pain levels. The patient is immobilized the first post op day with attention to chest Physiotherapy and bronchoscopic suctioning may be necessary to clear secretions in patients with ineffective cough [30]. Intensive respiratory care should be implemented and chest expansion measurements should be taken to ensure... [16]
o Adequate ventilation using mechanical support (if necessary)
o Satisfactory chest tube function
o Clearance of secretions by mobilizing, coughing, chest physiotherapy, nasotracheal or orotracheal or bronchoscopic suctioning, or a temporary tracheostomy
o Adequate analgesia
o Increased transpulmonary pressure with incentive spirometry or continuous positive airway pressure mask.
Avoid fluid overload and use diuretics judiciously to avoid acute respiratory distress. Chest tubes remain in place until all air leaks have stopped, there is complete lung expansion and almost no fluid drainage present [16].
Other roles of the PT are to maintain function and ADLs and search for and treat shoulder issues that include subluxation and adhesive capsulitis [8]. Laser therapy in combination with and individualized wellness program is also effective in treating this condition and can improve the patients overall health and wellbeing. [8]
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
Lung Cancer; Non-Small Cell or Oat Cell (Small Cell) [9]
Thoracic Outlet syndrome
Pulmonary echinococcosis [25]
Pulmonary leiomyosarcoma [26]
C8-T1 radiculopathy [27]
Primary Ewing's sarcoma [29]
Case Reports/ Case Studies[edit | edit source]
Paravertebral Cervical Nerve Block in a Patient Suffering from a Pancoast Tumor
Pancoast Tumour: a case report
Nasal tip metastasis revealing a pancoast tumour
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NGmwZeh8JwVIzrKgHG1LrDm0izTr7ViJiDkSYAY2BW5hiXsx0|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
1) Kruger F, Joubert J, Bolliger C. Severe pancoast tumour. Respiration; International Review Of Thoracic Diseases. 2000;67(3):315.
2) Vieira M, Correia, Resende, Azevedo, Mesquita-Guimarães. Nasal tip metastasis revealing a Pancoast tumour. British journal Of dermatology. 1998 March;138(3):559-560.
3) Peláez R, Pascual G, Aguilar J, Atanassoff P. Paravertebral cervical nerve block in a patient suffering from a pancoast tumor. Pain Medicine . 2010 December; 11(12):1799-1802.
4) Rusch VW. Management of pancoast tumours. The lancet oncology. 2006; 7:997-1005.
5) Medical State of Mind [homepage on the internet]. Medical State of Mind [updated 2011 April 6; cited 2012 April 1]. Available from: http://medicalstate.tumblr.com/post/4402556070/pancoasts-syndrome-a-pancoast-tumor-is-a-tumor
6) Barbetakis N. Pancoast tumor: surgical approaches and techniques. Topics in thoracic surgery. 2012; 273-84.
7) Kaufman A, Amar D, Rusch VW. Pancoast tumors and combined spinal resections. In: Slinger PD, editor. Principles and practice of anesthesia for thoracic surgery. New York: Springer Science + Business Media; 2011. p. 405-13.
8) Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm
9) D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication
10) Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.
11) Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview
12) Lynne Eldridge Md. What Is a Pancoast Tumor? [homepage on the Internet]. March 4th, 2012 [cited 2012 Mar 30]. Available from: http://lungcancer.about.com/od/typesoflungcancer/f/pancoasttumor.htm
13) Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.
14) Kwong KF, Edelman, MJ, Suntharalingam, M. High-dose radiotherapy in trimodality treatment of Pancoast tumors results in high pathologic complete response rates and excellent long-term survival, J Thorac Cardiovasc Surg Dec 17, 2004; 129:250-257.
15) Barbetakis N,, Pancoast Tumors: Surgical Approaches and Techniques. Topics in Thoracic Surgery 2012; :273-284.
16) Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.
17) Pitz CM, De La Rivière AB, Van Swieten HA. Surgical treatment of Pancoast tumours. European Journal of Cardio-Thoracic Surgery July 2004; 26(1):202-208.
18) Parissis H, Young V. Treatment of pancoast tumors from the surgeons prospective: re-appraisal of the anteriormanubrial sternal approach. Journal of Cardiothoracic Surgery 5/1/2010; 102(5).
19) Gofeld M, Bhatia A. Alleviation of Pancoast's Tumor Pain by Ultrasound-Guided Percutaneous Ablation of Cervical Nerve Roots. Pain Practice [serial online]. July 2008;8(4):314-319.
20) Peláez R, Pascual G, Aguilar J, Atanassoff P. Paravertebral Cervical Nerve Block in a Patient Suffering from a Pancoast Tumor. Pain Medicine [serial online]. December 2010;11(12):1799-1802.
21) Davis G, Knight S. Pancoast tumor resection with preservation of brachial plexus and hand function. Neurosurgical Focus [serial online]. June 15, 2007;22(6):E15.
22) Vranken J, Zuurmond W, de Lange J. Continuous brachial plexus block as treatment for the Pancoast syndrome. The Clinical Journal Of Pain [serial online]. December 2000;16(4):327-333.
23) Yukiue H, Tanahashi M, Haneda H, Suzuki E, Yoshii N, Niwa H. [Surgical treatment for Pancoast tumors--significance of surgical approach and induction chemoradiotherapy]. Kyobu Geka. The Japanese Journal Of Thoracic Surgery [serial online]. January 2010;63(1):4-8.
24) Narayan S, Thomas C. Multimodality therapy for Pancoast tumor. Nature Clinical Practice Oncology [serial online]. September 2006;3(9):484-491.
25) Karamustafaoglu Y, Yoruk Y, Mamedov R, Yavasman I. Pulmonary echinococcosis mimicking Pancoast tumor. The Journal Of Thoracic And Cardiovascular Surgery [serial online]. April 2010;139(4):e57-e58.
26) Shoji F, Yoshino I, Takeshita M, Sumiyoshi S, Sueishi K, Maehara Y. Pulmonary leiomyosarcoma presenting as a pancoast tumor. Pathology - Research & Practice [serial online]. October 18, 2007;203(10):745-748.
27) Abdul Khader S, Kumar A. Pancoast tumor presenting as shoulder pain and C8-T1 radiculopathy: a case report. (Poster Session). Archives Of Physical Medicine & Rehabilitation [serial online]. November 2002;83(11):1663.
28) Weiner S, Gardiner L. Pancoast tumor mimicking musculoskeletal pain: a case study. JNMS: Journal Of The Neuromusculoskeletal System [serial online]. March 2001;9(1):16-20.
29) Lowie V. Primary Ewing's sarcoma presenting as a Pancoast tumour. Thorax [serial online]. January 2011;66(1):89-90.
30) Slinger PD, & Principles and Practice of Anesthesia for Thoracic Surgery. New York: Springer Science+Business media LLC; 2011.