Paget's Disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 64: | Line 64: | ||
Bone scans can help document the extent of disease and should be used to follow treatment. In addition, a bone scan can pick up early changes in bone even before the patient develops symptoms. {{#ev:youtube|dC2TrqcEJEA}} | Bone scans can help document the extent of disease and should be used to follow treatment. In addition, a bone scan can pick up early changes in bone even before the patient develops symptoms. {{#ev:youtube|dC2TrqcEJEA}} | ||
== Management == | == Management == | ||
Revision as of 03:10, 13 May 2022
Original Editors - Kevin Schoenfeld from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kevin Schoenfeld, Admin, Lucinda hampton, Priya Gulla, Nikhil Benhur Abburi, Elaine Lonnemann, Dave Pariser, Kim Jackson, WikiSysop, Uchechukwu Chukwuemeka, Claire Knott, Aminat Abolade, Rachael Lowe, Wendy Walker and Mariam Hashem
Introduction[edit | edit source]
Also known as Osteitis Deformans, Paget's disease of the bone is a metabolic bone disease caused by increased bone resorption followed by excessive unrestricted bone formation, due to activated osteoclasts. The normal bone marrow is replaced by increased and unorganized collagen and fibrous tissue, which lacks the structural stability of normal bone. This increased bone mass formation leads to complications such as fractures, arthritis, deformities, pain, and to a patient's weakened condition. Paget's disease is the second most common metabolic bone disease to osteoporosis [1][2][3]
Etiology[edit | edit source]
The exact cause of Paget's disease is unknown, though it is thought to be a slow, viral bone infection due to risk factors that include a gene-environment interaction. [1][2][4] The prevalence and causes of Paget's disease has been associated with genetic and geographical factors. A positive family history is reported in as many as 40% of patients with Paget's disease [1][2][4][5]. Paget's disease is mostly seen in an autosomal dominant distribution, and there have been three identifiable chromosomal regions associated with Paget's disease. [1] Geographically, populations in European, British, and Australian origin, and a migratory influence also play an important role especially in countries which of the early population migrated from Britain (United States, Australia, New Zealand, Canada).[1]
Epidemiology[edit | edit source]
Paget disease is usually seen in individuals older than 50 years. It is common in Caucasians of northern European descent. Paget disease is equally common in males and females. In the US, it affects 1-3 million people with most being asymptomatic. The disorder is slightly more common in white males. The disorder usually presents in the 4-5 decade of life but the diagnosis is often made a decade later[6].
Characteristics/Clinical Presentation[edit | edit source]
A patient with Paget's disease will often present as asymptomatic. However, the clinical presentation of a symptomatic patient varies greatly, due to the different levels of severity of this condition.
- Bone pain presents as constant, deep, and aching. Bones most commonly affected by Paget's disease include: Pelvis, Lumbar spine, Sacrum, Femur, Tibia, Skull, Shoulders, Thoracic spine, Cervical spine, and the ribs. [1]
- Increased focal temperature due to hyperaemia
- Joint pain including swelling and stiffness may present due to the damage of the cartilage lining the joints near the affected bones. [7]
- The most common symptom experienced with symptomatic Paget's disease is an aching pain worse at night that decreases with physical activity. [1][2]
- Muscular pain may present as referred pain from bony structures involved or as a complication due to the mechanical changes from the joint and bone defects. [1][2]
- Neurological pain due to a compressed nerve root or the spinal cord may cause symptoms such as a sharp pain, numbness, tingling, weakness, hearing loss, and double vision. [4]
- Patients with Paget's disease usually describe their pain as continuous. Different from osteoarthritis, pagetic bone pain usually increases with rest, on weight-bearing, when the limbs are warm, and at night[5]
- As many as 70% of people with Paget's disease present asymptomatic and is usually detected through radiographs and laboratory tests which are most times ordered for other indications[8][9]
Other clinical presentations may include [4]:
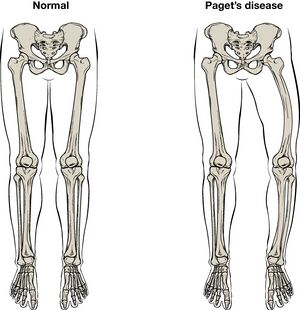
- Bone deformities such as bowlegs, and increased skull size
- Warmth over the affected bone or joint.
- Facial weakness or numbness.
- Loss of bowel or bladder control which may indicate spinal cord damage.
Associated Co-morbidities[edit | edit source]
- Paget's disease has an insidious onset and the disease progresses slowly. When Paget's disease is present in many bones the overactive osteoclasts have the ability to release enough calcium in the bloodstream to cause hypercalcemia, which can cause symptoms such as fatigue, weakness, loss of appetite, abdominal pain, and constipation. [2][1]
- Neurological complications due to nerve entrapment syndromes or nerve root compression as they exit the foramina which is narrowed by the increased bone mass of Paget's disease. [2]
- Hearing loss due to increased temporal bone mass and 8th spinal nerve compression. [2]
- Bone deformities such as increased skull size and bowing of limbs. [2]
- People with Paget's disease are also more susceptible to fractures because Pagetic bone is weaker than normal bone.[1][2]
- Cardiovascular problems may arise when 1/3 to 1/2 of the skeleton is involved, heart failure is possible due to an increased cardiac output (this is the most common cause of death in people with advanced Paget's disease).[1]
- Metabolic complications of Paget's disease may include renal stones, hyperparathyroidism, and hypercalcemia[8][9]
- A rare complication is sarcoma which is a bone cancer (also known as osteosarcoma or osteogenic sarcoma). This cancer may develop in Pagetic bone, which occurs in less than 1 percent of people with Paget's disease and usually doesn't develop until many years after the onset.[4]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Tests to assist in the diagnosis of Paget disease include:
- Bone scan
- Bone x-ray
- Elevated markers of bone breakdown like N-telopeptide
This disease also may also present with the following findings:
- Elevated ALP (alkaline phosphatase)
- Normal Serum calcium and Phosphate
Hyperuricemia is common and is due to a high turnover of bone.
Secondary hyperparathyroidism occurs in about 10% of patients due to inadequate calcium in the face of increased demand.
Plain x-rays may reveal arthritis or fractures of gross bony lesions.
Bone scans can help document the extent of disease and should be used to follow treatment. In addition, a bone scan can pick up early changes in bone even before the patient develops symptoms.
Management[edit | edit source]
Although there’s no cure for Paget’s disease of bone, there are treatments available to help people live well and manage the symptoms.
Medications
- Bisphosphonates are used to slow the progression of Paget’s disease. They help the body control the bone-building process to stimulate more normal bone growth.
- Pain relievers (analgesics) and non-steroidal anti-inflammatory drugs (NSAIDs) – are used to provide temporary pain relief.
- Calcium and vitamin D – are both important for bone health. You can get calcium through the diet and vitamin D through safe exposure to sunlight.
Surgery is only offered as an option to patients diagnosed with Paget disease when there is a progression into osteosarcoma. [6]
Physical Therapy Management[edit | edit source]
Encourage Client to Stay active – exercise helps to maintain bone health and joint mobility, as well as strengthen muscles. However as bones are weaker and more likely to fracture, certain forms of exercise are not suitable for people with Paget’s disease. eg avoid activities such as jogging, running, jumping, and aggressive forward bending and twisting exercises, if the spine is affected by Paget's disease [1]
Provide a tailored exercises plan, and also provide techniques and/or devices that can help to improve movement, reduce pain and make everyday activities easier. eg a walking stick to reduce the weight placed through affected bones, braces to correct position, foot orthotics to support and correct abnormal foot position or motion.
Educate on a healthy well-balanced diet – this can help client reach and maintain a healthy weight and reduce your risk of other health problems. Make sure they include calcium-rich foods.
Teach new ways to manage pain. eg heat packs can help ease muscle pain, cold packs can help with inflammation, gentle exercise can help relieve muscle tension, transcutaneous electrical nerve stimulation (TENS), and massage . Try different techniques until client finds the things that work best for them[10].
Encourage client to stay at work, it’s good for health and wellbeing. Discuss ways to help client get back to or stay at work[11]
A physical therapist can also assist a patient with Paget's disease in home modifications to make the patient safer with mobility around the home[10]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier;2009.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Josse RG, Hanley DA, Kendler D, Marie LG, Adachi JD, Brown J. Diagnosis and treatment of Paget’s disease of bone. Clinical and Investigative Medicine. 2007 Oct 1:E210-23.
- ↑ Seitz S, Priemel M, von Domarus C, Beil FT, Barvencik F, Amling M, Rueger JM. The second most common bone disease: a review on Paget’s disease of bone. European Journal of Trauma and Emergency Surgery. 2008 Dec 1;34(6):549-53.
- ↑ 4.0 4.1 4.2 4.3 4.4 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. 6th ed. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ 5.0 5.1 Schneider D, Hofmann MT,Peterson JA. Diagnosis and Treatment of Paget’s Disease of Bone. American Family Physician. 2002; 65(10):2069-72
- ↑ 6.0 6.1 Bouchette P, Boktor SW. Paget disease. InStatPearls [Internet] 2021 Jul 13. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK430805/(accessed 13.5.2022)
- ↑ Medical Foundation for Medical Education and Research. Mayo Clinic: Paget’s disease of bone.http://www.mayoclinic.com/health/pagets-disease-of-bone/DS00485. Updated August 15, 2008. Accessed March 3, 2010.
- ↑ 8.0 8.1 Seton M. Diagnosis, complications and treatment of Paget’s disease of bone. Aging Health. 2009 Aug;5(4):497-508.
- ↑ 9.0 9.1 Roux C, Dougados M. Treatment of patients with Paget’s disease of bone. Drugs. 1999 Nov 1;58(5):823-30.
- ↑ 10.0 10.1 Chow, David. Emedicine. Med Web:Paget Disease. http://emedicine.medscape.com/article/311688-overview. Updated December 18,2008. Accessed April 2, 2010.
- ↑ MSK Pagets Disease Available:https://msk.org.au/pagets-disease/ (accessed 13.5.2022)