Overview of Traumatic Brain Injury
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Definition[edit | edit source]
Traumatic Brain Injury [TBI}, also known as Head Injury and Acquired Brain Injury [ABI], is defined as injury to the brain which occurred as a result of trauma, and is non-progressive.
It occurs when an external force impacts the brain, & often is caused by a blow, bump, jolt or penetrating wound to the head. However, not all blows or jolts to the head cause TBI: some just cause bony damage to the skull but do not cause brain injury.
Causes of TBI[edit | edit source]
The 2 most common causes of TBI are:
- Falls
- Road Traffic Accident [RTA] This includes vehicle collisions, pedestrians being hit by a vehicle, vehicle-cyclist and car-motorcyclist collisions as well as bicycle and motorbike crashes which do not involve another vehicle.
Until recently, RTA was the primary cause of brain injury, but an international study published in 2013 reported that "falls have now surpassed road traffic incidents as the leading cause of this injury"[1].
Incidence of TBI[edit | edit source]
One study found that TBI was "a major cause of death and disability on the United States, contributing to about 30% of all injury deaths[2]".
A 2010 study looked at data from several nations, and reported that: "each year 235 000 Americans are hospitalized for non-fatal TBI, 1.1 million are treated in emergency departments, and 50 000 die. The northern Finland birth cohort found that 3.8% of the population had experienced at least 1 hospitalization due to TBI by 35 years of age. The Christchurch New Zealand birth cohort found that by 25 years of age 31.6% of the population had experienced at least 1 TBI, requiring medical attention (hospitalization, emergency department, or physician office). An estimated 43.3% of Americans have residual disability 1 year after injury. The most recent estimate of the prevalence of US civilian residents living with disability following hospitalization with TBI is 3.2 million."[3]
Mechanism of Injury
[edit | edit source]
Closed head injury[edit | edit source]
Often occurs as a result of RTA, or a blow to the head, or a fall where the head strikes the floor or another hard surface..
In closed head injury, the skull is not penetrated, but it is frequently fractured.
Generally there is both focal and diffuse axonal damage.
Open head injury[edit | edit source]
This is caused by a penetrating wound, eg. by a weapon or from a bullet.
In these cases the skull is penetrated.
The brain injury is usually largely focal axonal damage.
Deceleration injury[edit | edit source]
This frequently occurs in RTA, when rapid deceleration occurs as the skull meets a stationary object, causing the brain to move inside the skull.
Mechanical brain injury occurs due to axonal shearing, contusion and brain oedema.
Pathological Process[edit | edit source]
Mechanical Damage[edit | edit source]
AKA Primary Damage and Primary Insult. Primary mechanical brain injury is the direct injury to the brain cells caused by the initial impact.
The mechanical forces can cause intracranial haematoma [ defined as "a localised swelling that is filled with blood caused by a brea in the wall of a blood vessel"] and/or vascular injury, as well as injury to cranial nerves.
Intracranial haematomas are categorised in the following way:
- Epidural haematomas
- Subdural haematomas
- Subarachnoid haematomas
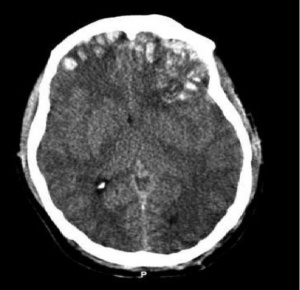
In the CT scan image shown here, skull fractures are visible, as well as multiple frontal, parietal and emporal lobe contusions with a subdural haematoma on the left isde as well as associated interhemispheric haemorrhages.
Delayed non-mechanical Damage[edit | edit source]
AKA Secondary Damage. Non-mechanical brain injury is caused by ischaemic[4], cytotoxic and inflammatory processes.
One of the most significant factors is the excessive release of glutamate and aspartate, which alter cell wall permeability which ultimately leads to destruction of axons[5].
Clinical Presentation[edit | edit source]
The presentation depends on the areas of the brain which have been damaged.
One of the early signs of TBI, often developing a week after the head injury, is the onset of spasticity.
Spasticity symptoms include hypertonicity and spasm of the affected muscles and an increase in deep tendon reflexes; it's severity can range from mild stiffness of the muscles to severe (and painful) muscle spasms.
Classifiation of TBI[edit | edit source]
There are 3 ways of classifying head injury:
- Patho-anatomic ie. what damage has occurred where in the brain, for instance, subdural haemorrhage
- Injury severity, typically using the Glasgow Coma Scale as the measure, where a score of 8 or less is defined as Severe TBI
- Physical mechanism causing the injury, categorised as contact or "impact" loading when the head is struck or strikes an object, as oppsed to noncontact or "inertial" loading (which is when the brain moves within the skull.
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Changing patterns in the epidemiology of traumatic brain injuryfckLRBob Roozenbeek, Andrew I. R. Maas & David K. Menon Nature Reviews Neurology 9, 231-236 (April 2013)
- ↑ Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Faul M, Xu L, Wald MM, Coronado VG. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010
- ↑ The Epidemiology of Traumatic Brain InjuryfckLRCorrigan, John D. PhD, ABPP; Selassie, Anbesaw W. DrPH; Orman, Jean A. (Langlois) ScD, MPH The Epidemiology of Traumatic Brain Injury March/April 2010 - Volume 25 - Issue 2
- ↑ Ischaemic brain damage in fatal non-missile head injuries. Graham DI, Adams JH, Doyle D. J Neurol Sci. 1978, 39 (2–3): 213-34
- ↑ Axonal Damage in Traumatic Brain Injury. Smith DH, Meaney DF. The Neuroscientist. 2000, 6: 483-495