Myelopathy
Original Editors - Bram Van Laer
Top Contributors - Lena Vanderaa, Simisola Ajeyalemi, Vidya Acharya, Admin, Manisha Shrestha, Rachael Lowe, Kim Jackson, Tony Lowe, Kai A. Sigel and Karen Wilson
Search Strategy[edit | edit source]
Databases
• Pubmed
• Web of Knowledge
• Google Scholar
• Medscape
Search Words
• Myelopathy
• Lumbale myelopathy
• Thoracic myelopathy
• Compressive myelopathy
Definition/Description[edit | edit source]
Myelopathy is a term used to describe any neurologic deficit related to the spinal cord. It’s usually due to compression of the spinal cord by osteophyte or extruded disc material. It is most commonly localized in the cervical spine but it can also occur in the thoracic and lumbar spine.5
There are many primary infectious, inflammatory, neurodegenerative, neoplastic vascular, idiopathic and nutritional disorders that results in myelopathy. These causes are much less common than disco genic diseases, metastases or trauma. Further explanations will be given in the following paragraphs.5
To determine the grade of severity of the myelopathy you can use the Nurick classification. The classification is based on abnormalities in the patient’s gait.7 This evaluation has demonstrated its sensitivity and validity. 8
The diagnosis of myelopathy depends on the neurological localization in the spinal cord, rather than the brain or peripheral nervous system. Also, the presence or absence of significant pain or trauma and the mode of onset is primordial to assess the myelopathy into clinical categories.5
Clinically Relevant Anatomy[edit | edit source]
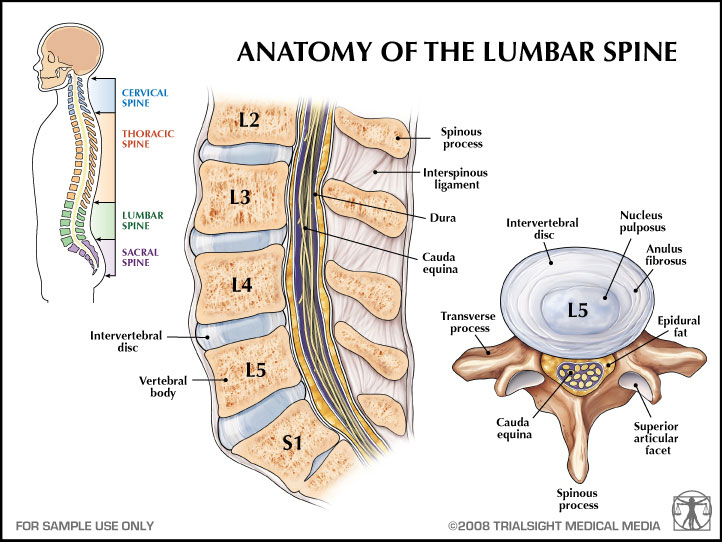
The spinal column begins in the cervical region under the skull. It continues into the thoracic region and finally into the lower back where it connects to the sacrum and pelvis. The cervical region consists of 7 vertebrae, the thoracic region of 12 vertebrae and the lumbar region of 5 vertebrae.
Between the corpus and the proccesus of the vertebrae is the spinal canal. It’s a region in the middle of the spine where the spinal cord goes down and nerves travel toward the extremities. The brain and the spinal cord are packed in 3 membranes: dura mater, arachnoid mater and pia mater. Each one has their own structure and function.
Even though the spinal cord is well protected, it can be damaged by epidural or intradural causes. This is what’s happens when we’re talking about myelopathy.11
Epidemiology /Etiology[edit | edit source]
Myelopathy can sometimes be a slow process. The symptoms can develop slowly over a period of months or it can go very fast.
It’s difficult to clinically distinguish myelopathy from other non-traumatic causes of myelopathy because the classic history is frequently absent or difficult to elicit from a seriously ill patient.
There are many risk factors that may cause or occur thoracic myelopathy.
Thoracic myelopathy occurs because of:
• Discus hernia5
• Spinal degeneration
• Facet degeneration
• Ligamentum flavum hypertrophy2,4
• Calcification of ligamentum flavum2,4
• Compression due to extradural mass (Spinal tumors)5
• Posttraumatic deformities5
• Infections5
• Angular kyfose (congenital, tuberculous, neurofibromatosis and posttraumatic kyphosis)3
• Vascular disorders (vascular malformations, spinal cord infarct and epidural hematoma)5
• Nutritional disorders5
Risk factors1:
1. Age
2. Degrees of motor and sensory deficits
Degrees of spinal cord compression, absence of proximal stenosis and intramedullary hypertension this factors predicted the surgical outcome.
Characteristics/Clinical Presentation[edit | edit source]
Following characteristics may occurs:
• Muscle weakness
• Alterned muscle tonus
• Sensory loss (in trunk and legs) and spasticity
• Impaired coordination
• Walking problems1,2
• Backache2
• Urinary disturbances
(Sometimes the patients have hypotony of theirs mucles.)
Differential Diagnosis10[edit | edit source]
It can be difficult to diagnose myelopathy because the clinical presentations are variable and sometimes like those of other disorders. That’s why it’s important to have a thorough history and complete physical examination of the patient.
In this case, it is very difficult to know which symptoms appear by myelopathy or to the mediated disorders.
Other pathologies that can be involved in myelopathy are:
• Spinal stenosis
• Discus hernia
• Spondylolistheses
• Discus bulging
Diagnostic Procedures[edit | edit source]
Imaging of the myelopathy is crucial.
Primary method:
Magnetic resonance imaging (MRI)2,3,5
This can show a reduced spinal cord diameter or abnormalities in the cord and hypertension in the central cord.
Other methods:
1. Computed tomography (CT)2,5 - You can see bony injury’s or ligamentous injury’s, when they are present
2. Myelogram2
3. Radiographs5 - Radiography may depict osteophytic narrowing of the spinal canal or bone destruction
Diagnosis of myelopathy depends on the neurologic localization.5
Outcome Measures[edit | edit source]
• Nurick classification
• The Japanese Orthopedic Asoociation scale (JOA)
• ODI
• VAS – scale
Examination[edit | edit source]
Diagnosis of myelopathy rest on demonstration of mechanical stability of the spine. We should note that MRI is considered as the golden standard to diagnose myelopathy.6
Physical examination results commonly in long tract signs such as spasticity, hyperreflexia and abnormal reflexes. Hoffmann, Babinski, and clunus are frequently tested reflexes7. Someone with myelopathy has a positive Hoffman and/or Babinski and/or clunus test. We also frequently notice progressive deterioration in their hand and gait function. So, it can be useful to examine the gait cycle of the patient with a toe-to-heel walk and the Romberg test.
Myelopathy leads to generalized weakness and intrinsic muscle wasting. That’s why it’s also important to test some muscles with tests such as the Finger escape sign or the Rapid grip and release test.7
The Japanese Orthopaedic Association scale can help us to assess the severity of clinical symptoms in patients with myelopathy.9 It consists of 6 scales (motor dysfunction in upper extremities, motor dysfunction in the lower extremities, sensory function in the upper extremities, sensory function in the trunk, sensory function in the lower extremities and bladder function) based on motor and sensory functions which are individually graded with a maximal score of 17.7,9 We should note that there exists a modified Japanese Orthopaedic Association score used in Europe. The two scores showed a good correlation with each other in terms of their total scores and recovery rates.9
More specific information about physical examination for cervical myelopathy can be read on this page.
Medical Management
[edit | edit source]
Conservative management, such as physical therapy, cervical immobilisation or anti-inflammatory medication is preferred. But when patients have intractable pain or progressive neurological symptoms surgical interventions are needed.13
As we mentioned above myelopathy is usually due to compression. When surgical intervention is needed, we will focuse on decompression of the spinal cord and nerve roots. Deformity prevention by maintaining or supplementing spinal stability will be another goal of this intervention.13
There are many techniques describes to decompress the spinal cord and roots which can be anterior, posterior or circumferential. The choice of the most effective technique is dependent on numerous factors such as location, comborbidity, stability of spinal column and surgeon’s experience.13
The following surgical techniques can be used to decompress the spinal cord:
- Laminectomy, a posterior approach thas has been proven to be a safe and effective technique
- Laminoplasty, a posterior approach developed to allow cord decompression while preserving motion with less substantial alteration of the natural biomechanics
- Anterior Cervical Disectomy, effective for ventral pathology such as osteophyte or disc complexes
Anterior Cervical Corpectomy, effective in pathology extends beyond the spine interspaces
When we look at the efficacy of a laminectomy and a laminoplasty we see that they bothshow an improvement in clinical disease severity, functional status and quality of life as far as 24 months of measurments show in patients wit degenerative cervical myelopathy. 23
When we look at to the differences between anterior and posterior laminectomy in patients with cervical spondylotitic myelopathy, we see that there are none concerning the health related outcome measurments. We do see that the anterior aproach is more often used in younger patient weer the myelopathy is less severe.25
When we look at compressive myelopathy, at first we see that lumar spine stenose can be a risk factor. Secondly we see that metastatic compression of the spinal cord can occur in myelopathy.
Lumbar spinal stenose can be treated conservatively with use of medicatcation wich will focuse on increasing the bloodvesel diameter and with this the bloodflow. This becaus the diameter of the blood vessels in the cauda equina in LSS patiënts is significnatly smaller than the diameter of blood vessels in heathy individuals.
Medication : vitamins, NSAID’s, muscle relaxers and prostaglandines.
Non operative treatment also consist physical therapy, epidural injection and facet joint injections. When doing a follow up (until 6 months) on LSS patients who onderwent non surgical treatment, we conclude that there is a significant pain relief and improvement in physical function 3 months follow up and an significant improvement in COMI scores on 6 month follow-up.17 There is no diffence found between treating LSS patients with epidural steroid injections and physical therapie, both of whom are suplemented with a home -based excersice program and received declofenac. Although both treatments didn’differ, they showed a significant improvement with the controlegroup.18
Lumbar spinal senose can be treated surgically by the decompressive mild procedure. This is a minimally invassive procedure in which they wil remove part of the posterior fibers of the hypertrophic ligamentum flavum and some interlaminar bone while maintaining anatomy, stability and biomechanics of the lumbar spine.
The use of the decomrpessive mild procedure is shown that … in comparison with an open laminectomy surgerylaminectomy :
- There are less complications
- There are less / none instability problems found post operative
- have a shorter operating lenght
- hav less blood loss
- hospitalisation time is smaller (the same day released)
- patient saftyis much better
when the mild procedure is used, there is a continiousepidurographic leteral oblique fluorscopic imaging.
Metastatic spinal cord compression is an other cause for compressive myelopathy.
Spinal tumors are classified in 3 sorts : extradural, intradural extramedularry an intradural intramedullary. These Metastatic spinal cord compression is diagnosed in 2,5 –5% of the cancer patients.21
The type of medical management of these tumors will depend on the stability of the spine, neurological and pain status.
A surgical intervention is indicated when :
- patient experiences paraplegia not more than 12 – 24 hours
- spinal instability
- bony compression of the spinal cord
A surgical intervention is performed to preserve neurological funtion en pain and will improve median survival rates for at least 6 months. Post operative complications are respiratory complications, deep venous thrombosis, pulmonary embolism, cerebrospinal fluid leek and wound infection.
Radiation therapy can be applied post operatively and can have beneficial effects when used in combination with corticosteriods or with Dexamethasone is used berore radiotherapy (higher ambulatory rate).4
In patiënt with a good prognosis, radiotherapie is indicated to relief pain, preserve or improve neurological function.
In patients with poor prognosis, who have a life expectance of 6 months, radiotherapy will not help on the matter of neurological function and wil just offer pain relief
A single dose radiation scadule is assosiated with higher in-field recurrance.5
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.