Musculoskeletal Injury Risk Screening: Difference between revisions
(formatting) |
(adding content on various screening tests) |
||
| Line 47: | Line 47: | ||
=== Injury Prediction === | === Injury Prediction === | ||
Can we predict injuries | Can we predict injuries | ||
Association vs prediction articles | Association vs prediction articles | ||
| Line 189: | Line 189: | ||
* Build ways to improve the skill in a controlled environment but then also in training and competition environments | * Build ways to improve the skill in a controlled environment but then also in training and competition environments | ||
== | === Examples of Screening Tests === | ||
[[Functional Movement Screen (FMS)]] | |||
[http://s3.amazonaws.com/ustaassets/assets/1/15/11940_highperformance_profile_lowres.pdf United States Tennis Association High Performance Profile] | |||
[https://www.researchgate.net/publication/311426830_The_nine_test_screening_battery_-_Normative_values_on_a_group_of_recreational_athletes Nine Test Screening Battery] | |||
Lower Quadrant Tests | |||
Single-leg squat | |||
Single-leg landing | |||
Drop Jump Test | |||
Star Excursion Balance Test | |||
Hop for distance tests | |||
Upper Quadrant Tests | |||
GIRD | |||
Closed chain upper limb test | |||
== Resources == | == Resources == | ||
Revision as of 17:58, 25 August 2021
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (25/08/2021)
Original Editor - User Name
Top Contributors - Wanda van Niekerk, Jess Bell, Kim Jackson, Tarina van der Stockt, Uchechukwu Chukwuemeka and Lucinda hampton
Introduction[edit | edit source]
Reasons for the Periodic Medical Assessment of Athletes[edit | edit source]
The main reason for the periodic medical assessment of athletes is to safeguard sports participation, but there are many more beneficial reasons as well. Some of the reasons include[1]:
- Identification of medical conditions that contraindicate sports participation
- Assessment of known injuries and illnesses
- Review of current medications and supplements
- Athlete education
- Baseline testing
- Development of athlete rapport
- Specific Screening
- Cardiac screening
- Screening for unknown illnesses
- Screening for risk factors for future injury
Why Screen for Injury Risk?[edit | edit source]
Injury rates in sports are increasing despite the increased professionalism of sports science and sports medicine support teams. Although participation in sport is encouraged as part of a healthy lifestyle, the sport-related injury burden is high.[2]
Consequences of Injuries in Sport[edit | edit source]
- Financial implications for the club
- The cost of player injuries on sports leagues and organisations mainly fall into two categories: the direct medical costs and the opportunity cost of time loss injuries and shortened careers. This has led to professional teams offering players contracts contingent upon medical evaluations and players with high injury risk being offered short-term contracts.[3]
- Team performance
- A significant relationship of injury rates and time loss with performance in elite team sports is reported.[4]
- Financial implications for the healthcare system
- Financial costs for the individual
- The inability to perform has significant impact on an athlete’s earnings. Secrist et al[6] showed that players in the National Football League with an ACL injury earned on average $2,070,521 less than salary-matched controls over the 4 years after the injury.
- Implications for long term health
- It has been shown that knee injuries such as ACL or meniscal injury increases the odds of subsequent knee OA development[7]
- Career progression in sports
Injury Prediction[edit | edit source]
Can we predict injuries
Association vs prediction articles
Factors Involved in the Development of Injuries[edit | edit source]
There are various factors that play a role in the risk of injury occurrence, and these factors can interact with each other: [9]
- Training-related factors
- Training volume, load, intensity
- Type of training
- Training and competition schedule
- Rest
- Motor control factors
- Posture
- Movement patterns
- Muscle tone
- Technique
- Sport specific movements
- Psychological factors
- Beliefs
- Fears
- Coping strategies
- Self-efficacy
- Catastrophising
- Emotional status (stress, depression, anxiety)
- Health-related factors
- Diet
- Medication
- General health
- Fatigue
- Sleep patterns
- Non-modifiable factors
- Gender
- Age
- Maturation stage
- Body type
- Genetics
- Previous injuries
- Environmental factors
- Training/competition surface
- Equipment
- Clothing
- Weather
- Coaching
- Conditioning factors
- Strength
- Endurance
- Muscle length
- Joint range of motion
- Chronic capacity
- Additional demands
- Home
- Work
- Family
- Social
- Leadership
- Media
- Sponsors
- Other factors
- Sport specific skill level
- Ranking and status
- Goals of athlete – short and long term
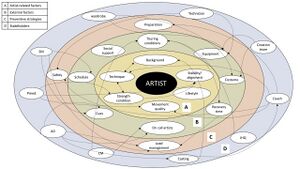
When considering injury screening it is important to consider this myriad of factors that can influence injury occurrence. Furthermore, it is unlikely that these can be reduced to a single factor that may lead to injury occurrence.[9] Factors that are commonly screened for in musculoskeletal injury risk screening are:
- strength and conditioning
- movement quality
- stability/alignment
From the map by Bolling et al[10] it is evident that these factors are just a few of numerous factors that can be involved in injury occurrence.[10]
Predisposition to Injuries[edit | edit source]
Instead of trying to predict injury occurrence, it may be more appropriate to identify athletes who are predisposed and where possible modify the predisposition.
- Non-modifiable predispositions include:
- Anatomy
- Genetics
- Previous injury
- Environmental factors
- Modifiable predispositions include:
- Strength
- Movement
- Skill
- Flexibility
- State of the athlete eg. tired or stressed?
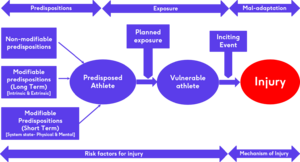
This flow diagram created by Dr Lee Herrington illustrates how predispositions and exposure to load can lead to vulnerability in an athlete and in combination with an inciting event this can lead to injury mechanisms and occurrences.
Considerations in Identifying Predisposed Athletes[edit | edit source]
- Understand the nature of the sport and the injuries occurring
- Common injuries vs Catastrophic injuries (for example hamstring injuries vs ACL injuries soccer)
- Identify which injury needs to be targeted as this will determine what types of screening tests will be used
- Do these specific injuries have modifiable factors?
- Are there clearly definable physical qualities related to the injury? ? Can these modifiable factors be clearly defined in terms of certain physical qualities?
- Can these physical qualities be identified with reliable screening tests?
- Can these physical qualities be influenced, modified or changed? (For example – blue eyes may be a predisposing factor to a certain type of injury and can easily and reliably be screened for, but eye colour can not be changed, modified or influenced.)
- Traumatic injuries in the sport – how influenceable are traumatic injuries through screening and training?
Screening for Neuromuscular Control of Movement[edit | edit source]
Neuromuscular control is the ability to perform a movement in the best possible way to minimise loading stress or maximise the distribution of loading stresses on the tissue involved.[9] An important part of “movement screening” is to identify the high-risk movement tasks and can these tasks be broken down into closed skills. A closed skill is undertaken in a controlled environment where the athlete only focuses on that specific skill (e.g. single leg squat or single-leg landing).[9] An open skill is undertaken in a very chaotic and random environment (e.g. single-leg landing in the middle of a sporting environment such as competition or match). The context in which these movements take pace will have an influence on performance as well as the risk for injury. For example, an athlete may pass a closed skill test/task such as single-leg landing at the pre-season screening, but still get injured (i.e. ACL injury) as a result of a single-leg landing in a sporting environment such as a competition.
Selecting a Screening Test/Task[edit | edit source]
Factors to consider when selecting a screening test or task include[9]:
- Nature of activities undertaken in the specific sport
- Nature of the major injuries in the specific sport (are these linked to specific movements or activities?)
- Athlete’s injury history (can the previous injuries be linked to specific movements or activities?)
Factors Influencing Neuromuscular Control of Movement[edit | edit source]
Various factors can have an impact on an athlete's ability to perform a specific screening test or task. These include[9]:
- Strength
- Joint range of motion
- Muscle length – flexibility
- Proprioception – joint position sense
- Movement dissociation
- Sport specific skill
Building a Paradigm for Injury Risk Screening[edit | edit source]
- Consider Predisposition vs Prediction of injuries
- Screening tests can’t predict if an athlete will get injured, but we can screen and look for predisposed athletes. Remember that being predisposed to a certain injury does not mean that the athlete will get injured. Also, if an athlete does not have a predisposition to an injury, this is not a guarantee that the athlete won’t be injured. Athletes become vulnerable to injury when they are exposed to load and inciting events. (see flow diagram)
- Identify if force generation, force absorption or movement skill is an issue in predisposition
- Identify the predisposing movement task/s
- Break down the identified movement task into close skills that can be measured reliably
- If the athlete fails the test/task, identify the reasons for failure
- Build ways to improve the skill in a controlled environment but then also in training and competition environments
Examples of Screening Tests[edit | edit source]
Functional Movement Screen (FMS)
United States Tennis Association High Performance Profile
Lower Quadrant Tests
Single-leg squat
Single-leg landing
Drop Jump Test
Star Excursion Balance Test
Hop for distance tests
Upper Quadrant Tests
GIRD
Closed chain upper limb test
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Targett S, Clarsen B. Periodic medical assessment of athletes. In: Brukner P, Clarsen B, Cook J, Cools A, Crossley K, Hutchinson M, McCroy P, Bahr R, Khan K. Brukner and Khan's Clinical Sports Medicine: Injuries, Volume 1, 5e. Sydney: McGraw Hill Education. 2017
- ↑ Emery CA, Pasanen K. Current trends in sport injury prevention. Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):3-15.
- ↑ Walia B, Boudreaux CJ. The cost of players’ injuries to professional sports leagues and other sports organizations. Managerial Finance. 2020 Jul 31.
- ↑ Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. British journal of sports medicine. 2013 Aug 1;47(12):738-42.
- ↑ 5.0 5.1 Finch CF, Kemp JL, Clapperton AJ. The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004–2010: a future epidemic of osteoarthritis?. Osteoarthritis and cartilage. 2015 Jul 1;23(7):1138-43.
- ↑ Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes. Orthopaedic journal of sports medicine. 2016 Aug 30;4(8):2325967116663921.
- ↑ Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4-6 fold after knee injury–a systematic review and meta-analysis. British journal of sports medicine. 2019 Dec 1;53(23):1454-63.
- ↑ 8.0 8.1 Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. Injuries are negatively associated with player progression in an elite football academy. Science and Medicine in Football. 2021 Jun 16(just-accepted)
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Herrington LC, Munro AG, Jones PA. Assessment of factors associated with injury risk. In: Performance Assessment in Strength and Conditioning 2018 Oct 9 (pp. 53-95). Routledge.
- ↑ 10.0 10.1 Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil. BMJ open sport & exercise medicine. 2019 Feb 1;5(1):e000492.
- ↑ Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil. BMJ open sport & exercise medicine. 2019 Feb 1;5(1):e000492.