Muscular Dystrophy: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 12: | Line 12: | ||
There is no cure for MD. Physiotherapists and other health professionals work on improving muscle and joint function and slowing muscle deterioration so people with MD can live as actively and independently as possible. | There is no cure for MD. Physiotherapists and other health professionals work on improving muscle and joint function and slowing muscle deterioration so people with MD can live as actively and independently as possible. | ||
== | == Aetiology == | ||
[[File:MuscularDystrophy.png|right|frameless|400x400px]] | [[File:MuscularDystrophy.png|right|frameless|400x400px]] | ||
Muscular dystrophy most often results from defective or absent glycoproteins in the muscle membrane. Each type of muscular dystrophy results from different gene deletions or mutations, causing various [[Enzymes|enzymatic]] or metabolic defects. | Muscular dystrophy most often results from defective or absent glycoproteins in the muscle membrane. Each type of muscular dystrophy results from different gene deletions or mutations, causing various [[Enzymes|enzymatic]] or metabolic defects. | ||
| Line 61: | Line 61: | ||
== Physiotherapy == | == Physiotherapy == | ||
[[File:Pool.jpg|right|frameless]] | [[File:Pool.jpg|right|frameless]] | ||
The goal of | The goal of physiotherapy is to improve strength in the large muscle groups and prevent scoliosis and contractures. According to the literature, the role of muscular exercise is controversial. Whether exercises can benefit patients? The data and evidence on the effectiveness of rehabilitation management of muscular dystrophies are limited. Since muscular dystrophy results in a progressive loss of muscle mass and strength, exercise may be considered harmful because it can induce damage, inflammation, and failure of the muscles to repair themselves<ref>Physiospot. [https://www.physiospot.com/research/exercise-for-muscular-dystrophy/ Exercise for Muscular Dystrophy | Apply Caution]| Article of The Week #20.December 14, 2020 by Scott Buxton</ref>. The muscle degeneration in muscular dystrophy may impose the risk of exercise-induced adverse effects such as overwork weakness following supramaximal, high-intensity exercise. However, the lack of physical activity may lead to functional loss, weight gain, fatigue, and an exacerbation and acceleration of the effects of muscular dystrophy<ref name=":4">Gianola S, Castellini G, Pecoraro V, Monticone M, Banfi G, Moja L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7688624/ Effect of muscular exercise on patients with muscular dystrophy: a systematic review and meta-analysis of the literature.] Frontiers in neurology. 2020:958.</ref>. A Systematic Review and Meta-Analysis of the Literature reviewing evidence for benefits of muscular exercises on patients with muscular dystrophy concludes that muscle exercises improve endurance during walking in most patients, though muscle exercises cannot be recommended for strength improvement, management of motor abilities, or fatigue reduction<ref name=":4" /> | ||
Physical therapy for muscular dystrophy may involve: | Physical therapy for muscular dystrophy may involve: | ||
Revision as of 23:41, 19 April 2023
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Jess Bell, Robin Tacchetti, Vidya Acharya, Rucha Gadgil, Olajumoke Ogunleye, Tarina van der Stockt, Kim Jackson, Uchechukwu Chukwuemeka, Kehinde Fatola and Shreya Pavaskar
Introduction[edit | edit source]
The term "muscular dystrophy" incorporates an assortment of hereditary disorders that lead to progressive, generalized disease of the muscle prompted by inadequate or missing glycoproteins in the muscle cell plasma membrane. Muscular dystrophy (MD) is a non-communicable disorder with abundant variations. Each has its pattern of inheritance, onset period, and the rate at which muscle is lost. Alterations in specific genes cause different representations of this disease[1].
Muscular dystrophies are characterized by progressive muscular atrophy and weakness. In most varieties the muscles of the limb girdles (the pelvic and shoulder muscles) are involved[2]. Over time, people with MD lose the ability to do things like walk, sit upright, breathe easily, and move their arms and hands[3].
There is no cure for MD. Physiotherapists and other health professionals work on improving muscle and joint function and slowing muscle deterioration so people with MD can live as actively and independently as possible.
Aetiology[edit | edit source]
Muscular dystrophy most often results from defective or absent glycoproteins in the muscle membrane. Each type of muscular dystrophy results from different gene deletions or mutations, causing various enzymatic or metabolic defects.
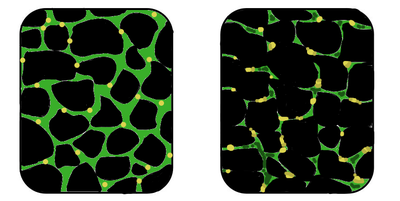
Images: In the affected muscle (right), the tissue has become disorganized and the concentration of dystrophin (green) is greatly reduced.
Dystrophin forms an integral part of a muscle's cytoskeleton and links the contractile apparatus to the sarcolemma.
- In 1986, researchers discovered the gene that, when defective or flawed, causes Duchenne muscular dystrophy. The muscle protein associated with this gene was named dystrophin.[4] The dystrophin gene is the largest in the human genome, with 79 exons. The dystrophin gene is subject to a high rate of spontaneous mutations because of its enormous size (>2 × 106 bases)[1].
- Duchenne muscular dystrophy(DMD) occurs when that gene fails to make dystrophin. Becker muscular dystrophy occurs when a different mutation in the same gene results in some dystrophin, but it's either not enough or it's poor in quality. Scientists have discovered and continue to search for the genetic defects that cause other forms of muscular dystrophy.
- Most muscular dystrophies are a form of an inherited disease called X-linked disorders or genetic diseases that mothers can transmit to their sons even though the mothers themselves are unaffected by the disease[5].
Epidemiology[edit | edit source]
Overall prevalence:
- Muscular Dystrophy: 3.6 per 100,000 people
- Duchenne Muscular Dystrophy: 4.6 per 100,000 people
- Becker Muscular Dystrophy: 1.6 per 100,000 people
** The highest prevalence is in the Americas with 5.1 percent per 100,000 people
** The lowest prevalence is in Africa with 1.7 percent per 100,000[6]
Management[edit | edit source]
There is no cure for muscular dystrophy, but treatments can help manage symptoms and improve quality of life.
1.Medical Interventions
- Anti-arrhythmics
- Anti-epileptics
- Anti-myotonic drugs
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Steroids
2. Surgical Interventions
- Defibrillator or a cardiac pacemaker
- Contracture release
- Shoulder surgery
- Spinal correction
3. Other Interventions
- Supportive physiotherapy
- Supportive bracing
- Supportive counseling
- Genetic counseling[1]
Physiotherapy[edit | edit source]
The goal of physiotherapy is to improve strength in the large muscle groups and prevent scoliosis and contractures. According to the literature, the role of muscular exercise is controversial. Whether exercises can benefit patients? The data and evidence on the effectiveness of rehabilitation management of muscular dystrophies are limited. Since muscular dystrophy results in a progressive loss of muscle mass and strength, exercise may be considered harmful because it can induce damage, inflammation, and failure of the muscles to repair themselves[7]. The muscle degeneration in muscular dystrophy may impose the risk of exercise-induced adverse effects such as overwork weakness following supramaximal, high-intensity exercise. However, the lack of physical activity may lead to functional loss, weight gain, fatigue, and an exacerbation and acceleration of the effects of muscular dystrophy[8]. A Systematic Review and Meta-Analysis of the Literature reviewing evidence for benefits of muscular exercises on patients with muscular dystrophy concludes that muscle exercises improve endurance during walking in most patients, though muscle exercises cannot be recommended for strength improvement, management of motor abilities, or fatigue reduction[8]
Physical therapy for muscular dystrophy may involve:
- Range of motion exercises
- Stretching
- Low-impact workouts, such as swimming or water exercise (aquatic therapy)[5].
- Supportive Bracing: This helps to maintain normal function as long as possible
- Molded ankle-foot orthoses help stabilize gait in patients with foot drop to prevent tripping or to provide support and comfort
- Lightweight plastic ankle-foot orthoses (AFOs) for foot-drop are extremely helpful
- Proper wheelchair seating is essential
- Individuals with scapulohumeral muscular dystrophy remain ambulatory for 40 or more years.
- Occasionally, walking may become hampered by paraspinal muscle contractures; in that case, a wheelchair may assist the individual when covering long distances. [1].
Children at school may need physio interventions such as providing:
- Adaptive or assistive technological devices in the classroom (such as a keyboard for writing)
- Use of a wheelchair or to wear joint braces
- Use of a ventilator for breathing
- Needing special considerations about tardiness, absences, shortened school days, and missed classwork and homework due to physical therapy sessions[3]
Complications[edit | edit source]
The complications of muscular dystrophy depend on the type. Some types are mild, while others are serious and get worse very fast. Worsening muscle weakness can affect the ability to walk, breathe, swallow, and speak. Complications can include:
- Breathing problems. Progressive weakness in the breathing muscles makes it hard to take a breath (raising the risk for eg lung infections such as pneumonia).
- Scoliosis.
- Heart problems. Some types of muscular dystrophy cause abnormal and dangerous changes in the heartbeat (a pacemaker may be needed). Muscular dystrophy can also cause cardiomyopathy leading to heart failure. Most patients die before the age of 30 years due to cardiopulmonary failure.[1]
- Swallowing difficulty. The weakness affects the muscles in the esophagus and causes problems with chewing and swallowing. This can lead to choking. Some people with muscular dystrophy will need a feeding tube.
- Contractures. Bracing and tendon release surgery can help prevent some contractures.
- Vision problems. Some types of muscular dystrophy cause cataracts.[9][10]
- Need for a wheelchair. Some people with muscular dystrophy eventually need to use a wheelchair.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 LaPelusa A, Kentris M. Muscular Dystrophy. StatPearls [Internet]. 2020 Jul 21.Available from: https://www.ncbi.nlm.nih.gov/books/NBK560582/(accessed 24.2.2021)
- ↑ Britannica Muscular Dystrophy Available from: https://www.britannica.com/science/muscle-disease/The-muscular-dystrophies(accessed 24.2.2021)
- ↑ 3.0 3.1 Kidz health MD fact sheet Available from: https://kidshealth.org/en/parents/md-factsheet.html (last accessed 24.2.2021)
- ↑ Allen DG, Whitehead NP, Froehner FC. Absence of Dystrophin Disrupts Skeletal Muscle Signaling: Roles of Ca2+, Reactive Oxygen Species, and Nitric Oxide in the Development of Muscular Dystrophy. Physiol Rev. 2016; 96(1): 253–305.
- ↑ 5.0 5.1 WebMD MD Available from: https://www.webmd.com/children/understanding-muscular-dystrophy-basics?page=-1281(accessed 24.2.2021).
- ↑ Salari N, Fatahi B, Valipour E, Kazeminia M, Fatahian R, Kiaei A, Shohaimi S, Mohammadi M. Global prevalence of Duchenne and Becker muscular dystrophy: A systematic review and meta-analysis. Journal of orthopaedic surgery and research. 2022 Dec;17(1):1-2.
- ↑ Physiospot. Exercise for Muscular Dystrophy | Apply Caution| Article of The Week #20.December 14, 2020 by Scott Buxton
- ↑ 8.0 8.1 Gianola S, Castellini G, Pecoraro V, Monticone M, Banfi G, Moja L. Effect of muscular exercise on patients with muscular dystrophy: a systematic review and meta-analysis of the literature. Frontiers in neurology. 2020:958.
- ↑ Kidd A, Turnpenny P, Kelly K, Clark C, Church W, Hutchinson C et al. Ascertainment of myotonic dystrophy through cataract by selective screening. J Med Genet. 1995; 32:519–23.
- ↑ Kang MJ, Yim HB, Hwang HB. Two cases of myotonic dystrophy manifesting various ophthalmic findings with genetic evaluation. Indian J Ophthalmol. 2016; 64(7):535-7.