Martin Gruber Anastomosis
Original Editor - Nehal Shah
Top Contributors - Nehal Shah and Ewa Jaraczewska
Introduction[edit | edit source]
Anomalous means deviated from normal / routine. Anomalous innervations are routinely a normal occurrence. But if these are not recognised, they may be mistaken for technical pitfall or an actual pathology which may not be present [1] Nerve communication between the median and ulnar nerves in the forearm, is known as Martin-Gruber anastomosis. This implies that nerve fascicles from Median nerve transfers to Ulnar nerve[2]
The prevalence of Martin Gruber Anastomosis (MGA) is between 3.3 to 40% of population [1]with a prevalence of 11.6 % in Indian population [3]Median to Ulnar nerve communication was first described by Martin in 1763 [4]who proposed the possibility of such a communication. This finding was finally confirmed after 100 years by Gruber in in 1870 [5]
Innervation Pattern of Hand[edit | edit source]
| Median Nerve | Ulnar Nerve |
|---|---|
| Abductor Pollicis Brevis | Abductor Digiti Minimi |
| Opponens Pollicis Brevis | Flexor Digiti Minimi |
| Flexor Pollicis Brevis | Opponens Digiti Minimi |
| 1st and 2nd Lumbrical | 3rd and 4th Lumbrical |
| Dorsal and Palmar Interossei | |
| Deep Head of Flexor Pollices Brevis | |
| Adductor Pollices |
Studies suggest that this standard pattern is seen in 33% of cases[6]
Common Patterns of Anamolous Innervations of Median and Ulnar nerves[edit | edit source]
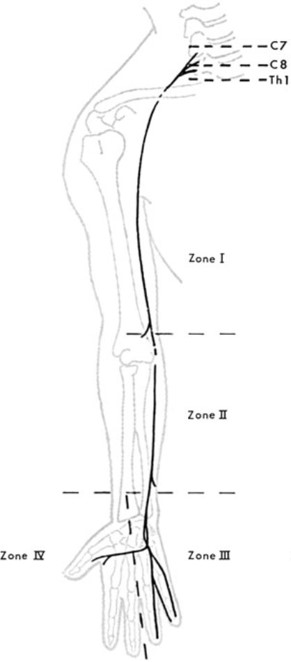
Due to the complexity of anatomy of upper extremity especially the brachial plexus and strategical anatomical zones as cubital tunnel, Guyon canal, carpal tunnel, results in anomalous branching of nerves. They may form anastomosis [2]To understand them better, Mennerfelt et al divided Ulnar nerve in four zones [7]
- ANOMALOUS PATTERN OF INNERVATION IN ZONE I - Usually Flexor Carpi Ulnaris (FCU) muscle innervates at the level of medial epicondyle of Humerus. But it can innervate 4-7 cms proximal to FCU (Sunderland & Hughes, 1946)
- ANOMALOUS PATTERN OF INNERVATION IN ZONE II -
- Isolated branch of Ulnar nerve arises in the middle of the forearm and runs down to supply Ulnar aspect of 4th finger (Turner 1874)
- Dorsal Ulnar Cutaneous nerve which usually arises about 5 cms above wrist
- Variation in the level of innervation of FCU and Flexor Digitorum Profundus IV & V (Sunderland and Hoges 1946)
- Martin Gruber Anastomosis - Anastomosis between Median and Ulnar nerve where there are communicating branch from Median nerve to Ulnar nerve. This is the main anomalous innervation in Zone II
- ANOMALOUS PATTERN OF INNERVATION IN ZONE III - Unusual distribution of Dorsal Ulnar Cutaneous nerve enclosing Pisiform bone (Kaplan 1963)
- ANOMALOUS PATTERN OF INNERVATION IN ZONE IV -
- Double innervation of First Dorsal Interosseus - both by Median and Ulnar nerves (Murphey, Kirklin and Finlayson (1946))
- Double innervation of Lumbricals - Double innervation of any of the Lumbricals by Median and Ulnar nerve (Brooke 1887 and Riche 1897)
- Thenar eminence supplied entirely or partly by Ulnar neve
- Anastomosis between deep ulnar branches and motor branches of the median nerve in the radial part of the palm of the hand.
- Hypothenar muscles innervated entirely or partly by the median nerve.
MARTIN GRUBER ANASTOMOSIS[edit | edit source]
MGA is an anomalous innervation which is formed from cross-over of median-to-ulnar motor nerve fibers which usually takes place in the forearm[1]It can occur bilaterally as well as unilaterally. It occurs bilaterally in 10-40% of detected cases[8]In MGA, a communicating branch arises from the trunk of Median nerve or from any of its branches in the forearm, mainly the Anterior Interosseous nerve. This communicating branch from the Median nerve can innervate any of the intrinsic hand muscles supplied by Ulnar nerve like ADM, FDI, Deep head of FPB, Adductor Pollicis or in any combination of these muscles.[9]
Types of MGA[edit | edit source]
Till date there have been various classification of MGA proposed by various authors. These depend upon the anatomical site of branching of the communicating branch with the most recent classification suggested by Cavalheiro et al described below[2]
- Type I - Nerve fascicles originate from Anterior Interosseus Nerve (AIN) distal to the elbow and join the Ulnar nerve between the proximal and middle one third of the forearm
- Type II - Nerve fascicles originate from AIN, bifurcate into two and communicate with Ulnar nerve at two different points in the forearm
- Type III - Nerve fascicles originate from Median nerve, proximal to the emergence of AIN and head towards joining the Ulnar nerve. These fascicles can originate either proximal or distal to the elbow joint.
- Type IV -The communication occur between the nerve fascicles originating from both Median and Ulnar nerve branches. They head towards FDP muscle mass.
- Type V - Nerve communications occur inside the muscle mass of FDP. This is also called intramuscular MGA
- Type VI - Nerve fascicles arise from the branch of Median nerve to the Flexor Digitorum Superficialis muscle and head towards communication with Ulnar nerve
Various authors have tried to classify MGA and their findings are listed as below table from 1893 to till date[2] -
| Year | Authors | Classification proposed; anastomosis between the median and ulnar nerves |
|---|---|---|
| 1893 | Thomson | Class I: anterior interosseous nerve and ulnar nerve |
| Class II: median nerve and ulnar nerve | ||
| Class III: muscle branch to deep flexor muscle of the fingers | ||
| 1931 | Hirasawa | Oblique anastomosis: anterior interosseous nerve and ulnar nerve |
| median nerve and ulnar nerve | ||
| Loop anastomosis: muscle branch to deep flexor muscle of the fingers | ||
| Combined anastomosis: combinations between others | ||
| 1976 | Kimura et al. | Type I: median nerve and ulnar nerve innervating the hypothenar muscle |
| Type II: median nerve and ulnar nerve innervating the deep flexor muscle of the fingers | ||
| Type III: median nerve and ulnar nerve innervating the thenar muscle | ||
| 1981 | Srinivasan and Rhodes | Types I, II, VI: anterior interosseous nerve and ulnar nerve or other |
| Type III: median nerve and ulnar nerve | ||
| Types IV, V: combinations of others | ||
| 1992 | Uchida and Sugioka | Type I: median nerve and ulnar nerve innervating the hypothenar muscle |
| Type II: median nerve and ulnar nerve innervating the thenar muscle | ||
| Type III: median nerve and ulnar nerve innervating the deep flexor muscle of the fingers | ||
| 1993 | Nakashima | Type Ia: anterior interosseous nerve and ulnar nerve |
| Type Ib: median nerve and ulnar nerve | ||
| Type III: combination of types Ia, Ib and II | ||
| 1995 | Oh et al. | Type I: median nerve and ulnar nerve innervating the hypothenar muscle |
| Type II: median nerve and ulnar nerve innervating the deep flexor muscle of the fingers | ||
| Type III: median nerve and ulnar nerve innervating the thenar muscle | ||
| 1999 | Shu et al. | Type I: anterior interosseous nerve and ulnar nerve |
| Type II: median nerve and ulnar nerve | ||
| Type III: muscle branch to deep flexor muscle of the fingers | ||
| Type IV: anterior interosseous nerve and ulnar nerve, muscle branch to deep flexor muscle of the fingers originating from the connection | ||
| Type V: two anastomotic branches | ||
| 2002 | Rodriguez-Niedenfuhr et al. | Pattern I: one anastomotic ramus |
| Pattern II: two anastomotic rami | ||
| Type A: anastomotic ramus originating from a branch of the median nerve to the nerve of the superficial flexor muscle of the forearm | ||
| Type B: anastomotic ramus originating from the median nerve | ||
| Type C: anastomotic ramus originating from the anterior interosseous nerve | ||
| 2005 | Lee et al. | Type I: anterior interosseous nerve and ulnar nerve |
| Type II: median nerve and ulnar nerve | ||
| Type III: muscle branch to deep flexor muscle of the fingers | ||
| Type IV: two anastomotic rami from the ulnar nerve or anterior interosseous nerve and ulnar nerve | ||
| 2015 | Cavalheiro et al | Type I: anterior interosseous nerve and ulnar nerve |
| Type II: anterior interosseous nerve and ulnar nerve (double anastomosis) | ||
| Type III: median nerve and ulnar nerve | ||
| Type IV: loop between anterior interosseous nerve and ulnar nerve with branches to deep flexor muscle of the fingers | ||
| Type V: intramuscular anastomosis | ||
| Type VI: branch from the median nerve to the superficial flexor muscle and ulnar nerve | ||
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Aziz Saba EK. Electrophysiological study of Martin—Gruber anastomosis in a sample of Egyptians. Egyptian Rheumatology and Rehabilitation. 2017 Oct;44:153-8.
- ↑ 2.0 2.1 2.2 2.3 Cavalheiro CS, Razuk Filho M, Pedro G, Caetano MF, Vieira LA, Caetano EB. Clinical repercussions of Martin-Gruber anastomosis: anatomical study. Revista Brasileira de Ortopedia. 2016 Mar;51:214-23.
- ↑ Kaur N, Singla RK, Kullar JS. Martin–Gruber Anastomosis-A cadaveric study in north indian population. Journal of Clinical and Diagnostic Research: JCDR. 2016 Feb;10(2):AC09.
- ↑ Martin R. Tal om nervers allmänna egenskaper i människans kropp.
- ↑ Gruber W. Ueber die verbindung des nervus medianus mit dem nervus ulnaris am unterarme des menshen und der saugethiere. Arch Anat Phisiol. 1870;37:501.
- ↑ Rowntree T. Anomalous innervation of the hand muscles. The Journal of Bone and Joint Surgery. British volume. 1949 Nov;31(4):505-10.
- ↑ Mannerfelt L. Studies on the hand in ulnar nerve paralysis: a clinical-experimental investigation in normal and anomalous innervation. Acta Orthopaedica Scandinavica. 1966 Mar 1;37(sup87):3-176.
- ↑ Taams KO. Martin-Gruber connections in South Africa: an anatomical study. Journal of Hand Surgery. 1997 Jun;22(3):328-30.
- ↑ Prates LC, de Carvalho VC, Prates JC, Langone F, Esquisatto MA. The Martin-Gruber anastomosis in Brazilians: an anatomical study. Journal of Morphological Sciences. 2017 Jan 16;20(3):0-.