Managing Burns and Limb Trauma
Original Editor - Wanda van Niekerk based on the course by Alicia White
Top Contributors - Wanda van Niekerk, Jess Bell and Tarina van der Stockt
Introduction[edit | edit source]
Limb loss and burn injuries are complex injuries that require the expertise of many members of the multidisciplinary team. This page highlights some factors to consider in persons with amputations and / or burn injuries.
Considerations with Amputations[edit | edit source]
- Zone of Injury
- The zone of injury is the area surrounding a wound that is traumatised but may not appear so.[1][2] Thorough assessment and careful consideration of the zone of injury are needed when deciding the level of amputation.
- Burn injuries produce a definable zone of injury. The Jackson’s Burn Model divides the wound into three zones[3]:
- zone of coagulation
- zone of stasis
- zone of hyperaemia
- read more about the local response to burn wounds here
- A multidisciplinary team approach is necessary to provide person-centred care that will facilitate positive outcomes and optimise quality of life. In cases where emergent amputation is needed (i.e. in situations such as severe sepsis or life-threatening trauma), it is not always possible to get input from the entire multidisciplinary team. However, as soon as the person is medically stable, the team should be involved in formulating the treatment plan.[4] Read more: Multidisciplinary and Interdisciplinary Management of the Amputee.
- Flap techniques
- Different flap techniques may be used to close the wound and create a functional stump. Techniques include:
- Amputation level and energy expenditure
- Energy expenditure and mechanical efficiency are influenced by the length of the residual limb. With more proximal amputations, the metabolic cost of walking is significantly increased – the higher the level of amputation, the more energy is needed for ambulation. For example, walking with a transfemoral prosthesis takes much more effort than a transtibial prosthesis.[7]
- The highest energy requirement is seen in persons with bilateral amputations.
- Aetiology may also influence energy expenditure in persons with amputation.
- Traumatic amputations often occur in younger, healthier individuals with higher baseline activity levels. These individuals can often compensate better, and the energy required for prosthetic gait may be less.
- The baseline activity levels of individuals with vascular disease who require an amputation are usually lower. Thus, the energy expenditure of these individuals is higher as they do not compensate as easily in terms of their endurance and cardiovascular capacities.[8]
- Energy requirements (indicated as a percentage of increased energy expenditure above normal) for different levels of amputation[8]:
- Transtibial amputation - 20-25%
- Bilateral transtibial amputation - 25%
- Transfemoral amputation - 60-70%
- Transtibial/transfemoral - 118%
- Bilateral transfemoral - >200%
- Amputation levels
- Read more about the levels of lower limb amputation and how the level affects weight-bearing, gait and balance: Levels of lower limb amputations
- Surgical techniques
- The goals of amputation surgery include[7]:
- consideration of analgesia - early and continued stages
- optimise the length of the residual limb
- wound healing that allows for prosthesis fitting (essential)
- avoid painful neuromas
- keep other joints supple
- avoid contractures
- early involvement of the multidisciplinary team
- Bevelled or contoured bone ends can reduce discomfort caused by bone edges and prominences
- For wound and scar management, soft tissue flaps should be planned so that the incision and scar are not over weight-bearing areas or bony prominences
- A neuroma is a dissected nerve buried in muscle. Neuromas can cause pain. There have, however, been advancements in physiologic nerve stabilisation, which is a good way to prevent or reduce post-amputation pain.[9] The most common techniques for physiologic nerve stabilisation are[9]:
- Read more here: Evolution of amputee care[9]
- The goals of amputation surgery include[7]:
- Heterotopic Ossificans (HO)
- Heterotopic ossification is defined as "the formation of bone at extraskeletal sites."[10] It is more common in persons undergoing amputation for trauma. The incidence of HO in military people with amputations has been reported to be as high as 65%.[10]
- Non-steroidal anti-inflammatories and local radiotherapy may prevent HO formation.[11] However, these treatments are often contraindicated in patients with complex trauma.[10]
- For symptomatic HO, initial management includes[10]:
- pain management
- physiotherapy
- socket modifications
- If surgical excision is needed, the following should be considered:
- surgery is usually delayed until local inflammation has decreased
- best results are achieved with complete excision of lesions performed at least six months from injury
- wound complications are a risk after excision, but relief of symptoms and patient satisfaction are typically achieved
Wound Healing[edit | edit source]
Key considerations for wound healing in persons with burn injuries:
- Nutritional intake is essential in the recovery and health of people with burn injuries, and medical nutritional therapy is necessary to improve clinical outcomes. Fluid shifts after injury, increased risk for loss of lean body mass and the production of potentially damaging free radicals are all key aspects that need to be addressed with targeted nutritional therapy following major burns.[12]
- Increased caloric intake:
- Protein
- 100 extra calories per each 1% of body surface area burned
- while healing: 1.5 grams of protein per 1 pound (lb) of body weight
- healed: 0.5 grams of protein per 1 pound (lb) of body weight to maintain healed skin
- protein dosage: 20-30 grams throughout the day
- Protein
- Increased caloric intake:
- Sleep
- a minimum of 5 hours of consistent sleep is necessary to assist with wound healing
- hours 0-5 = rest
- hours 5-8 = healing
- Read more:
Contractures[edit | edit source]
- Contracture is common in individuals with burn injuries[13]
- In persons with amputation, contractures may require prosthetic alignment compensations
- Contractures increase energy requirements with ambulation
- Contractures may increase the risk of injury due to asymmetrical ambulation patterns[14]
- Typical contracture patterns in the lower limb:
- hip flexion
- hip abduction
- hip external rotation
- knee flexion
- Prevention and early treatment of contractures are important. Useful techniques to preserve range of motion or to correct contractures include[13]:
- scar management
- stretching
- prolonged positioning
- positioning can be used to minimise the risk of contractures post-amputation. Consider the person's overall health, the level and type of amputation and recommendations from other members of the multidisciplinary team. Some examples to consider:
- transtibial/ below knee amputation - avoid shortening of the hip and knee flexors
- transfemoral/ above knee amputation - avoid shortening of the hip abductors and external rotators
- positioning can be used to minimise the risk of contractures post-amputation. Consider the person's overall health, the level and type of amputation and recommendations from other members of the multidisciplinary team. Some examples to consider:
- adaptive equipment
- for example, use a limb trough while sitting to avoid shortening of the knee flexors
- splinting
- read more: Splinting for Burns
- serial casting
- surgery
Prevention is more manageable than correction! Work smarter, not harder!
Limb Shaping for Amputations[edit | edit source]
Factors that may influence the success of rehabilitation with a prosthesis are[15]:
- the wound
- oedema
- incision scar
- skin condition
- length and shape of the residual limb
- tenderness of the stump
- contractures of adjacent joints
- the distal bone - e.g. bevelled edges, coverage of the flap
- additional / redundant tissue
- "dog ears"
For a proper socket fit, the limb must:
- be conical in shape
- decrease in girth from proximal to distal
- have no bulbous end
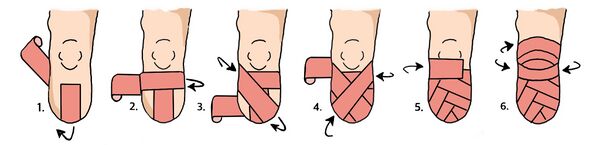
Initially, the residual limb is wrapped as it heals postoperatively with an elastic bandage in a figure of 8 pattern. Read more: Pre-fitting management of the patient with a lower limb amputation.
A shrinker is used once the patient is well-healed and the sutures are removed. The donning of a shrinker can place unwanted shear forces on an unhealed incision. Therefore, it is typically indicated once the surgical wound is healed.[16] The shrinker helps maintain the conical shape and should be worn all the time while the limb is healing. When a patient uses a prosthesis, a shrinker will still be worn in the evenings to help maintain the conical shape.
Prosthetic liners are also referred to as a second skin or artificial skin that adheres to the biological skin. They are used in approximately 85% of clinical prostheses.[17] Goals of a prosthetic liner are to[17]:
- spread and distribute shear stresses between the residual limb and the socket of the prosthesis
- protect sensitive areas such as bony prominences
- suspend the prosthesis on the residual limb
- limit vertical displacement (pistoning) of the limb in the socket
- facilitate heat transmission
- accommodate changes in shape, stiffness and volume of soft tissue
Wear schedules should be set for the patient, rotating the amount of time in and out of the liner/shrinker/socket:
- increase time in the liner, shrinker or socket while decreasing time out of the liner/shrinker/socket
- carefully and closely monitor the skin during the progression of the wear schedule
Scar Management[edit | edit source]
Scar management in persons with amputations:
The effects of scars on function in a person with an amputation include the following:
- scars limit movement in the socket of the prosthesis
- scars promote skin breakdown
- scars decrease sensation
Patient education is key to prevent scar formation.
Read more on:
- Scar management
- Massage, tapping, desensitisation and scar mobilisation
- Desensitisation of the residuum, scar massage and skin care
Scar management in burn injuries:
Read more on outcome measures and management options for scars in burn injuries:
References[edit | edit source]
- ↑ Loos MS, Freeman BG, Lorenzetti A. Zone of injury: a critical review of the literature. Annals of plastic surgery. 2010 Dec 1;65(6):573-7.
- ↑ White A. Considerations in the Management of Amputations and Burns Course. Plus, 2023.
- ↑ Whitaker I, Shokrollahi K, Dickson W. Burns. OUP Oxford, 2019.
- ↑ Keszler MS, Wright KS, Miranda A, Hopkins MS. Multidisciplinary amputation team management of individuals with limb loss. Current Physical Medicine and Rehabilitation Reports. 2020 Sep;8:118-26.
- ↑ Dewi M, Gwilym BL, Coxon AH, Carradice D, Bosanquet DC. Surgical techniques for performing a through knee amputation: a systematic review and development of an operative descriptive system. Annals of Vascular Surgery. 2023 Jan 26.
- ↑ Guest F, Marshall C, Stansby G. Amputation and rehabilitation. Surgery (Oxford). 2019 Feb 1;37(2):102-5.
- ↑ 7.0 7.1 Penn-Barwell JG, Bennett PM. Amputations and rehabilitation. Surgery (Oxford). 2023 Mar 22.
- ↑ 8.0 8.1 Meier RH, Melton D. Ideal functional outcomes for amputation levels. Physical Medicine and Rehabilitation Clinics. 2014 Feb 1;25(1):199-212.
- ↑ 9.0 9.1 9.2 9.3 9.4 Chang BL, Kleiber GM. Evolution of amputee care. Orthoplastic Surgery. 2023 Jun 1;12:1-4.
- ↑ 10.0 10.1 10.2 10.3 Edwards DS, Kuhn KM, Potter BK, Forsberg JA. Heterotopic ossification: a review of current understanding, treatment, and future. Journal of orthopaedic trauma. 2016 Oct 1;30:S27-30.
- ↑ Pakos EE, Ioannidis JP. Radiotherapy vs. nonsteroidal anti-inflammatory drugs for the prevention of heterotopic ossification after major hip procedures: a meta-analysis of randomized trials. International Journal of Radiation Oncology* Biology* Physics. 2004 Nov 1;60(3):888-95.
- ↑ Rollins C, Huettner F, Neumeister MW. Clinician’s guide to nutritional therapy following major burn injury. Clinics in Plastic Surgery. 2017 Jul 1;44(3):555-66.
- ↑ 13.0 13.1 Bryarly J, Kowalske K. Long-Term Outcomes in Burn Patients. Surgical Clinics. 2023 Jun 1;103(3):505-13.
- ↑ Poonsiri J, Dijkstra PU, Geertzen JH. Fitting transtibial and transfemoral prostheses in persons with a severe flexion contracture: problems and solutions–a systematic review. Disability and Rehabilitation. 2022 Jul 17;44(15):3749-59.
- ↑ O'Keeffe B, Rout S. Prosthetic rehabilitation in the lower limb. Indian Journal of Plastic Surgery. 2019 Jan;52(01):134-43.
- ↑ Kwasniewski M, Mitchel D. Post amputation skin and wound care. Physical Medicine and Rehabilitation Clinics. 2022 Sep 28.
- ↑ 17.0 17.1 Yang X, Zhao R, Solav D, Yang X, Lee DR, Sparrman B, Fan Y, Herr H. Material, design, and fabrication of custom prosthetic liners for lower-extremity amputees: A review. Medicine in Novel Technology and Devices. 2022 Dec 8:100197.