Lumbar Motor Control Training: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
No edit summary |
||
| (22 intermediate revisions by 6 users not shown) | |||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File:Physio_1.jpg|alt=|right|frameless]] | |||
[[File:Physio_2.jpg|alt=|right|frameless]] | |||
Motor control exercise is a popular form of [[Therapeutic Exercise|exercise]] that aims to restore [[Coordination Exercises|co-ordinated]] and efficient use of the [[Muscle|muscles]] that control and support the spine. The therapist guides the client to practice normal use of the muscles during simple tasks. As control and skill improve, the exercises are progressed to more complex and functional tasks involving the muscles of the trunk and limbs<ref name=":0">Saragiotto BT, Maher CG, Yamato TP, Costa LO, Costa LC, Ostelo RW, Macedo LG. [https://www.cochrane.org/CD012004/BACK_motor-control-exercise-chronic-non-specific-low-back-pain Motor control exercise for chronic non‐specific low‐back pain]. Cochrane Database of Systematic Reviews. 2016(1). Available:https://www.cochrane.org/CD012004/BACK_motor-control-exercise-chronic-non-specific-low-back-pain (accessed 3.1.2022)</ref>. | |||
During the 1990s and 2000s | During the 1990s and 2000s practitioners across the world began to recognise that the [[Core Muscles|core muscles]] e.g. [[Transversus Abdominis|transversus abdominis]], [[Lumbar Multifidus|lumbar multifidus]] and the [[Pelvic Floor Anatomy|pelvic floor]] need assessment and consideration for inclusion in an integrated treatment program for [[Low Back Pain|low back pain]]<ref name="Bystrom et al 2013">Bystrom MG, Rasmussen-Barr E, Grooten WJ. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/FullText/2013/03150/Motor_Control_Exercises_Reduces_Pain_and.18.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=10701181167903656957&ei=i6KuY96mPOeR6rQPyeixmAI&scisig=AAGBfm3TmtecdOrHQvbQPgPdyQaUVbjUiQ Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis]. Spine (Phila Pa 1976). 2013; 38(6): E350-8</ref>. A 2016 systematic review evaluating the effectiveness of [[Motor Control and Learning|motor control]] exercise (MCE) in patients with [[Chronic Low Back Pain|chronic non-specific low back pain]] concluded: | ||
"MCE probably provides better improvements in [[Motor Control Changes and Pain|pain]], function and global impression of recovery than minimal intervention at all follow-up periods. MCE may provide slightly better improvements than exercise and [[electrophysical]] agents for pain, disability, global impression of recovery and the physical component of [[Quality of Life|quality of life]] in the short and intermediate term. There is probably little or no difference between MCE and [[Manual Therapy|manual therapy]] for all [[Outcome Measures|outcomes]] and follow-up periods. Little or no difference is observed between MCE and other forms of exercise. Given the minimal evidence that MCE is superior to other forms of exercise, the choice of exercise for chronic LBP should probably depend on patient or therapist preferences, therapist training, costs and safety".<ref name=":0" /> | |||
Indeed, since 2016, most evidence is in agreement regarding the lack of difference in outcomes for chronic LBP between motor control exercises compared to other exercises<ref>Grooten WJA, Boström C, Dedering Åsa, Halvorsen M, Kuster RP, Nilsson-Wikmar L, et al. Summarizing the effects of different exercise types in chronic low back pain – a systematic review of systematic reviews. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-022-05722-x BMC musculoskeletal disorders. 2022;23(1):1–801.] | |||
</ref>. | |||
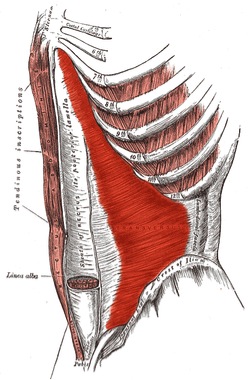
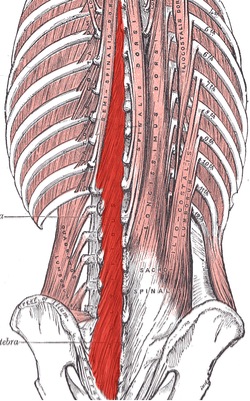
'''Figure 1: Transversus abdominis | '''Figure 1: Transversus abdominis'''<br>'''Figure 2: [[Lumbar Multifidus|Lumbar multifidus]] on the left of the spine''' | ||
== Justification for Use == | |||
Specific motor control training as part of the treatment protocol was based on the principles developed by Richardson and colleagues.<ref name="Richardson et al 2004">Richardson C, Jull G, Hodges P. [https://scholar.google.com/scholar_url?url=http://125.212.201.8:6008/handle/DHKTYTHD_123/7945&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16674606697935355322&ei=tKKuY7HZJOeR6rQPyeixmAI&scisig=AAGBfm0RxzM-OEOlI1b1jJbFc5OycyhLaQ Therapeutic exercise for lumbopelvic stabilisation:] a motor control approach for the treatment and prevention of low back pain. Edinburgh: Churchill Livingstone; 2004</ref>Extensive research has been published on the importance of normal motor control in the lumbar spine including but not limited to:<br>• An anatomical and [[Biomechanics|biomechanical]] suitability of the core muscles for providing stability to structures in the lumbar spine<ref name="Barker et al 2004">Barker P, Briggs, CA, Bogeski, G. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/Fulltext/2004/01150/The_Relation_Between_the_Transversus_Abdominis.5.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=10206056708636316310&ei=1KKuY4TpFtKxywSLm5agCA&scisig=AAGBfm3CuQinJ2e2M3rLpRxz9cIGV9rbJA Tensile transmission across the lumbar fasciae in embalmed cadavers:] effects of tension to various muscular attachments. Spine. 2004; 29: 129-38</ref><ref name="Barker et al 2006">Barker P, Guggenheimer, KT, Grkovic, I, Briggs, CA, Jones, DC, Thomas, CD, Hodges, PW. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/FullText/2006/02150/Effects_of_Tensioning_the_Lumbar_Fasciae_on.6.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=3378781173356912699&ei=9KKuY8jcO9KxywSLm5agCA&scisig=AAGBfm3uKybklTmG9eXbfa2GSZI63FHp6Q Effects of tensioning the lumbar fascia on segmental stiffness during flexion and extension.] Spine. 2006; 31(4): 387-405</ref><ref name="Barker, Briggs 1999">Barker P, Briggs C. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/Fulltext/1999/09010/Attachments_of_the_Posterior_Layer_of_Lumbar.2.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9298866629669642369&ei=FaOuY6yOE46yyAS9hoto&scisig=AAGBfm3RBi5ZBeOuwfr4ktgeJixMgtJBEA Attachments of the posterior layer of lumbar fascia.] Spine. 1999; 24(17): 1757-64</ref><ref name="Panjabi 1992">Panjabi M. [https://scholar.google.com/scholar_url?url=https://www.tigraheerenveen.nl/wp-content/uploads/2017/11/The-Stabilizing-System-of-the-Spine.-Part-I.-Funct-6280KB.pdf&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=11616096125410482423&ei=LqOuY-KzEpCXywSwqaaIDw&scisig=AAGBfm0lqQ27XbNfz6umnMqc_SJj9s_uXg The stabilizing system of the spine]: Part I: Function, dysfucntion, adaptation and enhancement. Journal of Spinal Disorders. 1992; 5: 383-9</ref><ref name="Wilke et al 1995">Wilke H, Wolf S, Claes L, Arand M, Wiesend A. [https://scholar.google.com/scholar_url?url=https://europepmc.org/article/med/7716624&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16929397915265268201&ei=SaOuY8mSNc6TywSl1LXoCA&scisig=AAGBfm1tg5yB-ZxncM8TFdHGBWa2BOLCag Stability increase on the lumbar spine with different muscle groups]. Spine. 1995; 20(2): 192-8</ref><ref name="MacIntosh, Bogduk 1986">MacIntosh J, Bogduk N. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/0268003386901464&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=4300849241011863501&ei=aaOuY7_zB86TywSl1LXoCA&scisig=AAGBfm2APhdeR19ZsWmshLCnua39GIPzlA The biomechanics of the lumbar multifidus]. Clinical biomechanics. 1986; 1: 205-13</ref><ref name="Kaigle et al 1995">Kaigle A, Holm S, Mansson T. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/abstract/1995/02001/experimental_instability_in_the_lumbar_spine.4.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=11908744133629695413&ei=i6OuY8X5BYa8yATUzZGgCg&scisig=AAGBfm0lsKiQ3y2E-DDeCpSRDi933BGdPg Experimental instability in the lumbar spine.] Spine. 1995; 20(4): 421-30</ref><ref name="Hodges et al 2005">Hodges P, Eriksson M, Shirley D, Gandevia S. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S0021929004004105&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=7913455018392281733&ei=q6OuY87zKM6TywSl1LXoCA&scisig=AAGBfm382hAucGiIwRg6tyZJue8hjpqtqg Intra-abdominal pressure increases stiffness of the lumbar spine.] Journal of Biomechanics. 2005; 38(9): 1873-80</ref><ref name="Hodges et al 2001">Hodges P, Cresswell, AG, Daggfeldt, K, Thorstensson, A. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S0021929000002062&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=1193912791330267928&ei=xqOuY-mwCI6yyAS9hoto&scisig=AAGBfm2J3zE6zdniBvgp1Il2FNsY8X4t7A In vivo measurements of the effect of intra-abdominal pressure on the human spine.] Journal of Biomechanics. 2001; 34(347-353)</ref><ref name="Hodges et al 2003">Hodges P, Kaigle, HA, Holm, S, Ekström, L, Cresswell, A, Hansson, T, Thorstensson, A. . [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/fulltext/2003/12010/intervertebral_stiffness_of_the_spine_is_increased.7.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=2292042474031696466&ei=8qOuY8bGI4a8yATUzZGgCg&scisig=AAGBfm3YNcrgm1xv_O9xEKlL4SHXtrtj6g Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies.] Spine. 2003; 28(23): 2594-601</ref> <br>• Feedforward mechanisms in people without a low back disorder (LBD) resulting in “pre-setting” of the core muscles in anticipation of [[Perturbation-Based Balance Training|postural perturbation]]<ref name="Cresswell et al 1994">Cresswell A, Oddsson, L, Thorstensson, A. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/BF00228421&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=2490314075079449303&ei=JaSuY7GyGdKxywSLm5agCA&scisig=AAGBfm3JcrmrX7bXwV0tSCd9-eOx3dZEgw The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing]. Exp Brain res. 1994; 98: 336-41</ref><ref name="Hodges, Richardson 1997">Hodges P, Richardson C. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/PL00005644&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=8335509890907426718&ei=QKSuY8W1BIa8yATUzZGgCg&scisig=AAGBfm2ADmrSBVgHqPaZmQA-9crOI4ODPA Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement]. Exp Brain Res. 1997; 114: 362-70</ref><ref name="Hodges et al 1997">Hodges P, Richardson C. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/ptj/article-abstract/77/2/132/2633127&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=7675833804909184605&ei=aqSuY6GtEYa8yATUzZGgCg&scisig=AAGBfm0sAZ_v0DDSJ8oVDqhiH9-odNl4vA Contraction of the abdominal muscles associated with movement of the lower limb. Physical Therapy]. 1997; 77(2): 132-44</ref> | |||
== | • Contraction of core muscles independent of direction of trunk forces and movements<ref name="Cresswell et al 1992">Cresswell A, Grundstrom H, Thorstensson A. [https://scholar.google.com/scholar_url?url=https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1748-1716.1992.tb09314.x&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9254590330650481097&ei=hKSuY6yLPOeR6rQPyeixmAI&scisig=AAGBfm2x36ysY5JKCyJw3FEqABGDwgxvqA Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man.] Acta Physiology Scandinavia. 1992</ref><ref name="Hodges et al 1999">Hodges P, Cresswell, A & Thorstensson, A. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s002210050601&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9648740362846654895&ei=oKSuY_-qOc6vywS1g6foAw&scisig=AAGBfm3ZYgJ4doixTFP2tmOA5syKq-j1Mw Preparatory trunk motion accompanies rapid upper limb movement.] Exp Brain Res. 1999; 124: 69-79</ref> <br>• Maladaptive differences between people with and without LBD in terms of altered feedforward mechanisms,<ref name="Hodges et al 1996">Hodges P, Richardson C. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/Fulltext/1996/11150/Inefficient_Muscular_Stabilization_of_the_Lumbar.14.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=10508810454767233703&ei=yaSuY92aDtKxywSLm5agCA&scisig=AAGBfm26zcOuhCeoWJZ0WfDuh5bO8nozsg Inefficient muscular stabilisation of the lumbar spine associated with low back pain:] a motor control evaluation of transversus abdominis. Spine. 1996; 21: 2640-50</ref><ref name="Hodges, Richardson 1998">Hodges P, Richardson, CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. Journal of Spinal Disorders. 1998; 11(1): 46-56</ref><ref name="Ferreira et al 2004">Ferreira P, Ferreira M, Hodges P. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/fulltext/2004/11150/changes_in_recruitment_of_the_abdominal_muscles_in.18.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=11835150447014700328&ei=O6WuY5j3EYa8yATUzZGgCg&scisig=AAGBfm3gqE4sNApgVkBNjMK4iBiw_a-d7A Changes in recruitment of the abdominal muscles in people with low back pain:] ultrasound measurement of muscle activity. Spine. 2004; 29(22): 2560-6</ref><ref name="MacDonald et al 2009">MacDonald D, Moseley G, Hodges P. Why do some patients keep hurting their back? [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S0304395908007215&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16314244400437277213&ei=V6WuY-eHN5CXywSwqaaIDw&scisig=AAGBfm3Iv43V09hxzyQdl6gWFLHc1oXuXw Evidence of ongoing back muscle dysfunction during remission from recurrent back pain]. Pain. 2009; 142(3): 183-8</ref>reduced core muscle cross sectional size,<ref name="Hides et al 2010">Hides J, Lambrecht G, Richardson C, Stanton W, Armbrecht G, Pruett C, et al. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s00586-010-1491-x&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=609324647705219577&ei=i6WuY4XQE86TywSl1LXoCA&scisig=AAGBfm3RrbKppKqVoTqoexPJtB0CAFUWGA The effects of rehabilitation on the muscles of the trunk following prolonged bed rest.] European Spine Journal. 2010</ref><ref name="Dickx et al 2010">Dickx N, Cagnie B, Parlevliet T, Lavens A, Danneels L. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S1356689X10000299&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16466028050617926617&ei=pKWuY4imEpCXywSwqaaIDw&scisig=AAGBfm0DzV0NL4flAFtJ3BLVtOTpDcqFBg The effect of unilateral muscle pain on recruitment of the lumbar multifidus during automatic contraction]. An experimental pain study. Manual Therapy. 2010; 15(4): 364-9</ref>increased global muscle activity in certain subgroups<ref name="Dankaerts W et al 2006">Dankaerts W, O'Sullivan P, Burnett A, Straker L. [https://journals.lww.com/spinejournal/fulltext/2006/08010/altered_patterns_of_superficial_trunk_muscle.21.aspx Altered patterns of superficial trunk muscle activation during sitting in nonspecific chronic low back pain patients:] importance of subclassification. Spine. 2006; 31(17): 2017-23</ref>and altered cortical representation of motor patterns<ref name="Tsao et al 2008">Tsao H, Galea M, Hodges P. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/brain/article-abstract/131/8/2161/268528&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16689223255946885989&ei=B6auY_68II6yyAS9hoto&scisig=AAGBfm0NyQ25QMsP2JdquIpaZzKS2WTQMg Reorganization of the motor cortex is associated with postural control deficits in recurrent low back pain]. Brain. 2008; 131(8): 2161-71</ref> | ||
[[File:Back pain lady.jpeg|right|frameless]] | |||
This substantial literature has led to the hypothesis that correcting maladaptive motor control is an important component in the rehabilitation of LBD and prevention of recurrence.<ref name="Hodges, Moseley 2003">Hodges P, Moseley G. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S1050641103000427&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=5181556371848924966&ei=I6auY7GFBOeR6rQPyeixmAI&scisig=AAGBfm14TRBCKcJ9kwoiYiUDjvnJrfgPFg Pain and motor control of the lumbopelvic region:] effect and possible mechanisms. Journal of Electromyography and Kinesiology. 2003; 13(4): 361-70</ref><ref name="Richardson, Hides et al 2004">Richardson C, Hides J, Wilson S, Stanton W, Snijders C. [https://scholar.google.com/scholar_url?url=https://europepmc.org/article/med/16235441&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=30687608771937140&ei=QqauY9bqL-eR6rQPyeixmAI&scisig=AAGBfm3Sg9zGxRRNyNbZZW7ZtOu7PvSRfA Lumbo-pelvic joint protection against antigravity forces]: motor control and segmental stiffness assessed with magnetic resonance imaging. J Gravit Physiol. 2004; 11(2): P119-22.</ref> | |||
* This hypothesis is strengthened based on clinical data showing a reversal of the maladaptive changes observed in people with LBD<ref name="Hides et al 2010" /><ref name="Tsao, Hodges 2007">Tsao H, Hodges P. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s00221-007-0950-z&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=11037989905456936849&ei=Z6auY7yvMYa8yATUzZGgCg&scisig=AAGBfm10-mJ-Gc85sLivtwhEmhAfYyVfKw Immediate changes in feedforward postural adjustments following voluntary motor training.] Experimental Brain Research. 2007; 181(4): 537-46</ref><ref name="Tsao, Hodges 2008">Tsao H, Hodges P. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S105064110700020X&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=18293805487801876232&ei=zKauY6ToI8SYywTZh5fgCg&scisig=AAGBfm1IVgneVMTO2pgQGRBF3JbTkFwyBw Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain]. Journal of Electromyography and Kinesiology. 2008; 18(4): 559-67</ref><ref name="Tsao et al 2010">Tsao H, Druitt T, Schollum T, Hodges P. [https://www.sciencedirect.com/science/article/pii/S1526590010003251 Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain.] The Journal of Pain. 2010; 11(11): 1120-8</ref><ref name="Tsao et al 2010" /><ref name="Vasseljen, Fladmark 2010">Vasseljen O, Fladmark A. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S1356689X10000755&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=3589341455644921894&ei=C6euY-rJNIa8yATUzZGgCg&scisig=AAGBfm35AJaZnY9r-voJVHeimZQl6FX5Nw Abdominal muscle contraction thickness and function after specific and general exercises:] a randomized controlled trial in chronic low back pain patients. Man Ther. 2010; 15(5): 482-9</ref> which is not achieved by less specific exercise such as abdominal bracing or general exercise.<ref name="Ferreira et al 2009">Ferreira P, Ferreira M, Maher C, Refshauge K, Herbert R, Hodges P. [https://bjsm.bmj.com/content/44/16/1166.short Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain]. British Journal of Sports Medicine. 2009; 44(16): 1166-72</ref><ref name="Hall et al 2009">Hall L, Tsao H, MacDonald D, Coppieters M, Hodges P. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S1050641107001708&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=7366745125719554297&ei=V6euY8u4HI6yyAS9hoto&scisig=AAGBfm0Jai81t-86M90psq81OHxWF0Xk_g Immediate effects of co-contraction training on motor control of the trunk muscles in people with recurrent low back pain.] Journal of electromyography and kinesiology: official journal of the International Society of Electrophysiological Kinesiology. 2009; 19(5): 763</ref> | |||
* In addition, RCTs have shown significant improvement for pain and activity in participants receiving specific motor control training compared to usual care<ref name="Ferreira et al 2006">Ferreira P, Ferreira M, Maher C, Herbert R, Refshauge K. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S0004951406700435&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=15789527465057237537&ei=h6euY46eOtLAywSsrIVo&scisig=AAGBfm0_aS-uhO9njqublHROm_zv5sd4jQ Specific stabilisation exercise for spinal and pelvic pain]: a systematic review. Australian Journal of Physiotherapy. 2006; 52(2): 79-88</ref><ref name="Standaert et al 2008" /><ref name="Rackwitz et al 2006">Rackwitz B, de Bie R, Limm H, von Garnier K, Ewert T, Stucki G. [https://scholar.google.com/scholar_url?url=https://journals.sagepub.com/doi/abs/10.1191/0269215506cr977oa&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=2530897818209895447&ei=zqeuY7iaKueR6rQPyeixmAI&scisig=AAGBfm36Dd4d1zWxxUgduhR9Tjy86OOhzA Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials]. Clin Rehabil. 2006; 20(7): 553-67</ref><ref name="Macedo et al 2009">Macedo L, Maher C, Latimer J, McAuley J. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/ptj/article-abstract/89/1/9/2737552&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=14578074909780481506&ei=8qeuY9PoOsSYywTZh5fgCg&scisig=AAGBfm0fnMKo_d7Zp8WNclO8Bs3PZqxcNA Motor control exercise for persistent, nonspecific low back pain: a systematic review.] Physical Therapy. 2009; 89(1): 9-25</ref> with larger effects demonstrable when homogenous subgroups are recruited.<ref name="Hodges 2008">Hodges P. [https://scholar.google.com/scholar_url?url=https://bjsm.bmj.com/content/42/12/941.short&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=7460151779642391648&ei=HaiuY4GsGYa8yATUzZGgCg&scisig=AAGBfm2aqqk_XeEU34I2SFDaeXSnyknW4Q Transversus abdominis:] a different view of the elephant. British Journal of Sports Medicine. 2008; 42(12): 941-4</ref> | |||
* Pain education coupled with cognition-targeted motor control training appears more effective than current best-evidence physiotherapy for improving pain in individuals with chronic LBP.<ref>[https://jamanetwork.com/journals/jamaneurology/fullarticle/2678439 Malfliet A, Kregel J, Coppieters I, De Pauw R, Meeus M, Roussel N, et al. Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA neurology. 2018;75(7):808–17.]</ref> | |||
* Recent controversy around specific motor control training<ref name="Allison, Morris 2008">Allison G, Morris S. Transversus abdominis and core stability: [https://scholar.google.com/scholar_url?url=https://bjsm.bmj.com/content/42/11/930.short&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=793245229566635607&ei=UKiuY8LlKueR6rQPyeixmAI&scisig=AAGBfm2jaMXRLn6bT_tlAMicM7_dP6Abvw has the pendulum swung?] British Journal of Sports Medicine. 2008; 42(11): 630-1</ref><ref name="McGill 2008">McGill SM. Low back disorders: Evidence-based prevention and rehabilitation 2nd ed. Illinois: Human Kinetics Publishers; 2008</ref>has been refuted based on an insufficient consideration of this expansive literature as a whole.<ref name="Hodges 2008" /> | |||
* There is clear and extensive mechanistic and randomised controlled trial based data supporting the rationale for precise motor control training for LBD. | |||
== Clinical Application == | |||
Lumbar motor control training <ref name="Richardson et al 2004" /><ref name="O'Sullivan 2000">O'Sullivan P. [https://scholar.google.com/scholar_url?url=https://fitnessmais.com.br/download/avaliacao-fisica/estabilizacao-01.pdf&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=9664533881687573630&ei=iKiuY47XMIa8yATUzZGgCg&scisig=AAGBfm2sP8k4HY-5MfkLJTV1vk0IQiCKCw Lumbar segmental 'instability']: clinical presentation and specific stabilizing exercise management. Manual Therapy. 2000; 5(1): 2-12</ref> has a large amount of variability in clinical application between physiotherapists.<ref name="Ford et al 2012">Ford J, Hahne A, Chan A, Surkitt L. [https://scholar.google.com/scholar_url?url=https://www.tandfonline.com/doi/abs/10.1179/1743288X11Y.0000000037&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9579384134772287677&ei=qaiuY7vTDZCXywSwqaaIDw&scisig=AAGBfm2B4N8APlis37s3iWlkqyLb5AoyBA A classification and treatment protocol for low back disorders]. Part 3: functional restoration for intervertebral disc related disorders. Physical Therapy Reviews. 2012; 17(1): 55-75</ref>and is commonly reported as a difficult concept to efficiently teach in people with LBD. <ref name="Richardson et al 2004" /><ref name="O'Sullivan 2000" /> <ref name="Standaert et al 2008">Standaert C, Weinstein S, Rumpeltes J. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S1529943007009096&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=14727089578241730639&ei=saeuY8a5INKxywSLm5agCA&scisig=AAGBfm08wq5uDxDrI38dlNmjQzpZYkZlkQ Evidence-informed management of chronic low back pain with lumbar stabilization exercises.] The Spine Journal. 2008; 8(1): 114-20</ref><ref name="Henry, Westervelt 2005">Henry S, Westervelt K. [https://scholar.google.com/scholar_url?url=https://www.jospt.org/doi/abs/10.2519/jospt.2005.35.6.338&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9695838525695579588&ei=xKiuY73eLI6yyAS9hoto&scisig=AAGBfm1SRFXAt0GHRicHP-G3wHzrzZ711A The use of real-time ultrasound feedback in teaching abdominal hollowing exercises to healthy subjects.] Journal of Orthopaedic & Sports Physical Therapy. 2005; 35(6): 338-45</ref><ref name="Hides et al 2008">Hides J, Stanton W, Freke M, Wilson S, McMahon S, [https://scholar.google.com/scholar_url?url=https://bjsm.bmj.com/content/42/10/809.short&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=13817960245410029639&ei=5KiuY-nkOs6TywSl1LXoCA&scisig=AAGBfm2SNif9O6KGZMYQ9hG4fyny_VYbmg Richardson C. MRI study of the size, symmetry and function of the trunk muscles among elite cricketers with and without low back pain.] Br J Sports Med. 2008; 42(10): 809-13</ref> | |||
Now a series of clinical decision making algorithms (based on established protocols) has been developed and validated in a major clinical trial.<ref name="Hahne et al 2011">Hahne AJ, Ford JJ, Surkitt LD, Richards MC, Chan AY, Thompson SL, et al. [https://scholar.google.com/scholar_url?url=https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-12-104&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=11160779804618987712&ei=BamuY9LJC-eR6rQPyeixmAI&scisig=AAGBfm2mnmOskB3OesetWxux1ARjJQl-hQ Specific treatment of problems of the spine (STOPS)]: design of a randomised controlled trial comparing specific physiotherapy versus advice for people with subacute low back disorders. BMC Musculoskeletal Disorders. 2011; 12: 104</ref><ref name="Richardson et al 2004" /><ref name="O'Sullivan 2000" /> | |||
== | == Physiotherapy == | ||
[[File:Drawin.jpg|right|frameless|531x531px]]The goal of the motor control program is to retrain the core muscles of the lumbar spine, comprising [[Abdominal Muscles|transversus abdominis]], lumbar [[Lumbar Multifidus|multifidus]] and the [[Pelvic_Floor_Anatomy|pelvic floor]], to maintain a tonic and automatic contraction<ref name="Ferreira et al 2004" /><ref name="Hides et al 2009">Hides J, Belavy D, Cassar L, Williams M, Wilson S, Richardson C. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s00586-008-0827-2&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=15113427093277221832&ei=YKmuY6uKIY6yyAS9hoto&scisig=AAGBfm11hVlzl4glf98UIAVBzRUONaB20g Altered response of the anterolateral abdominal muscles to simulated weight-bearing in subjects with low back pain.] Eur Spine J. 2009; 18(3): 410-8</ref> at less than 30% of maximum voluntary contraction in daily activities<ref name="Tsao et al 2010" /><ref name="Tsao, Hodges 2007" />. | |||
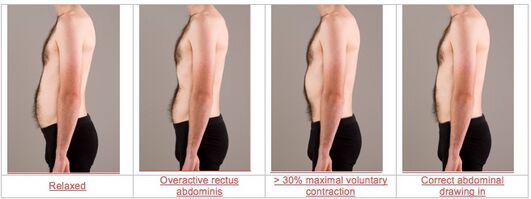
Image 4: Correct and incorrect abdominal drawing in | |||
* In most cases this requires initial training in non-weight bearing positions using a lower abdominal drawing in manoeuvre which has been shown to selectively activate transversus abdominis.<ref name="Hides et al 2010" /> Lumbar multifidus and the pelvic floor muscles, including [[Levator Ani Muscle|pubococcygeus]], have been shown to co-contract with transversus abdominis to provide a “corset” for the [[Lumbo Pelvic Stability|lumbo-pelvic area]]<ref name="Sapsford 2001">Sapsford R. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/S0003999301283129&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=8110561141098913096&ei=gqmuY-y0GY6yyAS9hoto&scisig=AAGBfm0FtwYgHVJONB2-q759cDMzYpdvOA Contraction of the pelvic floor muscles during abdominal maneuvers]. Archives of Physical Medicine and Rehabilitation. 2001; 82(8): 1081-8</ref><ref name="Neumann, Gill 2002">Neumann P, Gill V. [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s001920200027&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9756079865579858284&ei=n6muY-OmC4a8yATUzZGgCg&scisig=AAGBfm3dJojS0om3O3DITXPtoX4QiIh3yQ Pelvic floor and abdominal muscle interaction]: EMG activity and intra- abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002; 13: 125-32</ref> and practitioners should aim to achieve such a result in association with the lower abdominal drawing in manoeuvre. | |||
* Training should initially focus on quality of movement and precise isolation of the relevant core muscles which has been shown to be important in restoring normal motor control in people with LBD.<ref name="Tsao, Hodges 2007" /><ref name="Tsao et al 2010" /> | |||
* Once adequate motor control of the core muscles is achieved in non-weight bearing positions, subsequent progression to [[Back Pain Functional Scale|functional]] activities can be made.<ref name="Richardson et al 2004" /><ref name="Hides et al 2010" /> Importantly this progression involves integration of the global muscles of the spine with the core muscles during specific functional exercises as well as during strength training of the trunk.<ref name="Standaert et al 2008" /> | |||
* There is emerging evidence that functional retraining of normal [[Lumbosacral Biomechanics|lumbo-pelvic kinematics]] can improve motor control and clinical outcomes<ref name="Dankaerts et al 2010">Dankaerts W, O'Sullivan P. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X10001839 The validity of O'Sullivan's classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI):] Overview of a series of studies and review of the literature. Man Ther. 2010</ref> and these methods should also be considered during functional motor control exercises. | |||
== Assessment == | |||
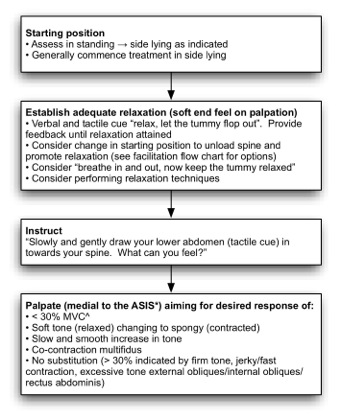
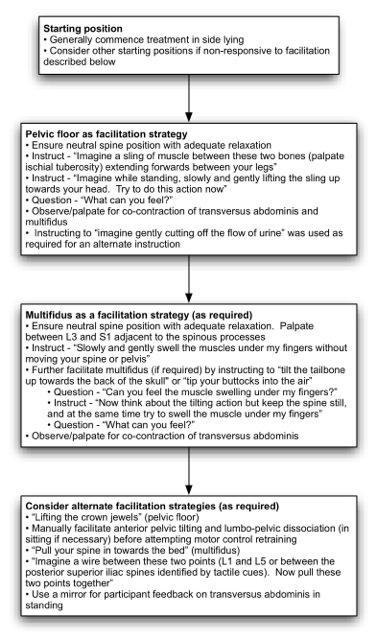
There is an overlap between assessment and treatment of motor control in the lumbar spine and these processes are summarised in Figure 5 below for non-weight bearing positions. | |||
There is an overlap between assessment and treatment of motor control in the lumbar spine and these processes are summarised in Figure | |||
[[Image:Figure 3.jpg]] | [[Image:Figure 3.jpg]] | ||
ASIS=anterior superior iliac spine<br>^MVC=maximal voluntary contraction | ASIS=[[Pelvic Landmarks|anterior superior iliac spine]]<br>^MVC=maximal voluntary contraction | ||
'''Figure 5: Initial non-weight bearing motor control training strategies'''<br><br>Adequate relaxation of the global muscles, eg [[Rectus Abdominis|rectus abdominis]], [[External Abdominal Oblique|external obliques]] and [[Erector_Spinae|erector spinae]], is required before attempting to contract the core stability muscles. Patients with maladaptive motor control strategies commonly demonstrate a dominance of the global muscles during functional tasks and at rest.<ref name="Hodges et al 2003" /><ref name="Hides et al 2009" /> In retraining a normal motor control pattern, adequate relaxation is an important first step in inhibiting tone of the global muscles, thereby allowing a more isolated contraction of the core muscles.<ref>Richardson C, Jull G, Hodges P. [https://scholar.google.com/scholar_url?url=http://125.212.201.8:6008/handle/DHKTYTHD_123/7945&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16674606697935355322&ei=86muY7KcH8SYywTZh5fgCg&scisig=AAGBfm0RxzM-OEOlI1b1jJbFc5OycyhLaQ Therapeutic exercise for lumbopelvic stabilisation:] a motor control approach for the treatment and prevention of low back pain. Edinburgh: Churchill Livingstone; 2004</ref> In attaining a relaxed state, a neutral spine position should also be encouraged, as this appears to improve activation of the core muscles.<ref name="Richardson et al 2004" /><ref name="O'Sullivan et al 2006">O'Sullivan P, Dankaerts W, Burnett A, Farrell G, Jefford E, Naylor C, et al. [https://scholar.google.com/scholar_url?url=https://journals.lww.com/spinejournal/FullText/2006/09010/Effect_of_Different_Upright_Sitting_Postures_on.24.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=5342507675684379242&ei=DqquY7ubCoa8yATUzZGgCg&scisig=AAGBfm3FfTDp-wy9I4EDN2cwtziP-HHG2Q Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population.] Spine. 2006; 31(19): E707-12</ref> | |||
# An instruction to “draw the lower abdomen in towards the spine” should be used, consistent with the developers of the abdominal drawing in method.<ref name="Richardson et al 2004" /> | |||
# In addition to these standard instructions, the terms “slowly” and “gently” can be added to emphasise a sub-maximal contraction.<ref name="Hides et al 2000">Hides J, Scott Q, Jull G, Richardson C. [https://scholar.google.com/scholar_url?url=https://journals.co.za/doi/abs/10.10520/EJC48442&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9265937931300231701&ei=J6quY9fnMY6yyAS9hoto&scisig=AAGBfm3TzNy7aqjRLkQIlZ9s8Spd1QrYcA A clinical palpation test to check the activation of the deep stabilizing muscles of the lumbar spine.] International SportMed Journal. 2000; 1(4)</ref> | |||
# Tactile cues to the lower abdomen should be used in conjunction with verbal cues to provide additional emphasis on a lower rather than more general drawing in of the abdomen.<ref name="Richardson et al 2004" /> | |||
# Non-weight bearing positions should be selected in the position where best activation of transversus abdominis is observed,<ref name="Richardson et al 2004" /><ref>Hides J, Stanton W, Wilson S, Freke M, McMahon S, Sims K. [https://scholar.google.com/scholar_url?url=https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0838.2009.01019.x&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=8142443811086389917&ei=RKquY7ekKtLAywSsrIVo&scisig=AAGBfm2Z5NHyt5otzNfpB_pI7DeILI7Y3w Retraining motor control of abdominal muscles among elite cricketers with low back pain]. Scandinavian Journal of Medicine & Science in Sports. 2010; 20(6): 834-42</ref> however side lying is commonly the optimal position for initial retraining<ref>Hides J, Stanton W, Wilson S, Freke M, McMahon S, Sims K. [https://scholar.google.com/scholar_url?url=https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0838.2009.01019.x&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=8142443811086389917&ei=YaquY_feI5CXywSwqaaIDw&scisig=AAGBfm2Z5NHyt5otzNfpB_pI7DeILI7Y3w Retraining motor control of abdominal muscles among elite cricketers with low back pain.] Scandinavian Journal of Medicine & Science in Sports. 2010; 20(6): 834-42</ref> due to ease of obtaining relaxation of the global muscles and an improved length tension relationship in [[Transversus Abdominis|transversus abdominis]] compared to other positions (eg supine or crook lying). | |||
Palpation | |||
< | * Primary outcomes indicative of an adequate and sub-maximal [[Transversus Abdominis|transversus abdominis]] contraction are a 2-3cm isolated inward movement of the abdomen approximately 3cm above the pubic symphysis and a palpable slow and co-ordinated change in tone from a “soft” feel in the relaxed state to a “spongy” feel at sub-maximal contraction.<ref name="Hides et al 2000" /> | ||
* These palpatory findings provide the physiotherapist with information additional to observation regarding the sub-maximal nature of the contraction.<ref name="Hides et al 2000" /> | |||
* The physiotherapist can concurrently palpate adjacent to the L3-L5 spinous processes to assess for co-contraction of lumbar multifidus, in the process identifying whether specific multifidus retraining is also required to achieve normal motor control. Well documented substitution strategies<ref name="Richardson et al 2004" /> should be monitored, and patient feedback provided, to ensure the observed drawing in of the lower abdomen and the palpatory findings are not the result of activity from the global muscles, in particular internal obliques. | |||
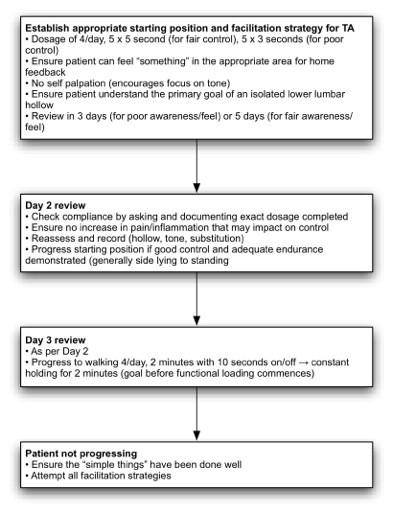
Patients commence motor control training in the position of highest functional demand where correct contraction of the core muscles can be achieved. This allows motor control training in a position specific to the patient’s capabilities and where improvement can be attained with between session practice. | |||
In the event of the patient not being able to engage transversus abdominis in any position with the processes described in Figure 3, a range of additional facilitation strategies can be attempted by the physiotherapist (Figure | * Side lying is generally recommended for patients where motor control is poor or inconsistent. | ||
* In the event of the patient not being able to engage [[Transversus Abdominis|transversus abdominis]] in any position with the processes described in Figure 3, a range of additional facilitation strategies can be attempted by the physiotherapist (Figure ). | |||
* These methods can also be used for patients who have good control of [[Transversus Abdominis|transversus abdominis]] but poor control of lumbar multifidus and/or poor awareness of pelvic floor activation.<br> | |||
[[Image:Figure 5.jpg]]<br> | [[Image:Figure 5.jpg]]<br> | ||
'''Figure | '''Figure 6: Activation and facilitation of transversus abdominis, lumbar multifidus and pelvic floor motor control''' | ||
In patients where transversus abdominis is difficult to isolate, activation was facilitated by an initial focus on the pelvic floor and/or lumbar multifidus.<ref name="Richardson et al 2004" /><ref name="Critchley 2002">Critchley D. [https://scholar.google.com/scholar_url?url=https://onlinelibrary.wiley.com/doi/abs/10.1002/pri.243&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=5297425251596789190&ei=i6quY_e8OpCXywSwqaaIDw&scisig=AAGBfm0vCaCvQT-esd7eA0lZ6zLrrhhoCw Instructing pelvic floor contraction facilitates transversus abdominis thickness increase during low-abdominal hollowing]. Physiother Res Int. 2002; 7(2): 65-75</ref> In such cases the strategies listed in Figure 6 are applied and co-contraction of transversus abdominis is concurrently monitored. In the event of co-contraction occurring, the patient should be encouraged to focus on awareness of simultaneous activation of transversus abdominis as well as the pelvic floor and/or lumbar multifidus. The pelvic floor instructions aim to illustrate the anatomy of the region and provide guidance in performing a submaximal isotonic contraction. The multifidus instructions aim to provide guidance in performing a submaximal isometric contraction. If necessary, multifidus can be facilitated by provision of kinaesthetic feedback to the patient with an initial isotonic contraction, followed by an attempt to transfer this awareness to the required isometric contraction. | |||
[[File:Abdominal curl-CDC strength training for older adults.gif|right|frameless]] | |||
During all motor control training the patient should be encouraged to develop a kinaesthetic awareness of the correct motor pattern. This is important in order for the patient to have some form of proprioceptive feedback regarding correct performance of the exercises when practising between sessions.<ref name="Richardson et al 2004" /> Subsequently during the treatment program, adequate kinaesthetic awareness of normal motor control is also required for transference into more functional and demanding exercises/activities. Due to the effect of even low force postural perturbation in initiating maladaptive motor patterns,<ref name="Hodges et al 1996" /><ref name="Hodges, Richardson 1998" /><ref name="MacDonald et al 2009" /> patients should be instructed not to self palpate as means of providing feedback on exercise performance until more consistent motor control skills are demonstrated. Self palpation can also focus the patient on tone rather than the primary goal of an isolated drawing in of the lower abdomen. | During all motor control training the patient should be encouraged to develop a kinaesthetic awareness of the correct motor pattern. This is important in order for the patient to have some form of proprioceptive feedback regarding correct performance of the exercises when practising between sessions.<ref name="Richardson et al 2004" /> Subsequently during the treatment program, adequate kinaesthetic awareness of normal motor control is also required for transference into more functional and demanding exercises/activities. Due to the effect of even low force postural perturbation in initiating maladaptive motor patterns,<ref name="Hodges et al 1996" /><ref name="Hodges, Richardson 1998" /><ref name="MacDonald et al 2009" /> patients should be instructed not to self palpate as means of providing feedback on exercise performance until more consistent motor control skills are demonstrated. Self palpation can also focus the patient on tone rather than the primary goal of an isolated drawing in of the lower abdomen. | ||
| Line 70: | Line 86: | ||
[[Image:Figure 6.jpg]]<br> | [[Image:Figure 6.jpg]]<br> | ||
'''Figure | '''Figure 7: Dosage and progression of motor control training<br>''' | ||
== | == Functional Activities == | ||
[[File:Lifting_light_weights_1.jpg|alt=|right|frameless]][[File:Lifting_light_weights_2.jpg|alt=|right|frameless]] | |||
Once adequate motor control has been demonstrated in walking, the patient should commence functional motor control training. In keeping with the principles of exercise prescription and rehabilitation, a graded exercise program based on the functional requirements of the patient’s own goals should be prescribed. Each exercise should be completed with tonic control of the core muscles in a correct motor control pattern. Key components of this program should include:<br>• Supervised functional exercise and motor control training at least weekly for at least 3 weeks in the clinic gym<br>• A focus on the quality of functional movement including facilitation of correct posture and lumbo-pelvic kinematics <br>• Concurrent between session functional exercise and motor control training at least 5 times a week for 15-45 minutes<br>• Patient documentation of exercise compliance using an exercise diary<br>• Regular patient/physiotherapist review of activity and exercise based goals with positive reinforcement of progress made<br>• A planned progression towards independence after completion of around 10 treatment sessions with the provision of a medium and long term exercise plan | Once adequate motor control has been demonstrated in walking, the patient should commence functional motor control training. In keeping with the principles of exercise prescription and rehabilitation, a graded exercise program based on the functional requirements of the patient’s own goals should be prescribed. Each exercise should be completed with tonic control of the core muscles in a correct motor control pattern. Key components of this program should include:<br>• Supervised functional exercise and motor control training at least weekly for at least 3 weeks in the clinic gym<br>• A focus on the quality of functional movement including facilitation of correct posture and lumbo-pelvic kinematics <br>• Concurrent between session functional exercise and motor control training at least 5 times a week for 15-45 minutes<br>• Patient documentation of exercise compliance using an exercise diary<br>• Regular patient/physiotherapist review of activity and exercise based goals with positive reinforcement of progress made<br>• A planned progression towards independence after completion of around 10 treatment sessions with the provision of a medium and long term exercise plan. | ||
'''Image 9 and 10 : An example of functional motor control''', biceps curls as a method of motor control training during low level manual handling of external resistance | |||
'''Lifting light weights''' will build up your core stability in preparation for heavier lifting, gardening and housework. Hold a dumbbell in each hand with your palm facing forward and arms straight. Without moving your upper arm, bend your left elbow and curl the dumbbell up toward the shoulder. Lower the left and curl the right arm. Perform the movement with good control of the trunk and arms. | '''Lifting light weights''' will build up your core stability in preparation for heavier lifting, gardening and housework. Hold a dumbbell in each hand with your palm facing forward and arms straight. Without moving your upper arm, bend your left elbow and curl the dumbbell up toward the shoulder. Lower the left and curl the right arm. Perform the movement with good control of the trunk and arms. | ||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 20:41, 20 January 2024
Original Editors - Jon Ford as part of the STOPS Project.
Top Contributors - Jon Ford, Lucinda hampton, Kim Jackson, Joris Servranckx, Sehriban Ozmen, Jonathan Wong, 127.0.0.1, Wendy Walker, Mariam Hashem, Chelsea Mclene, Carina Therese Magtibay and Rachael Lowe
Introduction[edit | edit source]
Motor control exercise is a popular form of exercise that aims to restore co-ordinated and efficient use of the muscles that control and support the spine. The therapist guides the client to practice normal use of the muscles during simple tasks. As control and skill improve, the exercises are progressed to more complex and functional tasks involving the muscles of the trunk and limbs[1].
During the 1990s and 2000s practitioners across the world began to recognise that the core muscles e.g. transversus abdominis, lumbar multifidus and the pelvic floor need assessment and consideration for inclusion in an integrated treatment program for low back pain[2]. A 2016 systematic review evaluating the effectiveness of motor control exercise (MCE) in patients with chronic non-specific low back pain concluded:
"MCE probably provides better improvements in pain, function and global impression of recovery than minimal intervention at all follow-up periods. MCE may provide slightly better improvements than exercise and electrophysical agents for pain, disability, global impression of recovery and the physical component of quality of life in the short and intermediate term. There is probably little or no difference between MCE and manual therapy for all outcomes and follow-up periods. Little or no difference is observed between MCE and other forms of exercise. Given the minimal evidence that MCE is superior to other forms of exercise, the choice of exercise for chronic LBP should probably depend on patient or therapist preferences, therapist training, costs and safety".[1]
Indeed, since 2016, most evidence is in agreement regarding the lack of difference in outcomes for chronic LBP between motor control exercises compared to other exercises[3].
Figure 1: Transversus abdominis
Figure 2: Lumbar multifidus on the left of the spine
Justification for Use[edit | edit source]
Specific motor control training as part of the treatment protocol was based on the principles developed by Richardson and colleagues.[4]Extensive research has been published on the importance of normal motor control in the lumbar spine including but not limited to:
• An anatomical and biomechanical suitability of the core muscles for providing stability to structures in the lumbar spine[5][6][7][8][9][10][11][12][13][14]
• Feedforward mechanisms in people without a low back disorder (LBD) resulting in “pre-setting” of the core muscles in anticipation of postural perturbation[15][16][17]
• Contraction of core muscles independent of direction of trunk forces and movements[18][19]
• Maladaptive differences between people with and without LBD in terms of altered feedforward mechanisms,[20][21][22][23]reduced core muscle cross sectional size,[24][25]increased global muscle activity in certain subgroups[26]and altered cortical representation of motor patterns[27]
This substantial literature has led to the hypothesis that correcting maladaptive motor control is an important component in the rehabilitation of LBD and prevention of recurrence.[28][29]
- This hypothesis is strengthened based on clinical data showing a reversal of the maladaptive changes observed in people with LBD[24][30][31][32][32][33] which is not achieved by less specific exercise such as abdominal bracing or general exercise.[34][35]
- In addition, RCTs have shown significant improvement for pain and activity in participants receiving specific motor control training compared to usual care[36][37][38][39] with larger effects demonstrable when homogenous subgroups are recruited.[40]
- Pain education coupled with cognition-targeted motor control training appears more effective than current best-evidence physiotherapy for improving pain in individuals with chronic LBP.[41]
- Recent controversy around specific motor control training[42][43]has been refuted based on an insufficient consideration of this expansive literature as a whole.[40]
- There is clear and extensive mechanistic and randomised controlled trial based data supporting the rationale for precise motor control training for LBD.
Clinical Application[edit | edit source]
Lumbar motor control training [4][44] has a large amount of variability in clinical application between physiotherapists.[45]and is commonly reported as a difficult concept to efficiently teach in people with LBD. [4][44] [37][46][47]
Now a series of clinical decision making algorithms (based on established protocols) has been developed and validated in a major clinical trial.[48][4][44]
Physiotherapy[edit | edit source]
The goal of the motor control program is to retrain the core muscles of the lumbar spine, comprising transversus abdominis, lumbar multifidus and the pelvic floor, to maintain a tonic and automatic contraction[22][49] at less than 30% of maximum voluntary contraction in daily activities[32][30].
Image 4: Correct and incorrect abdominal drawing in
- In most cases this requires initial training in non-weight bearing positions using a lower abdominal drawing in manoeuvre which has been shown to selectively activate transversus abdominis.[24] Lumbar multifidus and the pelvic floor muscles, including pubococcygeus, have been shown to co-contract with transversus abdominis to provide a “corset” for the lumbo-pelvic area[50][51] and practitioners should aim to achieve such a result in association with the lower abdominal drawing in manoeuvre.
- Training should initially focus on quality of movement and precise isolation of the relevant core muscles which has been shown to be important in restoring normal motor control in people with LBD.[30][32]
- Once adequate motor control of the core muscles is achieved in non-weight bearing positions, subsequent progression to functional activities can be made.[4][24] Importantly this progression involves integration of the global muscles of the spine with the core muscles during specific functional exercises as well as during strength training of the trunk.[37]
- There is emerging evidence that functional retraining of normal lumbo-pelvic kinematics can improve motor control and clinical outcomes[52] and these methods should also be considered during functional motor control exercises.
Assessment[edit | edit source]
There is an overlap between assessment and treatment of motor control in the lumbar spine and these processes are summarised in Figure 5 below for non-weight bearing positions.
ASIS=anterior superior iliac spine
^MVC=maximal voluntary contraction
Figure 5: Initial non-weight bearing motor control training strategies
Adequate relaxation of the global muscles, eg rectus abdominis, external obliques and erector spinae, is required before attempting to contract the core stability muscles. Patients with maladaptive motor control strategies commonly demonstrate a dominance of the global muscles during functional tasks and at rest.[14][49] In retraining a normal motor control pattern, adequate relaxation is an important first step in inhibiting tone of the global muscles, thereby allowing a more isolated contraction of the core muscles.[53] In attaining a relaxed state, a neutral spine position should also be encouraged, as this appears to improve activation of the core muscles.[4][54]
- An instruction to “draw the lower abdomen in towards the spine” should be used, consistent with the developers of the abdominal drawing in method.[4]
- In addition to these standard instructions, the terms “slowly” and “gently” can be added to emphasise a sub-maximal contraction.[55]
- Tactile cues to the lower abdomen should be used in conjunction with verbal cues to provide additional emphasis on a lower rather than more general drawing in of the abdomen.[4]
- Non-weight bearing positions should be selected in the position where best activation of transversus abdominis is observed,[4][56] however side lying is commonly the optimal position for initial retraining[57] due to ease of obtaining relaxation of the global muscles and an improved length tension relationship in transversus abdominis compared to other positions (eg supine or crook lying).
Palpation
- Primary outcomes indicative of an adequate and sub-maximal transversus abdominis contraction are a 2-3cm isolated inward movement of the abdomen approximately 3cm above the pubic symphysis and a palpable slow and co-ordinated change in tone from a “soft” feel in the relaxed state to a “spongy” feel at sub-maximal contraction.[55]
- These palpatory findings provide the physiotherapist with information additional to observation regarding the sub-maximal nature of the contraction.[55]
- The physiotherapist can concurrently palpate adjacent to the L3-L5 spinous processes to assess for co-contraction of lumbar multifidus, in the process identifying whether specific multifidus retraining is also required to achieve normal motor control. Well documented substitution strategies[4] should be monitored, and patient feedback provided, to ensure the observed drawing in of the lower abdomen and the palpatory findings are not the result of activity from the global muscles, in particular internal obliques.
Patients commence motor control training in the position of highest functional demand where correct contraction of the core muscles can be achieved. This allows motor control training in a position specific to the patient’s capabilities and where improvement can be attained with between session practice.
- Side lying is generally recommended for patients where motor control is poor or inconsistent.
- In the event of the patient not being able to engage transversus abdominis in any position with the processes described in Figure 3, a range of additional facilitation strategies can be attempted by the physiotherapist (Figure ).
- These methods can also be used for patients who have good control of transversus abdominis but poor control of lumbar multifidus and/or poor awareness of pelvic floor activation.
Figure 6: Activation and facilitation of transversus abdominis, lumbar multifidus and pelvic floor motor control
In patients where transversus abdominis is difficult to isolate, activation was facilitated by an initial focus on the pelvic floor and/or lumbar multifidus.[4][58] In such cases the strategies listed in Figure 6 are applied and co-contraction of transversus abdominis is concurrently monitored. In the event of co-contraction occurring, the patient should be encouraged to focus on awareness of simultaneous activation of transversus abdominis as well as the pelvic floor and/or lumbar multifidus. The pelvic floor instructions aim to illustrate the anatomy of the region and provide guidance in performing a submaximal isotonic contraction. The multifidus instructions aim to provide guidance in performing a submaximal isometric contraction. If necessary, multifidus can be facilitated by provision of kinaesthetic feedback to the patient with an initial isotonic contraction, followed by an attempt to transfer this awareness to the required isometric contraction.
During all motor control training the patient should be encouraged to develop a kinaesthetic awareness of the correct motor pattern. This is important in order for the patient to have some form of proprioceptive feedback regarding correct performance of the exercises when practising between sessions.[4] Subsequently during the treatment program, adequate kinaesthetic awareness of normal motor control is also required for transference into more functional and demanding exercises/activities. Due to the effect of even low force postural perturbation in initiating maladaptive motor patterns,[20][21][23] patients should be instructed not to self palpate as means of providing feedback on exercise performance until more consistent motor control skills are demonstrated. Self palpation can also focus the patient on tone rather than the primary goal of an isolated drawing in of the lower abdomen.
Once an appropriate motor control strategy, exercise and starting position has been identified, a detailed information sheet should be provided and explained to the patient. The content should include information on the anatomy and normal function of the core muscles, the general principle of progressing motor control training from non-weight bearing to functional activities, and instructions for between session practice. The physiotherapist should document an appropriate dosage regime on the information sheet according to the principles outlined in Figure 6. Over the following sessions the physiotherapist, working with the patient, should aim to achieve a tonic contraction of the core muscles, during walking for two minutes before progressing to more advanced functional training.
Figure 7: Dosage and progression of motor control training
Functional Activities[edit | edit source]
Once adequate motor control has been demonstrated in walking, the patient should commence functional motor control training. In keeping with the principles of exercise prescription and rehabilitation, a graded exercise program based on the functional requirements of the patient’s own goals should be prescribed. Each exercise should be completed with tonic control of the core muscles in a correct motor control pattern. Key components of this program should include:
• Supervised functional exercise and motor control training at least weekly for at least 3 weeks in the clinic gym
• A focus on the quality of functional movement including facilitation of correct posture and lumbo-pelvic kinematics
• Concurrent between session functional exercise and motor control training at least 5 times a week for 15-45 minutes
• Patient documentation of exercise compliance using an exercise diary
• Regular patient/physiotherapist review of activity and exercise based goals with positive reinforcement of progress made
• A planned progression towards independence after completion of around 10 treatment sessions with the provision of a medium and long term exercise plan.
Image 9 and 10 : An example of functional motor control, biceps curls as a method of motor control training during low level manual handling of external resistance
Lifting light weights will build up your core stability in preparation for heavier lifting, gardening and housework. Hold a dumbbell in each hand with your palm facing forward and arms straight. Without moving your upper arm, bend your left elbow and curl the dumbbell up toward the shoulder. Lower the left and curl the right arm. Perform the movement with good control of the trunk and arms.
References[edit | edit source]
- ↑ 1.0 1.1 Saragiotto BT, Maher CG, Yamato TP, Costa LO, Costa LC, Ostelo RW, Macedo LG. Motor control exercise for chronic non‐specific low‐back pain. Cochrane Database of Systematic Reviews. 2016(1). Available:https://www.cochrane.org/CD012004/BACK_motor-control-exercise-chronic-non-specific-low-back-pain (accessed 3.1.2022)
- ↑ Bystrom MG, Rasmussen-Barr E, Grooten WJ. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis. Spine (Phila Pa 1976). 2013; 38(6): E350-8
- ↑ Grooten WJA, Boström C, Dedering Åsa, Halvorsen M, Kuster RP, Nilsson-Wikmar L, et al. Summarizing the effects of different exercise types in chronic low back pain – a systematic review of systematic reviews. BMC musculoskeletal disorders. 2022;23(1):1–801.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Richardson C, Jull G, Hodges P. Therapeutic exercise for lumbopelvic stabilisation: a motor control approach for the treatment and prevention of low back pain. Edinburgh: Churchill Livingstone; 2004
- ↑ Barker P, Briggs, CA, Bogeski, G. Tensile transmission across the lumbar fasciae in embalmed cadavers: effects of tension to various muscular attachments. Spine. 2004; 29: 129-38
- ↑ Barker P, Guggenheimer, KT, Grkovic, I, Briggs, CA, Jones, DC, Thomas, CD, Hodges, PW. Effects of tensioning the lumbar fascia on segmental stiffness during flexion and extension. Spine. 2006; 31(4): 387-405
- ↑ Barker P, Briggs C. Attachments of the posterior layer of lumbar fascia. Spine. 1999; 24(17): 1757-64
- ↑ Panjabi M. The stabilizing system of the spine: Part I: Function, dysfucntion, adaptation and enhancement. Journal of Spinal Disorders. 1992; 5: 383-9
- ↑ Wilke H, Wolf S, Claes L, Arand M, Wiesend A. Stability increase on the lumbar spine with different muscle groups. Spine. 1995; 20(2): 192-8
- ↑ MacIntosh J, Bogduk N. The biomechanics of the lumbar multifidus. Clinical biomechanics. 1986; 1: 205-13
- ↑ Kaigle A, Holm S, Mansson T. Experimental instability in the lumbar spine. Spine. 1995; 20(4): 421-30
- ↑ Hodges P, Eriksson M, Shirley D, Gandevia S. Intra-abdominal pressure increases stiffness of the lumbar spine. Journal of Biomechanics. 2005; 38(9): 1873-80
- ↑ Hodges P, Cresswell, AG, Daggfeldt, K, Thorstensson, A. In vivo measurements of the effect of intra-abdominal pressure on the human spine. Journal of Biomechanics. 2001; 34(347-353)
- ↑ 14.0 14.1 Hodges P, Kaigle, HA, Holm, S, Ekström, L, Cresswell, A, Hansson, T, Thorstensson, A. . Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine. 2003; 28(23): 2594-601
- ↑ Cresswell A, Oddsson, L, Thorstensson, A. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Exp Brain res. 1994; 98: 336-41
- ↑ Hodges P, Richardson C. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp Brain Res. 1997; 114: 362-70
- ↑ Hodges P, Richardson C. Contraction of the abdominal muscles associated with movement of the lower limb. Physical Therapy. 1997; 77(2): 132-44
- ↑ Cresswell A, Grundstrom H, Thorstensson A. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiology Scandinavia. 1992
- ↑ Hodges P, Cresswell, A & Thorstensson, A. Preparatory trunk motion accompanies rapid upper limb movement. Exp Brain Res. 1999; 124: 69-79
- ↑ 20.0 20.1 Hodges P, Richardson C. Inefficient muscular stabilisation of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine. 1996; 21: 2640-50
- ↑ 21.0 21.1 Hodges P, Richardson, CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. Journal of Spinal Disorders. 1998; 11(1): 46-56
- ↑ 22.0 22.1 Ferreira P, Ferreira M, Hodges P. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine. 2004; 29(22): 2560-6
- ↑ 23.0 23.1 MacDonald D, Moseley G, Hodges P. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain. 2009; 142(3): 183-8
- ↑ 24.0 24.1 24.2 24.3 Hides J, Lambrecht G, Richardson C, Stanton W, Armbrecht G, Pruett C, et al. The effects of rehabilitation on the muscles of the trunk following prolonged bed rest. European Spine Journal. 2010
- ↑ Dickx N, Cagnie B, Parlevliet T, Lavens A, Danneels L. The effect of unilateral muscle pain on recruitment of the lumbar multifidus during automatic contraction. An experimental pain study. Manual Therapy. 2010; 15(4): 364-9
- ↑ Dankaerts W, O'Sullivan P, Burnett A, Straker L. Altered patterns of superficial trunk muscle activation during sitting in nonspecific chronic low back pain patients: importance of subclassification. Spine. 2006; 31(17): 2017-23
- ↑ Tsao H, Galea M, Hodges P. Reorganization of the motor cortex is associated with postural control deficits in recurrent low back pain. Brain. 2008; 131(8): 2161-71
- ↑ Hodges P, Moseley G. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. Journal of Electromyography and Kinesiology. 2003; 13(4): 361-70
- ↑ Richardson C, Hides J, Wilson S, Stanton W, Snijders C. Lumbo-pelvic joint protection against antigravity forces: motor control and segmental stiffness assessed with magnetic resonance imaging. J Gravit Physiol. 2004; 11(2): P119-22.
- ↑ 30.0 30.1 30.2 Tsao H, Hodges P. Immediate changes in feedforward postural adjustments following voluntary motor training. Experimental Brain Research. 2007; 181(4): 537-46
- ↑ Tsao H, Hodges P. Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. Journal of Electromyography and Kinesiology. 2008; 18(4): 559-67
- ↑ 32.0 32.1 32.2 32.3 Tsao H, Druitt T, Schollum T, Hodges P. Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. The Journal of Pain. 2010; 11(11): 1120-8
- ↑ Vasseljen O, Fladmark A. Abdominal muscle contraction thickness and function after specific and general exercises: a randomized controlled trial in chronic low back pain patients. Man Ther. 2010; 15(5): 482-9
- ↑ Ferreira P, Ferreira M, Maher C, Refshauge K, Herbert R, Hodges P. Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. British Journal of Sports Medicine. 2009; 44(16): 1166-72
- ↑ Hall L, Tsao H, MacDonald D, Coppieters M, Hodges P. Immediate effects of co-contraction training on motor control of the trunk muscles in people with recurrent low back pain. Journal of electromyography and kinesiology: official journal of the International Society of Electrophysiological Kinesiology. 2009; 19(5): 763
- ↑ Ferreira P, Ferreira M, Maher C, Herbert R, Refshauge K. Specific stabilisation exercise for spinal and pelvic pain: a systematic review. Australian Journal of Physiotherapy. 2006; 52(2): 79-88
- ↑ 37.0 37.1 37.2 Standaert C, Weinstein S, Rumpeltes J. Evidence-informed management of chronic low back pain with lumbar stabilization exercises. The Spine Journal. 2008; 8(1): 114-20
- ↑ Rackwitz B, de Bie R, Limm H, von Garnier K, Ewert T, Stucki G. Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials. Clin Rehabil. 2006; 20(7): 553-67
- ↑ Macedo L, Maher C, Latimer J, McAuley J. Motor control exercise for persistent, nonspecific low back pain: a systematic review. Physical Therapy. 2009; 89(1): 9-25
- ↑ 40.0 40.1 Hodges P. Transversus abdominis: a different view of the elephant. British Journal of Sports Medicine. 2008; 42(12): 941-4
- ↑ Malfliet A, Kregel J, Coppieters I, De Pauw R, Meeus M, Roussel N, et al. Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA neurology. 2018;75(7):808–17.
- ↑ Allison G, Morris S. Transversus abdominis and core stability: has the pendulum swung? British Journal of Sports Medicine. 2008; 42(11): 630-1
- ↑ McGill SM. Low back disorders: Evidence-based prevention and rehabilitation 2nd ed. Illinois: Human Kinetics Publishers; 2008
- ↑ 44.0 44.1 44.2 O'Sullivan P. Lumbar segmental 'instability': clinical presentation and specific stabilizing exercise management. Manual Therapy. 2000; 5(1): 2-12
- ↑ Ford J, Hahne A, Chan A, Surkitt L. A classification and treatment protocol for low back disorders. Part 3: functional restoration for intervertebral disc related disorders. Physical Therapy Reviews. 2012; 17(1): 55-75
- ↑ Henry S, Westervelt K. The use of real-time ultrasound feedback in teaching abdominal hollowing exercises to healthy subjects. Journal of Orthopaedic & Sports Physical Therapy. 2005; 35(6): 338-45
- ↑ Hides J, Stanton W, Freke M, Wilson S, McMahon S, Richardson C. MRI study of the size, symmetry and function of the trunk muscles among elite cricketers with and without low back pain. Br J Sports Med. 2008; 42(10): 809-13
- ↑ Hahne AJ, Ford JJ, Surkitt LD, Richards MC, Chan AY, Thompson SL, et al. Specific treatment of problems of the spine (STOPS): design of a randomised controlled trial comparing specific physiotherapy versus advice for people with subacute low back disorders. BMC Musculoskeletal Disorders. 2011; 12: 104
- ↑ 49.0 49.1 Hides J, Belavy D, Cassar L, Williams M, Wilson S, Richardson C. Altered response of the anterolateral abdominal muscles to simulated weight-bearing in subjects with low back pain. Eur Spine J. 2009; 18(3): 410-8
- ↑ Sapsford R. Contraction of the pelvic floor muscles during abdominal maneuvers. Archives of Physical Medicine and Rehabilitation. 2001; 82(8): 1081-8
- ↑ Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra- abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002; 13: 125-32
- ↑ Dankaerts W, O'Sullivan P. The validity of O'Sullivan's classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI): Overview of a series of studies and review of the literature. Man Ther. 2010
- ↑ Richardson C, Jull G, Hodges P. Therapeutic exercise for lumbopelvic stabilisation: a motor control approach for the treatment and prevention of low back pain. Edinburgh: Churchill Livingstone; 2004
- ↑ O'Sullivan P, Dankaerts W, Burnett A, Farrell G, Jefford E, Naylor C, et al. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine. 2006; 31(19): E707-12
- ↑ 55.0 55.1 55.2 Hides J, Scott Q, Jull G, Richardson C. A clinical palpation test to check the activation of the deep stabilizing muscles of the lumbar spine. International SportMed Journal. 2000; 1(4)
- ↑ Hides J, Stanton W, Wilson S, Freke M, McMahon S, Sims K. Retraining motor control of abdominal muscles among elite cricketers with low back pain. Scandinavian Journal of Medicine & Science in Sports. 2010; 20(6): 834-42
- ↑ Hides J, Stanton W, Wilson S, Freke M, McMahon S, Sims K. Retraining motor control of abdominal muscles among elite cricketers with low back pain. Scandinavian Journal of Medicine & Science in Sports. 2010; 20(6): 834-42
- ↑ Critchley D. Instructing pelvic floor contraction facilitates transversus abdominis thickness increase during low-abdominal hollowing. Physiother Res Int. 2002; 7(2): 65-75