Legionnaire's Disease: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (48 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- Itayi Charasika [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] <br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | |||
'''Original | |||
==Definition/Description== | |||
= | |||
Legionnaires' Disease is a severe form of [[pneumonia]] (lung infection) caused by a bacteria, known as ''Legionella''. It can occur through inhalation of contaminated aerosols such as humidifiers, hot and cold water systems, air conditioning cooling towers and whirlpool spas. Infection can also occur by exposure of babies during water births or aspiration of contaminated ice or water, particularly in susceptible hospital patients. It can be a cause of community acquired pneumonia or [[Hospital Acquired Pneumonia|hospital acquired pneumonia]]<ref>Pedro-Botet M. L., Sabria-Leal M., Haro M., Rubio C., Gimenez G., Sopena N., Tor J.Nosocomial and community-acquired Legionella pneumonia: clinical comparative analysis. ''Eur. Respir. J.''8199519291933 retrieved from https://erj.ersjournals.com/content/8/11/1929.short</ref>. This disease is often screened for whenever a person is diagnosed with pneumonia because of the close resemblance Legionnaires' has to pneumonia. | |||
<br>The bacteria, ''Legionella'', in | <br>The bacteria, ''Legionella'', in Legionnaires' disease can also cause a milder illness called Pontiac Fever. Pontiac Fever resembles a mild and self-resolving flu-like disease.<ref name=":0">Sharma L, Losier A, Tolbert T, Dela Cruz CS, Marion CR. Atypical Pneumonia: Updates on Legionella, Chlamydophila, and Mycoplasma Pneumonia. ''Clin Chest Med''. 2017;38(1):45–58. doi:10.1016/j.ccm.2016.11.011 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5679202/</ref> Unlike Legionnaires' disease, Pontiac Fever usually resolves on its own after 2-5 days.<ref name=":0" />If diagnosed with both illnesses, then the term is Legionellosis. | ||
==History of Disease== | |||
Legionnaires' disease was first discovered about in 1967 when a group of people in Philadelphia, attending an American Legion convention meeting were exposed to this disease. Those affected suffered from a type of pneumonia, now referred to as Legionnaires’ disease. | |||
The first identified cases of Pontiac fever occurred in 1968 in Pontiac, Michigan, among people who worked at and visited the city’s health department. It wasn’t until ''Legionella'' was discovered after the 1976 Legionnaires’ disease outbreak in Philadelphia that public health officials were able to show that ''Legionella'' causes both diseases. | |||
[[Image:Lunganatomy.jpg|frame|Legionnaire's Disease]] | |||
[[Image:Ld image.jpg|Image:Ld_image.jpg]] | |||
<br> | |||
== Etiology == | |||
The pathogen causing Legionnaires' Disease came from the ''Legionellaceae'' family of bacteria. Although the family ''Legionellaceae'' now contains more than 40 species, ''L. pneumophila'' causes over 90% of human infections. ''L micdadei'', the second most frequently isolated species in human infection, evidently has lower virulence for humans than ''L. pneumophila'' as it appears to infect only immunocompromised hosts.<ref>Myerowitz RL, Pasculle AW, Dowling JN et al. (1971) Opportunistic lung infection due to “Pittsburgh Pneumonia Agent”. N Engl J Med 301: 953–958.</ref> Water is the major natural reservoir for ''Legionella'', and the pathogen is found in many different natural and artificial aquatic environments such as cooling towers or water systems in buildings, including hospitals.<ref>Cunha BA, Burillo A, Bouza E, Legionnaires' disease, The Lancet, Volume 387, Issue 10016, 2016, Pages 376-385, ISSN 0140-6736, <nowiki>https://doi.org/10.1016/S0140-6736(15)60078-2</nowiki> retrieved from https://www.sciencedirect.com/science/article/pii/S0140673615600782</ref> | |||
| Common places that allow Legionella transmission:<br>1. Potable (drinking) water systems<br>2. Whirlpool spas<br>3. Cooling towers | ||
[[Image:Images7.jpg]] <br>Conditions for Legionella transmission:<br>1. Heat<br>2. Stasis<br>3. Aerosolization | |||
== Prevalence== | |||
Accurate data reflecting the true incidence of disease are not available because of underutilization of diagnostic testing and under-reporting.<ref>Plouffe JF, Breiman RF, Fields BS, Herbert M, Inverso J, Knirsch C, Kolokathis A, Marrie TJ, Nicolle L, Schwartz DB, Azithromycin in the Treatment of ''Legionella'' Pneumonia Requiring Hospitalization, ''Clinical Infectious Diseases'', Volume 37, Issue 11, December 2003, Pages 1475–1480, <nowiki>https://doi.org/10.1086/379329</nowiki> retrieved from https://academic.oup.com/cid/article/37/11/1475/372119</ref> It is a common cause of severe pneumonia requiring hospitalization.<br> | |||
'''Facts''': | |||
| *Responsible for ~ 5% of all pneumonias | ||
*12,000 people affected yearly in the U.S | |||
*Each year an estimated 8,000-18,000 hospitalized cases occur in the U.S.<ref name=":1">Legionnaires' Disease available at https://emedicine.medscape.com/article/220163-overview</ref> | |||
*The majority of reported cases are sporadic but 10-20% of them are linked to outbreaks<ref name=":1" /> | |||
*Travel-associated outbreaks, outbreaks in community settings, and nosocomial and occupational outbreaks are common | |||
*More than 20% of all cases are thought to be associated with recent travel | |||
*Difficult to detect among travelers because of the low attack rate, long incubation period, and the dispersal of persons from the source of the outbreak | |||
*Present rate is that 80% of those contracting the disease die | |||
*In 2011 California health officials reported Legionnaires disease as a potential diagnosis during a investigation of a mystery illness at the Playboy mansion possibly caused by a fog machine where a 100 people developed respiratory infections. [http://www.youtube.com/watch?v=xk5dEOYtPbw&feature=fvsr http://www.youtube.com/watch?v=xk5dEOYtPbw&feature=fvsr]. | |||
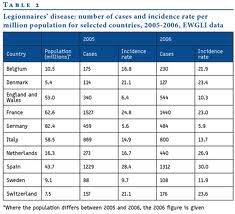
'''Legionnaire's Disease is found worldwide as illustrated below'''. | |||
[[Image:World images.jpg|Image:World_images.jpg]] [[Image:Images3.jpg]] | |||
| |||
== Associated Comorbidities == | |||
People at risk: | |||
*Smokers ( | *Smokers (current and former) | ||
*Chronic lung disease | *Chronic lung disease | ||
* | *Advanced age (50 years and above) | ||
*Alcohol abuse | *Alcohol abuse | ||
*Surgery | *Surgery | ||
| Line 68: | Line 62: | ||
*Recent repairs or maintenance work on domestic plumb | *Recent repairs or maintenance work on domestic plumb | ||
*Immune system compromised by | *Immune system compromised by | ||
**DM | |||
**Renal Failure | |||
**Cancer (esp. hematological or pulmonary malignancy) | |||
**AIDS | |||
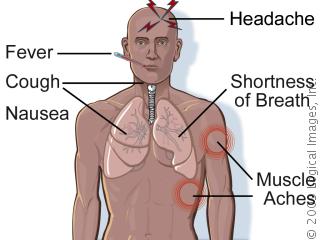
==Characteristics/Clinical Presentation== | |||
'''Signs & Symptoms''': | |||
== ''' | |||
* Fever | |||
* Dry or productive cough, | |||
* Fatigue | |||
* Anorexia | |||
* Headache | |||
* Myalgia | |||
* Diarrhea | |||
* Gastrointestinal symptoms | |||
[[Image:Images4.jpg]] | |||
=== Systemic Involvement === | |||
*Gastrointestinal symptoms include nausea, vomiting, diarrhea, and anorexia. | |||
*Neurologic symptoms include headache, lethargy, altered mental status, and rarely, focal symptoms. | |||
*Musculoskeletal symptoms include arthralgias and myalgias. | |||
*Nonpulmonary symptoms are prominent early in the disease.<br> | |||
== | ==Diagnostic Tests/Laboratory Findings:== | ||
Legionnaire’s disease is diagnosed by growing bacteria on a special medium and silver staining. The bacteria is identified in the sputum and the Legionella antigen is seen in the urine | Legionnaire’s disease is diagnosed by growing bacteria on a special medium and silver staining. The bacteria is identified in the sputum and the ''Legionella'' antigen is seen in the urine. | ||
[[Image:Images6.jpg]] [[Image:Images8.jpg]]<br>What diagnostic tests can confirm Legionnaires' disease? | [[Image:Images6.jpg]] [[Image:Images8.jpg]]<br>What diagnostic tests can confirm Legionnaires' disease?<ref name=":2">Legionnaires Disease- CDC available at https://www.cdc.gov/legionella/index.html</ref><br> | ||
{| style="width: 639px; height: 366px" border="2" cellspacing="1" cellpadding="1" width="639" | {| style="width: 639px; height: 366px" border="2" cellspacing="1" cellpadding="1" width="639" | ||
|+ ''' | |+'''Diagnostic Tests''' | ||
{| style="width: 309px; height: 149px" border="3" cellspacing="1" cellpadding="1" width="309" | |||
|+'''Tests In Relationship to Snout/Spin''' | |||
|- | |||
|'''Test''' | |||
|'''Sensitivity (%)''' | |||
|'''Specificity (%)''' | |||
|- | |||
|'''Culture''' | |||
| 80 | |||
| 100 | |||
|- | |||
|'''Urine antigen''' | |||
| 70 | |||
| 100 | |||
|- | |||
|'''Paired serology*''' | |||
| 70-80 | |||
|>90 | |||
|- | |||
|'''[http://www.nlm.nih.gov/medlineplus/ency/article/003553.htm Direct fluorescent antibody stain]''' | |||
| 25-75% | |||
| 95 | |||
|- | |||
| *''Note: A single antibody titer of any level is not diagnostic of legionellosis'' | |||
| | |||
| | |||
|} | |||
|- | |- | ||
| | | | ||
| Line 102: | Line 135: | ||
|- | |- | ||
| '''Culture''' | |'''Culture''' | ||
| - Clinical & Environmental isolates can be compared<br>- Detects all species & serogroups<br>- 100% specific<br> | | - Clinical & Environmental isolates can be compared<br>- Detects all species & serogroups<br>- 100% specific<br> | ||
| - Technically difficult<br>- Slow (>5 days to grow)<br>- Sensitivity highly dependent on technical skill<br>- May be affected by antibiotic treatment <br> | | - Technically difficult<br>- Slow (>5 days to grow)<br>- Sensitivity highly dependent on technical skill<br>- May be affected by antibiotic treatment <br> | ||
|- | |- | ||
| '''Urine Antigen''' | |'''Urine Antigen''' | ||
| - >99% specific...<br>- Rapid (same day)<br> | | - >99% specific...<br>- Rapid (same day)<br> | ||
| - ...but only for L. pneumophila serogroup 1 (Lp1) [ which may account for up to 80% of cases]<br>- Limited utility when compared to environmental isolates<br> | | - ...but only for L. pneumophila serogroup 1 (Lp1) [ which may account for up to 80% of cases]<br>- Limited utility when compared to environmental isolates<br> | ||
|- | |- | ||
| '''Serology''' | |'''Serology''' | ||
| - Not affected by antibiotic treatment<br>- 70-80% sensitive; >90% specific<br> | | - Not affected by antibiotic treatment<br>- 70-80% sensitive; >90% specific<br> | ||
| - Must have paired sera<br>- 5-10% of population has titer 1:≥256<br>Single acute phase antibody titers of 1:≥256 do not discriminate between cases of Legionnaires' disease and other causes of community-acquired pneumonia. <br> | | - Must have paired sera<br>- 5-10% of population has titer 1:≥256<br>Single acute phase antibody titers of 1:≥256 do not discriminate between cases of Legionnaires' disease and other causes of community-acquired pneumonia. <br> | ||
|- | |- | ||
| | | DFA | ||
| - Can be performed on pathologic specimens<br>- 95% specific<br> | | - Can be performed on pathologic specimens<br>- 95% specific<br> | ||
| - 25-75% sensitive | | - 25-75% sensitive | ||
|} | |} | ||
== | ===== Legionnaires Disease VS Pontiac Fever ===== | ||
= | |||
== | |||
{| style="width: 714px; height: 260px" border="3" cellspacing="1" cellpadding="1" width="714" | {| style="width: 714px; height: 260px" border="3" cellspacing="1" cellpadding="1" width="714" | ||
|+ '''Legionnaire's Disease vs. Pontiac Fever''' | |+ '''Legionnaire's Disease vs. Pontiac Fever''' | ||
| Line 195: | Line 193: | ||
|} | |} | ||
* Percent of persons who, when exposed to the source of an outbreak, become ill. <br>** Percent of persons who die from Legionnaires' disease or Pontiac fever. | |||
==Medical Management== | |||
== Medications == | |||
*Erythromycin (the drug of choice for prolonged period) - given early | |||
*Rifampin is also a benefit | |||
< | <br>Newer Effective Therapeutic Options Include Antibiotics (Macrolides):<br> | ||
* Clarithromycin | |||
*Azithromycin | |||
* Fluoroquinolones | |||
Patients diagnosed with Legionnaire's Disease are prescribed to take the various medications. | |||
For patients with Pontiac fever: it is a self-limited illness that does not benefit from antibiotic treatment. Complete recovery usually occurs within 1 week. | |||
== | ==Physical Therapy Management== | ||
*Screening Questions: | |||
- Have you traveled recently? (Patient could have traveled-associated Legionnaire’s disease<ref name=":2" /> | |||
* Patient Care: Respiratory Therapists/PTs: O<sub>2</sub> therapy, repositioning, postural drainage, suctioning | |||
* Monitor: Chest wall expansion, depth/pattern of ventilations, cough, chest pain, restlessness, & hypoxemia | |||
* Signs of Shock: ↓ blood pressure, tachycardia w/weak thread pulse, diaphoresis, clamy skin, & cold | |||
* Patient Education: Pulmonary hygiene, deep breathing and coughing exercises, chest physiotherapy, postural drainage, disposal of solid tissues to prevent disease transmission<sup><br></sup><br> | |||
==Differential Diagnosis== | |||
== | |||
*Adult Respiratory Distress Syndrome (ARDS) | *Adult Respiratory Distress Syndrome (ARDS) | ||
| Line 263: | Line 239: | ||
*Tuberculosis | *Tuberculosis | ||
== | ==Case Reports/ Case Studies== | ||
• | •[https://newyorkmedicaljournal.org/articles/atypical-presentation-of-legionnaires-disease/ Atypical Presentation of Legionnaire’s Disease: A Case Report and Review] <br>•[https://casesjournal.biomedcentral.com/articles/10.1186/1757-1626-2-9151 Severe Legionnaires disease complicated by multi-organ dysfunction in a previously healthy patient: a case report]<br>•[http://ajcc.aacnjournals.org/content/12/3/234.full Legionnaires Disease: A Case Study] | ||
==Resources == | |||
* [https://www.cdc.gov/legionella/index.html Legionella(Legionnaire' Disease and Pontiac Fever)- Centers for Disease Control and Prevention] | |||
* [http://legionella.org/ Legionella.org] | |||
* [https://thesureword.org/wp-content/uploads/2016/11/The-Natural-Remedies-Encyclopedia.pdf Natural Remedies Encyclopedia] | |||
* [https://www.who.int/news-room/fact-sheets/detail/legionellosis Legionellosis- WHO]<br> | |||
< | ==References== | ||
<references /> | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Respiratory Disease - Conditions]] | |||
[[Category:Respiratory]] | |||
[[Category:Respiratory Disease]] | |||
[[ | [[Category:Communicable Diseases]] | ||
Latest revision as of 16:21, 3 March 2023
Top Contributors - Itayi Charasika, Donald John Auson, Kim Jackson, Kalyani Yajnanarayan, Admin, Elaine Lonnemann, WikiSysop, Adam Vallely Farrell and Nupur Smit Shah
Definition/Description[edit | edit source]
Legionnaires' Disease is a severe form of pneumonia (lung infection) caused by a bacteria, known as Legionella. It can occur through inhalation of contaminated aerosols such as humidifiers, hot and cold water systems, air conditioning cooling towers and whirlpool spas. Infection can also occur by exposure of babies during water births or aspiration of contaminated ice or water, particularly in susceptible hospital patients. It can be a cause of community acquired pneumonia or hospital acquired pneumonia[1]. This disease is often screened for whenever a person is diagnosed with pneumonia because of the close resemblance Legionnaires' has to pneumonia.
The bacteria, Legionella, in Legionnaires' disease can also cause a milder illness called Pontiac Fever. Pontiac Fever resembles a mild and self-resolving flu-like disease.[2] Unlike Legionnaires' disease, Pontiac Fever usually resolves on its own after 2-5 days.[2]If diagnosed with both illnesses, then the term is Legionellosis.
History of Disease[edit | edit source]
Legionnaires' disease was first discovered about in 1967 when a group of people in Philadelphia, attending an American Legion convention meeting were exposed to this disease. Those affected suffered from a type of pneumonia, now referred to as Legionnaires’ disease.
The first identified cases of Pontiac fever occurred in 1968 in Pontiac, Michigan, among people who worked at and visited the city’s health department. It wasn’t until Legionella was discovered after the 1976 Legionnaires’ disease outbreak in Philadelphia that public health officials were able to show that Legionella causes both diseases.
Etiology[edit | edit source]
The pathogen causing Legionnaires' Disease came from the Legionellaceae family of bacteria. Although the family Legionellaceae now contains more than 40 species, L. pneumophila causes over 90% of human infections. L micdadei, the second most frequently isolated species in human infection, evidently has lower virulence for humans than L. pneumophila as it appears to infect only immunocompromised hosts.[3] Water is the major natural reservoir for Legionella, and the pathogen is found in many different natural and artificial aquatic environments such as cooling towers or water systems in buildings, including hospitals.[4]
Common places that allow Legionella transmission:
1. Potable (drinking) water systems
2. Whirlpool spas
3. Cooling towers

Conditions for Legionella transmission:
1. Heat
2. Stasis
3. Aerosolization
Prevalence[edit | edit source]
Accurate data reflecting the true incidence of disease are not available because of underutilization of diagnostic testing and under-reporting.[5] It is a common cause of severe pneumonia requiring hospitalization.
Facts:
- Responsible for ~ 5% of all pneumonias
- 12,000 people affected yearly in the U.S
- Each year an estimated 8,000-18,000 hospitalized cases occur in the U.S.[6]
- The majority of reported cases are sporadic but 10-20% of them are linked to outbreaks[6]
- Travel-associated outbreaks, outbreaks in community settings, and nosocomial and occupational outbreaks are common
- More than 20% of all cases are thought to be associated with recent travel
- Difficult to detect among travelers because of the low attack rate, long incubation period, and the dispersal of persons from the source of the outbreak
- Present rate is that 80% of those contracting the disease die
- In 2011 California health officials reported Legionnaires disease as a potential diagnosis during a investigation of a mystery illness at the Playboy mansion possibly caused by a fog machine where a 100 people developed respiratory infections. http://www.youtube.com/watch?v=xk5dEOYtPbw&feature=fvsr.
Legionnaire's Disease is found worldwide as illustrated below.
Associated Comorbidities[edit | edit source]
People at risk:
- Smokers (current and former)
- Chronic lung disease
- Advanced age (50 years and above)
- Alcohol abuse
- Surgery
- Recent travel with an overnight stay outside of the home
- Exposure to whirlpool spas
- Recent repairs or maintenance work on domestic plumb
- Immune system compromised by
- DM
- Renal Failure
- Cancer (esp. hematological or pulmonary malignancy)
- AIDS
Characteristics/Clinical Presentation[edit | edit source]
Signs & Symptoms:
- Fever
- Dry or productive cough,
- Fatigue
- Anorexia
- Headache
- Myalgia
- Diarrhea
- Gastrointestinal symptoms
Systemic Involvement[edit | edit source]
- Gastrointestinal symptoms include nausea, vomiting, diarrhea, and anorexia.
- Neurologic symptoms include headache, lethargy, altered mental status, and rarely, focal symptoms.
- Musculoskeletal symptoms include arthralgias and myalgias.
- Nonpulmonary symptoms are prominent early in the disease.
Diagnostic Tests/Laboratory Findings:[edit | edit source]
Legionnaire’s disease is diagnosed by growing bacteria on a special medium and silver staining. The bacteria is identified in the sputum and the Legionella antigen is seen in the urine.

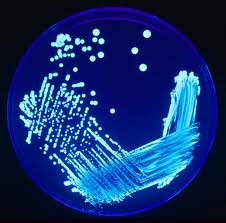
What diagnostic tests can confirm Legionnaires' disease?[7]
| Test | Sensitivity (%) | Specificity (%) |
| Culture | 80 | 100 |
| Urine antigen | 70 | 100 |
| Paired serology* | 70-80 | >90 |
| Direct fluorescent antibody stain | 25-75% | 95 |
| *Note: A single antibody titer of any level is not diagnostic of legionellosis |
Test
Advantages
Disadvantages
- Detects all species & serogroups
- 100% specific
- Slow (>5 days to grow)
- Sensitivity highly dependent on technical skill
- May be affected by antibiotic treatment
- Rapid (same day)
- Limited utility when compared to environmental isolates
- 70-80% sensitive; >90% specific
- 5-10% of population has titer 1:≥256
Single acute phase antibody titers of 1:≥256 do not discriminate between cases of Legionnaires' disease and other causes of community-acquired pneumonia.
- 95% specific
Legionnaires Disease VS Pontiac Fever[edit | edit source]
| Legionnaires' disease | Pontiac fever | |
| Clinical Features | Pneumonia: cough, fever, chest pain | Flu-like illness (fever, chills, malaise) without pneumonia |
| Radiographic pneumonia | Yes | No |
| Incubation period | 2-14 days after exposure | 24-48 hours after exposure |
| Etiologic agent | Legionella species | Legionella species |
| Attack rate* | < 5% | > 90% |
| Isolation of organism | Possible | Virtually never |
| Outcome | Hospitalization common Case-fatality rate: 5-40%** |
Hospitalization uncommon Case-fatality rate: 0% |
| Additional Below* |
* Percent of persons who, when exposed to the source of an outbreak, become ill.
** Percent of persons who die from Legionnaires' disease or Pontiac fever.
Medical Management[edit | edit source]
Medications[edit | edit source]
- Erythromycin (the drug of choice for prolonged period) - given early
- Rifampin is also a benefit
Newer Effective Therapeutic Options Include Antibiotics (Macrolides):
- Clarithromycin
- Azithromycin
- Fluoroquinolones
Patients diagnosed with Legionnaire's Disease are prescribed to take the various medications.
For patients with Pontiac fever: it is a self-limited illness that does not benefit from antibiotic treatment. Complete recovery usually occurs within 1 week.
Physical Therapy Management[edit | edit source]
- Screening Questions:
- Have you traveled recently? (Patient could have traveled-associated Legionnaire’s disease[7]
- Patient Care: Respiratory Therapists/PTs: O2 therapy, repositioning, postural drainage, suctioning
- Monitor: Chest wall expansion, depth/pattern of ventilations, cough, chest pain, restlessness, & hypoxemia
- Signs of Shock: ↓ blood pressure, tachycardia w/weak thread pulse, diaphoresis, clamy skin, & cold
- Patient Education: Pulmonary hygiene, deep breathing and coughing exercises, chest physiotherapy, postural drainage, disposal of solid tissues to prevent disease transmission
Differential Diagnosis[edit | edit source]
- Adult Respiratory Distress Syndrome (ARDS)
- Bronchitis
- Congestive heart failure
- Gastroenteritis
- HIV infection and AIDS
- Inflammation of the rib cartilage (costochondritis)
- Meningitis
- Non-Legionnaire's pneumonia
- Pleural effusion
- Pneumonia caused by other organisms
- Prostatitis
- Septic shock
- Tuberculosis
Case Reports/ Case Studies[edit | edit source]
•Atypical Presentation of Legionnaire’s Disease: A Case Report and Review
•Severe Legionnaires disease complicated by multi-organ dysfunction in a previously healthy patient: a case report
•Legionnaires Disease: A Case Study
Resources[edit | edit source]
- Legionella(Legionnaire' Disease and Pontiac Fever)- Centers for Disease Control and Prevention
- Legionella.org
- Natural Remedies Encyclopedia
- Legionellosis- WHO
References[edit | edit source]
- ↑ Pedro-Botet M. L., Sabria-Leal M., Haro M., Rubio C., Gimenez G., Sopena N., Tor J.Nosocomial and community-acquired Legionella pneumonia: clinical comparative analysis. Eur. Respir. J.8199519291933 retrieved from https://erj.ersjournals.com/content/8/11/1929.short
- ↑ 2.0 2.1 Sharma L, Losier A, Tolbert T, Dela Cruz CS, Marion CR. Atypical Pneumonia: Updates on Legionella, Chlamydophila, and Mycoplasma Pneumonia. Clin Chest Med. 2017;38(1):45–58. doi:10.1016/j.ccm.2016.11.011 retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5679202/
- ↑ Myerowitz RL, Pasculle AW, Dowling JN et al. (1971) Opportunistic lung infection due to “Pittsburgh Pneumonia Agent”. N Engl J Med 301: 953–958.
- ↑ Cunha BA, Burillo A, Bouza E, Legionnaires' disease, The Lancet, Volume 387, Issue 10016, 2016, Pages 376-385, ISSN 0140-6736, https://doi.org/10.1016/S0140-6736(15)60078-2 retrieved from https://www.sciencedirect.com/science/article/pii/S0140673615600782
- ↑ Plouffe JF, Breiman RF, Fields BS, Herbert M, Inverso J, Knirsch C, Kolokathis A, Marrie TJ, Nicolle L, Schwartz DB, Azithromycin in the Treatment of Legionella Pneumonia Requiring Hospitalization, Clinical Infectious Diseases, Volume 37, Issue 11, December 2003, Pages 1475–1480, https://doi.org/10.1086/379329 retrieved from https://academic.oup.com/cid/article/37/11/1475/372119
- ↑ 6.0 6.1 Legionnaires' Disease available at https://emedicine.medscape.com/article/220163-overview
- ↑ 7.0 7.1 Legionnaires Disease- CDC available at https://www.cdc.gov/legionella/index.html