Laminectomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox"> | <div class="noeditbox"><div class="editorbox"> | ||
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})[ | This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}}) | ||
'''Original Editor '''- [https://www.physio-pedia.com/User:Shreya_Pavaskar Shreya Pavaskar] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
==Description== | |||
The word laminectomy literally means - excision of lamina. However in most cases, involves excision of the supraspinous ligament and some or all of the spinous process. A '''laminectomy''' is a surgical procedure that removes a portion of a vertebra called the lamina. It is a major spine operation with residual scar tissue and may result in post-laminectomy syndrome. This procedure is performed to decompress the spinal canal. As medical science advances, there are several techniques to accomplish spinal decompression, such as open or minimally invasive laminectomy, hemi-laminectomy, laminotomy and laminoplasty. Decompression techniques classify as direct and indirect; direct procedures involve those techniques with visualization of the dural sac during the surgery such as laminectomy. On the other hand, indirect decompression takes place without dural sac visualization. Laminectomy alone or associated with fusion is one of the most common procedures performed by a spinal surgeon.The word laminectomy literally means - excision of lamina. However in most cases, involves excision of the supraspinous ligament and some or all of the spinous process. Lamina is rarely removed if utterly required rather, it is done to break the continuity of the rigid ring of the spinal canal to allow the soft tissues within the canal to: 1) expand (decompress); 2) change the contour of the vertebral column; or 3) permit access to deeper tissue inside the spinal canal. | |||
Technique 1: Conventional Laminectomy - The skin was incised horizontally over a length of 8–10 cm in the midline along with lumbodorsal fascia. The paraspinal musculature was detached from the spinous process and laminae in a subperiosteal fashion and bilaterally retracted. Decompression was performed using standard techniques to remove the spinous process, lamina, and ligamentum flavum, along with partial medial facetectomy (limited to one-third of the facet joint) and rhizolysis of the traversing nerve roots (that is, the nerve roots that exit at the vertebral level below the surgical level). <ref>Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy. Journal of Neurosurgery: Spine. 2014 Aug 1;21(2):179-86.</ref> | |||
Technique 2: Minimally Invasive ULBD - Minimally Invasive Surgical (MIS) techniques include laminotomy and microendoscopic laminotomy with tubular retractors. Contemporary literature supports these procedures resulting in better preservation of posterior musculature, decreased intraoperative bleeding, and postoperative pain.<ref>Estefan M, GO CW. Laminectomy.</ref> | |||
== Relevant Anatomy == | |||
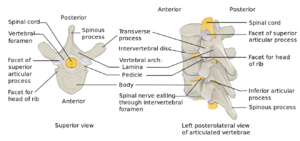
[[File:Vertebra anatomy.png|thumb|lamina and other elements of vertebrae]]The lamina is a posterior arch of the vertebral bone lying between the spinous process and the more lateral pedicles and the transverse processes of each vertebra. The lamina, facets and spinous process are major parts of the posterior elements that help guide the movement of the vertebrae and protect the spinal cord. The supraspinous ligament connects the tips of the spinous processes from the seventh cervical vertebra to the sacrum. It runs over the posterior aspect of the vertebrae. | |||
</div><div class="noeditbox"> | |||
==Indication== | |||
* presence of spinal canal stenosis | |||
* primary or secondary tumors | |||
* infection (peridural abscesses | |||
* trauma (fractures that compromise the spinal canal) | |||
* stenosis associated with the deformity | |||
* Ankylosing spondylitis (may help n relieving symptoms) | |||
* cervical myelopathy | |||
== Contraindication == | |||
* Spinal instability (is a contraindication for laminectomy without associated fusion technique) | |||
* Degenerative or isthmic spondylolisthesis (relative contraindication) | |||
* Severe scoliosis (relative contraindication) | |||
* Severe kyphosis (relative contraindication) | |||
==Clinical Presentation== | |||
* central stenosis- neurogenic claudication, which includes pain, tingling, or cramping sensation in the extremity | |||
* lateral recess, foraminal and extraforaminal lumbar stenosis - radiculopathy, patients with central stenosis may experience more symptoms in standing position and during walking and pain is usually relieved with leaning forward or in sitting position. | |||
==Diagnostic Tests== | |||
'''Cervical''' | |||
#[https://en.wikipedia.org/wiki/Spurling%27s_test#:~:text=The%20Spurling%20test%20is%20a,top%20of%20the%20patient's%20head. Spurling test.] | |||
#[https://www.physio-pedia.com/Cervical_Distraction_Test Distraction test]. | |||
#[[Upper Limb Tension Tests (ULTTs)|Upper limb tension test]]. | |||
#[https://www.youtube.com/watch?v=8_AHkiiPYS8 Shoulder abduction test.] | |||
#[https://www.physio-pedia.com/Tinel%E2%80%99s_Test Tinel's sign] | |||
#Compression test | |||
'''Lumbar''' | |||
#The [[Straight Leg Raise Test|straight leg raise test]]: | |||
#The contralateral (crossed) straight leg raise test | |||
#[[Straight Leg Raise Test|Lasègue’s Test]] - - see straight leg raise test | |||
#[https://www.youtube.com/watch?v=orb-VI51QF0 Bowstring test] | |||
#[https://www.thestudentphysicaltherapist.com/prone-knee-bend-test.html Prone knee bending] | |||
#[[Slump Test|Slump test]] | |||
#Muscle Weakness or Paresis | |||
#[[Reflexes]] | |||
#Hyperextension Test The patient needs to passively mobilise the trunk over the full range of extension, while the knees stay extended. The test indicates that the radiant pain is caused by disc herniation if the pain deteriorates. | |||
#Manual Testing and [[Sensation|Sensory Testing]] Look for hypoaesthesia, hypoalgesia, tingling or numbness | |||
'''Spinal canal stenosis''' | |||
# Bicycle Stress Test | |||
# Two-Stage Treadmill Test | |||
==Pre-Operative Exercises== | |||
1. Instruction in bed mobility, transfers, and body mechanics education with ADLs | |||
2. Instruction in basic home exercise program: | |||
* Ankle pumps | |||
* Gluteal sets | |||
* Quadriceps sets | |||
* Hamstring sets | |||
* Heel slides | |||
* Long and short arc LE extension | |||
* Transverse abdominis isometric contractions | |||
* Breathing relaxation exercises | |||
== Post-Operative Cervical laminectomy == | |||
'''Phase I: Immediate post Surgical Phase (IPSP) 06 weeks''' | |||
# Prevent excessive initial mobility or stress on tissues. | |||
# Diaphragmatic breathing | |||
# Relaxation exercises | |||
# Upper extremity extension isometric exercises | |||
# Multilevel fusions hard collar for 6 wks; one level fusions wear a collar as needed for a week or two | |||
Phase II: 6-9 weeks/2-3 times per week | |||
# | |||
==Post-Op lumbar laminectomy== | |||
'''Phase I (0 to 2 Weeks): Protective Phase''' | |||
Avoid bending and twisting, lifting, pushing and pulling 5kgs or more for two weeks. | |||
Limit sitting, including the car, to no more than 30 minutes at a time (standing/walk breaks). | |||
No extension range of motion or rotation exercises for eight weeks | |||
Educate regarding posture and body mechanics | |||
Light Stretching: Hip flexors, quadriceps, hamstrings, calf | |||
Gluteal, multifidus and transverse abdominus (without pelvic tilt) bracing/isometrics | |||
Walk for 10 mins twice daily | |||
'''Phase II (2 to 6 Weeks): Initial Strengthening Phase''' | |||
Frequency - One to two times a week, for four or more weeks | |||
Lifting Restrictions: Begin at 5kgs | |||
Keep spine neutral with focus on proper neuromuscular control | |||
Walking Progression: At least 30 minutes or more • Stationary Bike Recumbent: Can initiate at two weeks | |||
Transverse Abdominis/Multifidi Progression (maintain neutral spine) - start with isometrics and progress to SLR, marches, superman etc. | |||
Continue with Proper Glute Activation Exercises Eg.: prone hip extensions, bridges, side lying clams, side lying 90/90 leg lifts, side lying abduction, quadruped hip extension, bird dog | |||
Upper Extremity/Lower Extremity Strength Training - Step ups, leg press, wall squats, squats, etc. Balance (with transverse abdominis bracing): single leg stance, tandem, foam, etc. Upper extremity light resistive exercises (machines, theraband, free weights) | |||
Continue stretching exercises | |||
'''Phase III (6 to 8 Weeks): Progression to Advanced Strengthening''' | |||
Advanced core strength and stabilization exercises: Progress to weight bearing, balance, Swiss Ball, Reformer, etc. | |||
Progress to multi-planar exercises with upper extremity/lower extremity | |||
Progress upper extremity/lower extremity strengthening | |||
Begin running, agility and plyometrics for return to sport after 8 to 12 weeks (if symptoms stable and cleared) | |||
Lumbar Spine: More than eight weeks to improve lumbar extension range of motion, but avoid end-range Eg.: prone lying, prone on elbows, press-ups, and/or standing extensions (if no periphalization) | |||
== Resources == | |||
add appropriate resources here | |||
==References== | |||
<references /> | |||
</div> | </div> | ||
Revision as of 18:15, 13 January 2022
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (13/01/2022)
Original Editor - Shreya Pavaskar
Top Contributors - Shreya Pavaskar, Kim Jackson, Blessed Denzel Vhudzijena, Naomi O'Reilly, Kirenga Bamurange Liliane and Carina Therese Magtibay
Description[edit | edit source]
The word laminectomy literally means - excision of lamina. However in most cases, involves excision of the supraspinous ligament and some or all of the spinous process. A laminectomy is a surgical procedure that removes a portion of a vertebra called the lamina. It is a major spine operation with residual scar tissue and may result in post-laminectomy syndrome. This procedure is performed to decompress the spinal canal. As medical science advances, there are several techniques to accomplish spinal decompression, such as open or minimally invasive laminectomy, hemi-laminectomy, laminotomy and laminoplasty. Decompression techniques classify as direct and indirect; direct procedures involve those techniques with visualization of the dural sac during the surgery such as laminectomy. On the other hand, indirect decompression takes place without dural sac visualization. Laminectomy alone or associated with fusion is one of the most common procedures performed by a spinal surgeon.The word laminectomy literally means - excision of lamina. However in most cases, involves excision of the supraspinous ligament and some or all of the spinous process. Lamina is rarely removed if utterly required rather, it is done to break the continuity of the rigid ring of the spinal canal to allow the soft tissues within the canal to: 1) expand (decompress); 2) change the contour of the vertebral column; or 3) permit access to deeper tissue inside the spinal canal.
Technique 1: Conventional Laminectomy - The skin was incised horizontally over a length of 8–10 cm in the midline along with lumbodorsal fascia. The paraspinal musculature was detached from the spinous process and laminae in a subperiosteal fashion and bilaterally retracted. Decompression was performed using standard techniques to remove the spinous process, lamina, and ligamentum flavum, along with partial medial facetectomy (limited to one-third of the facet joint) and rhizolysis of the traversing nerve roots (that is, the nerve roots that exit at the vertebral level below the surgical level). [1]
Technique 2: Minimally Invasive ULBD - Minimally Invasive Surgical (MIS) techniques include laminotomy and microendoscopic laminotomy with tubular retractors. Contemporary literature supports these procedures resulting in better preservation of posterior musculature, decreased intraoperative bleeding, and postoperative pain.[2]
Relevant Anatomy[edit | edit source]
The lamina is a posterior arch of the vertebral bone lying between the spinous process and the more lateral pedicles and the transverse processes of each vertebra. The lamina, facets and spinous process are major parts of the posterior elements that help guide the movement of the vertebrae and protect the spinal cord. The supraspinous ligament connects the tips of the spinous processes from the seventh cervical vertebra to the sacrum. It runs over the posterior aspect of the vertebrae.Indication[edit | edit source]
- presence of spinal canal stenosis
- primary or secondary tumors
- infection (peridural abscesses
- trauma (fractures that compromise the spinal canal)
- stenosis associated with the deformity
- Ankylosing spondylitis (may help n relieving symptoms)
- cervical myelopathy
Contraindication[edit | edit source]
- Spinal instability (is a contraindication for laminectomy without associated fusion technique)
- Degenerative or isthmic spondylolisthesis (relative contraindication)
- Severe scoliosis (relative contraindication)
- Severe kyphosis (relative contraindication)
Clinical Presentation[edit | edit source]
- central stenosis- neurogenic claudication, which includes pain, tingling, or cramping sensation in the extremity
- lateral recess, foraminal and extraforaminal lumbar stenosis - radiculopathy, patients with central stenosis may experience more symptoms in standing position and during walking and pain is usually relieved with leaning forward or in sitting position.
Diagnostic Tests[edit | edit source]
Cervical
- Spurling test.
- Distraction test.
- Upper limb tension test.
- Shoulder abduction test.
- Tinel's sign
- Compression test
Lumbar
- The straight leg raise test:
- The contralateral (crossed) straight leg raise test
- Lasègue’s Test - - see straight leg raise test
- Bowstring test
- Prone knee bending
- Slump test
- Muscle Weakness or Paresis
- Reflexes
- Hyperextension Test The patient needs to passively mobilise the trunk over the full range of extension, while the knees stay extended. The test indicates that the radiant pain is caused by disc herniation if the pain deteriorates.
- Manual Testing and Sensory Testing Look for hypoaesthesia, hypoalgesia, tingling or numbness
Spinal canal stenosis
- Bicycle Stress Test
- Two-Stage Treadmill Test
Pre-Operative Exercises[edit | edit source]
1. Instruction in bed mobility, transfers, and body mechanics education with ADLs
2. Instruction in basic home exercise program:
- Ankle pumps
- Gluteal sets
- Quadriceps sets
- Hamstring sets
- Heel slides
- Long and short arc LE extension
- Transverse abdominis isometric contractions
- Breathing relaxation exercises
Post-Operative Cervical laminectomy[edit | edit source]
Phase I: Immediate post Surgical Phase (IPSP) 06 weeks
- Prevent excessive initial mobility or stress on tissues.
- Diaphragmatic breathing
- Relaxation exercises
- Upper extremity extension isometric exercises
- Multilevel fusions hard collar for 6 wks; one level fusions wear a collar as needed for a week or two
Phase II: 6-9 weeks/2-3 times per week
Post-Op lumbar laminectomy[edit | edit source]
Phase I (0 to 2 Weeks): Protective Phase
Avoid bending and twisting, lifting, pushing and pulling 5kgs or more for two weeks.
Limit sitting, including the car, to no more than 30 minutes at a time (standing/walk breaks).
No extension range of motion or rotation exercises for eight weeks
Educate regarding posture and body mechanics
Light Stretching: Hip flexors, quadriceps, hamstrings, calf
Gluteal, multifidus and transverse abdominus (without pelvic tilt) bracing/isometrics
Walk for 10 mins twice daily
Phase II (2 to 6 Weeks): Initial Strengthening Phase
Frequency - One to two times a week, for four or more weeks
Lifting Restrictions: Begin at 5kgs
Keep spine neutral with focus on proper neuromuscular control
Walking Progression: At least 30 minutes or more • Stationary Bike Recumbent: Can initiate at two weeks
Transverse Abdominis/Multifidi Progression (maintain neutral spine) - start with isometrics and progress to SLR, marches, superman etc.
Continue with Proper Glute Activation Exercises Eg.: prone hip extensions, bridges, side lying clams, side lying 90/90 leg lifts, side lying abduction, quadruped hip extension, bird dog
Upper Extremity/Lower Extremity Strength Training - Step ups, leg press, wall squats, squats, etc. Balance (with transverse abdominis bracing): single leg stance, tandem, foam, etc. Upper extremity light resistive exercises (machines, theraband, free weights)
Continue stretching exercises
Phase III (6 to 8 Weeks): Progression to Advanced Strengthening
Advanced core strength and stabilization exercises: Progress to weight bearing, balance, Swiss Ball, Reformer, etc.
Progress to multi-planar exercises with upper extremity/lower extremity
Progress upper extremity/lower extremity strengthening
Begin running, agility and plyometrics for return to sport after 8 to 12 weeks (if symptoms stable and cleared)
Lumbar Spine: More than eight weeks to improve lumbar extension range of motion, but avoid end-range Eg.: prone lying, prone on elbows, press-ups, and/or standing extensions (if no periphalization)
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy. Journal of Neurosurgery: Spine. 2014 Aug 1;21(2):179-86.
- ↑ Estefan M, GO CW. Laminectomy.