Introduction to Vestibular Rehabilitation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 56: | Line 56: | ||
** Ototoxicity, barotrauma, acoustic neuroma | ** Ototoxicity, barotrauma, acoustic neuroma | ||
{{#ev:youtube| | {{#ev:youtube|kx4mQB0QzvQ/}}<ref>Zero To Finals. Understanding the Causes of Vertigo. Available from: https://www.youtube.com/watch?v=kx4mQB0QzvQ [last accessed 15/5/2021]</ref> | ||
== Signs and Symptoms of Vestibular Disorders == | == Signs and Symptoms of Vestibular Disorders == | ||
Revision as of 01:34, 15 May 2021
Introduction[edit | edit source]
Vestibular rehabilitation is an evidence-based approach to managing dizziness, vertigo, motion sensitivity, balance and postural control issues that occur due to vestibular dysfunction.[1]
Patients with vestibular impairment typically experience issues with gaze stability, motion stability, and balance and postural control. Vestibular rehabilitation, therefore, includes exercises that are focused towards these areas of pathology or dysfunction. However, the specific treatment approach will depend on the patient’s presentation.[1]
This page introduces vestibular dysfunction in general in order to provide background information and specific context for vestibular rehabilitation.
Epidemiology[edit | edit source]
Vestibular disturbance is a significant issue globally. It is estimated that 35.4 percent of North Americans aged over 40 have experienced some form of vestibular dysfunction. The likelihood of experiencing vestibular dysfunction increases with age.[2]
- 80 percent of people aged over 65 years experience dizziness - in 50 percent of cases this dizziness is caused by benign paroxysmal positional vertigo (BPPV)[2]
- 75 percent of adults aged over 70 years have a balance impairment (often associated with vestibular dysfunction and sensory loss in the feet)[3]
- Nearly 85 percent of adults aged over 80 years have vestibular dysfunction[3]
These numbers are significant as having vestibular dysfunction makes an individual eight times more likely to experience a fall[3] and falls are associated with significant morbidity, mortality[3] and economic cost.[4]
Moreover, the number of people experiencing vestibular dysfunction is expected to grow due to our ageing populations.[1]
Defining Dizziness and Vertigo[edit | edit source]
Dizziness and vertigo are not interchangeable terms.[1]
Dizziness is a non-specific term used to describe a variety of sensations such as light-headedness, swaying, disorientation and presyncope.[5]
Vertigo is a specific type of dizziness which is defined as the illusion of movement that occurs in the environment. Dizziness is not associated with this illusion of movement.[1]
Vertigo is caused by both peripheral and central vestibular diseases.[6] It is often rotational (i.e. the room spins around the patient), but there can also be linear disruptions or, less commonly, the patient might feel that his / her body is moving relative to the environment.[1]
Dizziness and vertigo are both purely subjective phenomena. There is no objective means of measuring them, so the patient’s subjective history is key.[1]
Causes of Dizziness[edit | edit source]
There are many causes of dizziness including:
- Cardiovascular dysfunction[1]
- Strokes are a rare cause of dizziness. The figures vary, but recent reports suggest strokes are the underlying cause of symptoms in around 3 to 5 percent of patients visiting emergency departments with dizziness and vertigo[7]
- Orthostatic hypotension
- Arrhythmias
- Neurological dysfunction[1]
- Dizziness is a common symptom associated with multiple sclerosis (MS)[8] and it can mimic a peripheral vestibular disorder and cause vertigo
- Vision dysfunctions[1][9]
- Any issues resulting in degradation of visual input can cause dizziness. These might occur in the eye (e.g. macular degeneration, cataracts), be related to the optic nerve, or be due to problems with visual processing
- Psychogenic dizziness[1]
- It is not common to see purely psychogenic dizziness and vertigo. However, dizziness can trigger anxiety and anxiety can cause dizziness[9]
- Cervicogenic dizziness
- Vestibular system disorders[1][11]
- Head trauma such as whiplash or concussion
- Vestibular system degeneration (age related)
- Vestibular neuritis / labyrinthitis
- BPPV
- Endolymphatic hydrops (e.g. Meniere’s disease)
- Ototoxicity, barotrauma, acoustic neuroma
Signs and Symptoms of Vestibular Disorders[edit | edit source]
- Nystagmus (involuntary eye movement)
- Vertigo
- Dizziness
- Imbalance or ataxia
- Compromised gaze stability (decreased visual acuity with head movement - i.e. the vestibular ocular reflex (VOR) is affected)
Anatomy of the Peripheral Vestibular System[edit | edit source]
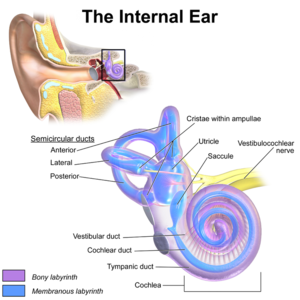
The outer ear consists of the external acoustic meatus. The tympanic membrane (i.e. eardrum) separates the outer ear from the middle ear. The inner ear contains the vestibular system and the cochlear.[1]
As is shown in figure 1, the vestibular apparatus consists of three semicircular canals, the utricle and the saccule (which together form the otoliths).[13]
The semicircular canals are specialised mechanoreceptors that enable us to access information about angular velocity.[14]
There are three canals:
- Anterior
- Posterior
- Horizontal (or lateral)
The anterior and posterior canals have a conjoint canal, called the common crus.[1]
The otoliths (i.e. utricle and saccule) are positioned in the central chamber known as the vestibule. They provide information about linear acceleration.[15]
The cochlear is also positioned in the inner ear and it is responsible for hearing.
Travelling within the membranous labyrinth of the inner ear is a clear, viscous fluid called endolymph:[1][13]
- The acceleration of endolymph in the vestibular apparatus enables people to perceive balance and equilibrium
- Endolymph in the cochlear duct plays an important role in the perception of sound
Because endolymph travels in both the vestibular apparatus and the cochlear, any conditions that cause increased endolymphatic pressure (e.g. Meniere’s disease) will affect the cochlear as well.[1]
Planes of Movement[edit | edit source]
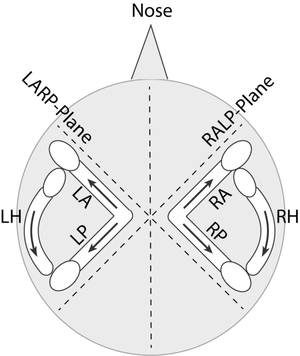
The vestibular apparatus has three specific planes of motion or movement:
- Anterior
- Posterior
- Horizontal
There are six semicircular canals in total (three on the right and three on the left). Each plane of movement has two canals in it (i.e. there are three coplanar pairs).[16]See figure 2.
- The anterior and posterior canals sit on the vertical plane
- The anterior and posterior canals are also oriented along two diagonal planes:
- The LARP plane = left anterior right posterior plane
- RALP plane = right anterior left posterior plane
- The horizontal canals are positioned on a 30 degree angle (i.e. close to horizontal)
Ampullae[edit | edit source]
The ampullae is a widened area in the semicircular canals. It contains the neurons that detect head movement. The neurons are embedded in a matrix of blood vessels and connective tissue called the crista ampullaris. Attached to these neurons are specialised mechanoreceptors called “hair cells”.[17] Each hair cell contains a large number of cross-linked actin filaments, which are called stereocilia. Stereocilia move in response to the acceleration of endolymph.[17] Essentially, they act as motion sensors that are able to convert angular head movements into afferent neural discharges.[1]
Cupula[edit | edit source]
The cupula is the gelatinous part of the crista ampullaris in which the hair cells are embedded. It extends from the crista to the roof of the ampullae.[1]
The cupula creates a fluid barrier - the endolymph cannot circulate within the cupula, but it is affected by movements of the endolymph around it:[18]
- If you turn your head in the plane of a semicircular canal, the movement of the endolymph generates a force across the cupula, pushing it away from the direction your head is moving
- This moves the hair cells in the crista
Linear accelerations create an equal force on either side of the cupula, so displacement does not occur.[18] The semicircular canals are, therefore, unable to detect linear movement patterns and are also insensitive to gravity.[1]
Otoliths[edit | edit source]
Unlike the semicircular canals, the otoliths detect translational or linear movements,[18] including:[1]
- Forward to backward
- Up and down
- Side to side (not turning)
- Static head position relative to gravity
Both the utricle and saccule contain a macula in which neuronal hair cells are anchored.[1][19] The hair cells sit under a gelatinous layer, which in turn is under the otolithic membrane.[19]
The otolithic membrane has calcium carbonate crystals, also known as otoconia embedded in it.[19]
The otolithic membrane is heavier than surrounding structures and fluids because of the weight of the otoconia. Because of this weight, when you tilt your head, gravity causes the membrane to move in relation to the macula. This displaces the hair cells and generates a receptor potential.[19]
Vestibular Reflexes[edit | edit source]
Vestibulo-spinal reflex (VSR)[edit | edit source]
The VSR stabilises the body. [21] However, while assessing a patient's balance will activate his / her vestibulo-spinal reflex, it does not provide enough information about the vestibular apparatus to be relevant in this patient group.[1]
Vestibulo-Ocular Reflex (VOR)[edit | edit source]
The VOR enables gaze stability by maintaining stable vision during head motion.[22] There are two components to the VOR and both work together to ensure gaze stability while the head turns.[1][21]
- Angular VOR[21]
- Mediated by the semicircular canals
- Compensates for rotation
- Primarily responsible for gaze stabilisation
- Linear VOR[21]
- Mediated by the otoliths
- Compensates for translation
- More important when looking at targets close up and when head moves at reasonably high frequencies
When you turn your head to the right:[1]
- The right horizontal canal is excited and the left is inhibited (in a push-pull arrangement)
- The right horizontal canal activates the right medial rectus and left lateral rectus muscles to pull eyes to the left
- The left horizontal canal inhibits the right lateral rectus and left medial rectus muscles, which allows this movement to occur
The VOR is the fastest human reflex - operating in around 14 milliseconds.[1] The reason for this speed is that the VOR pathway:[23]
- Is relatively short
- Uses only sensory information from the vestibular system to activate the motoneurons
Because of this speed, the VOR must be very accurate (98 percent or more) to ensure that there is no blurring / skipping of the visual field when you move your head.[1][23]
Gain[edit | edit source]
VOR gain is defined as the amount of eye rotation relative to the amount of head rotation. It is often used as a physiological measure of vestibular function and it tends to decline with age.[24]
VOR gain should be near unity (i.e. close to 1).[24] This means that the magnitude of eye velocity should be equal to the magnitude of head velocity.[25] VOR gain is typically around 0.96 - 0.97, but it can operate anywhere from 0.5 to 2.[1] It has been proposed that a VOR gain of less than 0.68 is the cut off point between normal and too low.[24]
VOR gain is mediated by the central nervous system control (CNS) in a process called adaptation. When the CNS modifies VOR gain, it changes the sensitivity of the reflex to enable us to adapt to the environment. Thus, gaze stabilisation exercises, which form part of vestibular rehabilitation, can be thought of as adaptation exercises.[1]
Nystagmus[edit | edit source]
Nystagmus is one of the signs of vestibular dysfunction and it is defined as “a rhythmic, involuntary, rapid, oscillatory movement of the eyes.”[26]
It can result in slow or fast movements or a combination of the two.[26] Movements may be:[27]
- Side to side (horizontal nystagmus)
- Up and down (vertical nystagmus)
- In a circle (rotary nystagmus)
- Continuous or sudden[26]
- Related to specific gaze or head positioning triggers[26]
- Pathological or physiological (i.e. normal)[1]
While every reflex has a central and peripheral component, the saccade system (i.e. rapid eye movements) is considered more centrally mediated and the VOR is more peripherally mediated. Therefore, nystagmus can be considered a combination of peripheral and central mediated reflexes.[1]
Types of nystagmus include:
- Jerk:
Pendular:[29]
- The eye moves in sinusoidal pattern (i.e. like a pendulum)
- Only slow eye movements present - does not typically have a fast phase
- Centrally mediated[1]
Summary
- Vestibular dysfunction is a significant issue that becomes more prevalent as we age
- There are many different causes of dizziness, all of which will be managed differently
- Dizziness and vertigo are not interchangeable terms
- Understanding the anatomy of the vestibular system is essential to vestibular rehabilitation
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 Tonks B. Introduction to Vestibular Rehabilitation Course. Physioplus. 2021.
- ↑ 2.0 2.1 Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Arch Intern Med. 2009;169(10):938-44.
- ↑ 3.0 3.1 3.2 3.3 Hall CD, Herdman SJ, Whitney SL, Cass SP, Clendaniel RA, Fife TD et al. Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline: FROM THE AMERICAN PHYSICAL THERAPY ASSOCIATION NEUROLOGY SECTION. J Neurol Phys Ther. 2016;40(2):124-55.
- ↑ Haddad YK, Bergen G, Florence CS. Estimating the economic burden related to older adult falls by state. J Public Health Manag Pract. 2019;25(2):E17-E24.
- ↑ Kerber KA, Brown DL, Lisabeth LD, Smith MA, Morgenstern LB. Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke. 2006;37(10):2484-2487.
- ↑ Kovacs E, Wang X, Grill E. Economic burden of vertigo: a systematic review. Health Econ Rev. 2019;9(1):37.
- ↑ Saber Tehrani AS, Kattah JC, Kerber KA, Gold DR, Zee DS, Urrutia VC et al. Diagnosing stroke in acute dizziness and vertigo: pitfalls and pearls. Stroke. 2018;49(3):788-795.
- ↑ Marrie RA, Cutter GR, Tyry T. Substantial burden of dizziness in multiple sclerosis. Mult Scler Relat Disord. 2013;2(1):21-8.
- ↑ 9.0 9.1 Armstrong D, Charlesworth E, Alderson AJ, Elliott DB. Is there a link between dizziness and vision? A systematic review. Ophthalmic Physiol Opt. 2016;36(4):477-86.
- ↑ Reiley AS, Vickory FM, Funderburg SE, Cesario RA, Clendaniel RA. How to diagnose cervicogenic dizziness. Arch Physiother. 2017;7:12.
- ↑ VEDA. Types of vestibular disorders. Available from: https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/ (accessed 14 May 2021).
- ↑ Zero To Finals. Understanding the Causes of Vertigo. Available from: https://www.youtube.com/watch?v=kx4mQB0QzvQ [last accessed 15/5/2021]
- ↑ 13.0 13.1 Casale J, Agarwal A. Anatomy, Head and Neck, Ear Endolymph. [Updated 2021 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531505/
- ↑ Rabbitt RD. Semicircular canal biomechanics in health and disease. Journal of neurophysiology. 2018 Dec 19;121(3):732-55.
- ↑ Kniep R, Zahn D, Wulfes J, Walther LE. The sense of balance in humans: Structural features of otoconia and their response to linear acceleration. PloS one. 2017 Apr 13;12(4):e0175769.
- ↑ Robertson M. Vestibular Anatomy and Neurophysiology Course. Physioplus. 2019.
- ↑ 17.0 17.1 Casale J, Browne T, Murray I, et al. Physiology, Vestibular System. [Updated 2020 May 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532978/
- ↑ 18.0 18.1 18.2 Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Semicircular Canals. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10863/
- ↑ 19.0 19.1 19.2 19.3 Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Otolith Organs: The Utricle and Sacculus. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10792/
- ↑ Neuroscientifically Challenged. 2-Minute Neuroscience: Vestibular System. Available from: https://www.youtube.com/watch?v=P3aYqxGesqs [last accessed 15/5/2021]
- ↑ 21.0 21.1 21.2 21.3 Hain TC. Vestibular reflexes [Internet]. Chicago Dizziness and Balance. 2021 [cited 14 May 2021]. Available from: https://dizziness-and-balance.com/anatomy/physiology/vestibular-reflexes.html
- ↑ Dunlap PM, Mucha A, Smithnosky D, Whitney SL, Furman JM, Collins MW et al. The gaze stabilization test following concussion. J Am Acad Audiol. 2018:10.3766/jaaa.18015.
- ↑ 23.0 23.1 Broussard DM, Titley HK, Heskin-Sweezie R. Motor learning in the vestibulo-ocular reflex. In: Koob GF, Le Moal M, Thompson RF editors. Encyclopedia of Behavioral Neuroscience. Academic Press. 2010. p273-9.
- ↑ 24.0 24.1 24.2 Anson ER, Bigelow RT, Carey JP, Xue QL, Studenski S, Schubert MC et al. VOR gain Is related to compensatory saccades in healthy older adults. Front Aging Neurosci. 2016;8:150.
- ↑ Schubert MC, Migliaccio AA. New advances regarding adaptation of the vestibulo-ocular reflex. J Neurophysiol. 2019;122(2):644-58.
- ↑ 26.0 26.1 26.2 26.3 Sekhon RK, Rocha Cabrero F, Deibel JP. Nystagmus Types. [Updated 2020 Nov 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539711/
- ↑ Boyd K. What is nystagmus? [Internet]. American Academy of Ophthalmology [cited 14 May 2021]. Available from: https://www.aao.org/eye-health/diseases/what-is-nystagmus
- ↑ Hain TC. Spontaneous nystagmus [Internet]. Chicago Dizziness and Hearing. 2021 [cited 14 May 2021]. Available from: https://dizziness-and-balance.com/practice/nystagmus/spontaneous.html
- ↑ Hain TC. Pendular nystagmus [Internet]. Chicago Dizziness and Hearing. 2021 [cited 14 May 2021]. Available from: https://dizziness-and-balance.com/practice/nystagmus/pendular.html