Introduction to Frailty: Difference between revisions
(added to introduction section) |
(edited Fried's section) |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Christina Nowak]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Christina Nowak]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction to Frailty == | == Introduction to Frailty == | ||
Frailty is associated with an increased risk of falls, harm events, institutionalisation, care needs and disability/death.<ref name=":0">Buxton S. An Introduction to Frailty course. Physioplus. 2020.</ref> It affects quality of life and is becoming more common | Frailty is a clinical state that is associated with an increased risk of falls, harm events, institutionalisation, care needs and disability/death.<ref name=":0">Buxton S. An Introduction to Frailty course. Physioplus. 2020.</ref> It affects quality of life and is becoming more common with ageing populations.<ref name=":0" /> While it is generally accepted that frailty exists, it remains difficult to define and measure as it manifests differently in each individual. However, a working definition of frailty is as follows: it is a distinct clinical entity from ageing, but it is related to the ageing process. It consists of multi-system dysregulation leading to a loss of physiological reserve. This loss of reserve means that the individual living with frailty is in a state of increased vulnerability to stressors meaning they are more likely to suffer adverse effects from treatments, diseases or infections. Morley et al (2013) also provide the following definition: | ||
<blockquote>“Frailty is a clinical state in which there is an increase in an individual’s vulnerability for developing increased dependency and/or mortality when exposed to a stressor.”<ref>Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabel R et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013. 14(6): 392-7.</ref></blockquote> | <blockquote>“Frailty is a clinical state in which there is an increase in an individual’s vulnerability for developing increased dependency and/or mortality when exposed to a stressor.”<ref>Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabel R et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013. 14(6): 392-7.</ref></blockquote> | ||
These are fairly complex definitions, but they can ultimately be broken down into two key concepts:<ref name=":0" /> | |||
* | * Frailty is a distinct process separate from aging, but related to aging. While older people tend to be more frailty, you will not be frail just because you are old. Frailty depends on your physiological state and how well you can respond to stressors (injury/illness). | ||
* Frailty involves multiple systems rather than just a single body system. Frail individuals will usually have a number of co-morbidities (eg cardiovascular, musculoskeletal and neurological).<ref name=":0" /> | * Frailty involves multiple systems rather than just a single body system. Frail individuals will usually have a number of co-morbidities (eg cardiovascular, musculoskeletal and neurological).<ref name=":0" /> | ||
Frailty is a dynamic state - there is evidence that frailty could be modifiable and has greater reversibility than disability.<ref name=":1">Clegg A, Bates C, Young J, Ryan R, Nichols L, Teale EA et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age and Ageing. 2016; 45(3): 353–60, <nowiki>https://doi.org/10.1093/ageing/afw039</nowiki>.</ref> An individual's frailty level can be influenced by an intervention or lack of intervention.<ref name=":0" /> Overall, if unmanaged, a frail individual will follow a trajectory towards death and disability.<ref name=":0" /><ref name=":1" /> It is estimated that 25% to 50% of individuals aged over 85 years are frail, but equally this means that up to 75% of people aged over 85 may not be frail.<ref name=":2">Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in older people, The Lancet. 2013; 381(9868): 752-62. Available from <nowiki>https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4098658/</nowiki></ref> Importantly, up to three quarters of people over 85 years might not be frail, so as Clegg et al (2013) note, it is important to consider why some individuals become frail and how it might be detected and prevented.<ref name=":2" /> | |||
== Models of Frailty == | |||
There are two main theories of frailty: Fried's Phenotpye Model and Rockwood's Accumulation of Deficits Model. It is important to understand that these are not competing models. They should be considered as complimentary - both have been validated and have been used to develop various assessment tools and treatment indicators. In some instances, one model will work better than the other. For instance, Fried's model is particularly useful when assessing an individual who is who is pre-frail whereas Rockwood's model is more useful when assessing how cognitive issues may be impacting frailty.<u></u> | |||
== Fried's Phenotype Model == | == Fried's Phenotype Model == | ||
Fried's Phenotype Model was first published in 2001.<ref>Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T et al. Frailty in older adults: evidence for a phenotype. J Gerontol. 2001. 56A(3): 146-56.</ref> It is a yes-no model based on five sub categories. Each subcategory will be scored as 0 (no) or 1 (yes). It assumes an individual is frail if s/he has a score of greater than three.<ref name=":0" /> The five categories are: | |||
# '''Physical Inactivity''' - measured using the usual outcome measures you would expect | # '''Physical Inactivity''' - measured using the usual outcome measures you would expect | ||
# '''Low muscle strength''' - can be measured in grip strength | # '''Low muscle strength''' - can be measured in grip strength - <21kgf in men and <14 kgf in women (NB this is dependent on ethnicity) | ||
# '''Slow gait speed''' - less than 0.8 m/s with or without a walking aid | # '''Slow gait speed''' - less than 0.8 m/s with or without a walking aid | ||
# '''Exhaustion/ fatigue''' - this is self-reported | # '''Exhaustion/ fatigue''' - this is self-reported | ||
# '''Weight loss -''' loss of 10lbs or more in 1 year | # '''Weight loss -''' loss of 10lbs or more in 1 year | ||
The scoring is as follows: 0-1 = not frail 1-2 = pre-frail 3+ = frail (mild, moderate and severe) | |||
When using this model, it is important to remember that frailty is a '''multi-system dysregulation'''. If an impairment is clearly due to a mono-articular or single system problem (eg low grip strength following a hand injury) then this must be considered when assessing for frailty. It should be noted also that this model focuses solely on physical attributes of frailty. Some therefore consider that it is an incomplete model as it does not address cognitive aspects or chronic conditions which are associated with frailty.<ref>Fried LP, Xue QL, Cappola AR, Ferrucci L, Chanves P, Varadhan R, Guralnik JM, Leng SX, Semba RD, et al. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol. 2009. 64(10): 1049-57.</ref> However, this focus on physical attributes makes Fried's Model useful for physiotherapists as, it provides clear direction when creating treatment plans to address frailty - for instance if a patient is shown to have low muscle strength, treatment would focus on strengthening. Similarly patients who are found to be physically inactive would need to increase their activity levels.<ref name=":0" /> <u></u> | |||
== Rockwood's Accumulation of Deficits Model == | == Rockwood's Accumulation of Deficits Model == | ||
The Accumulation of Deficits approach considers the number of conditions present in the individual and gives the person a score of 0 to 1 known as the [https://consultgeri.org/try-this/general-assessment/issue-34.pdf Frailty Index]. The score is calculated through the (total number of impairments in the individual)/ (the total number of impairments examined). Impairment can be any sort of defecit from symptoms, signs, diseases or disabilities. This model dichotomizes each variable, you either have the defecit or you do not. The higher your overall score towards 1.0, the more frail you are considered<sup>5</sup>. Think of it as a descriptor of overall burden on a persons ability to cope. The model has high predictive ability for mortality in both men and women<ref>Song X, Mitnitski A, Rockwood MD. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010. 58: 681-7. </ref>. | The Accumulation of Deficits approach considers the number of conditions present in the individual and gives the person a score of 0 to 1 known as the [https://consultgeri.org/try-this/general-assessment/issue-34.pdf Frailty Index]. The score is calculated through the (total number of impairments in the individual)/ (the total number of impairments examined). Impairment can be any sort of defecit from symptoms, signs, diseases or disabilities. This model dichotomizes each variable, you either have the defecit or you do not. The higher your overall score towards 1.0, the more frail you are considered<sup>5</sup>. Think of it as a descriptor of overall burden on a persons ability to cope. The model has high predictive ability for mortality in both men and women<ref>Song X, Mitnitski A, Rockwood MD. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010. 58: 681-7. </ref>. | ||
Revision as of 06:47, 12 June 2020
Introduction to Frailty[edit | edit source]
Frailty is a clinical state that is associated with an increased risk of falls, harm events, institutionalisation, care needs and disability/death.[1] It affects quality of life and is becoming more common with ageing populations.[1] While it is generally accepted that frailty exists, it remains difficult to define and measure as it manifests differently in each individual. However, a working definition of frailty is as follows: it is a distinct clinical entity from ageing, but it is related to the ageing process. It consists of multi-system dysregulation leading to a loss of physiological reserve. This loss of reserve means that the individual living with frailty is in a state of increased vulnerability to stressors meaning they are more likely to suffer adverse effects from treatments, diseases or infections. Morley et al (2013) also provide the following definition:
“Frailty is a clinical state in which there is an increase in an individual’s vulnerability for developing increased dependency and/or mortality when exposed to a stressor.”[2]
These are fairly complex definitions, but they can ultimately be broken down into two key concepts:[1]
- Frailty is a distinct process separate from aging, but related to aging. While older people tend to be more frailty, you will not be frail just because you are old. Frailty depends on your physiological state and how well you can respond to stressors (injury/illness).
- Frailty involves multiple systems rather than just a single body system. Frail individuals will usually have a number of co-morbidities (eg cardiovascular, musculoskeletal and neurological).[1]
Frailty is a dynamic state - there is evidence that frailty could be modifiable and has greater reversibility than disability.[3] An individual's frailty level can be influenced by an intervention or lack of intervention.[1] Overall, if unmanaged, a frail individual will follow a trajectory towards death and disability.[1][3] It is estimated that 25% to 50% of individuals aged over 85 years are frail, but equally this means that up to 75% of people aged over 85 may not be frail.[4] Importantly, up to three quarters of people over 85 years might not be frail, so as Clegg et al (2013) note, it is important to consider why some individuals become frail and how it might be detected and prevented.[4]
Models of Frailty[edit | edit source]
There are two main theories of frailty: Fried's Phenotpye Model and Rockwood's Accumulation of Deficits Model. It is important to understand that these are not competing models. They should be considered as complimentary - both have been validated and have been used to develop various assessment tools and treatment indicators. In some instances, one model will work better than the other. For instance, Fried's model is particularly useful when assessing an individual who is who is pre-frail whereas Rockwood's model is more useful when assessing how cognitive issues may be impacting frailty.
Fried's Phenotype Model[edit | edit source]
Fried's Phenotype Model was first published in 2001.[5] It is a yes-no model based on five sub categories. Each subcategory will be scored as 0 (no) or 1 (yes). It assumes an individual is frail if s/he has a score of greater than three.[1] The five categories are:
- Physical Inactivity - measured using the usual outcome measures you would expect
- Low muscle strength - can be measured in grip strength - <21kgf in men and <14 kgf in women (NB this is dependent on ethnicity)
- Slow gait speed - less than 0.8 m/s with or without a walking aid
- Exhaustion/ fatigue - this is self-reported
- Weight loss - loss of 10lbs or more in 1 year
The scoring is as follows: 0-1 = not frail 1-2 = pre-frail 3+ = frail (mild, moderate and severe)
When using this model, it is important to remember that frailty is a multi-system dysregulation. If an impairment is clearly due to a mono-articular or single system problem (eg low grip strength following a hand injury) then this must be considered when assessing for frailty. It should be noted also that this model focuses solely on physical attributes of frailty. Some therefore consider that it is an incomplete model as it does not address cognitive aspects or chronic conditions which are associated with frailty.[6] However, this focus on physical attributes makes Fried's Model useful for physiotherapists as, it provides clear direction when creating treatment plans to address frailty - for instance if a patient is shown to have low muscle strength, treatment would focus on strengthening. Similarly patients who are found to be physically inactive would need to increase their activity levels.[1]
Rockwood's Accumulation of Deficits Model[edit | edit source]
The Accumulation of Deficits approach considers the number of conditions present in the individual and gives the person a score of 0 to 1 known as the Frailty Index. The score is calculated through the (total number of impairments in the individual)/ (the total number of impairments examined). Impairment can be any sort of defecit from symptoms, signs, diseases or disabilities. This model dichotomizes each variable, you either have the defecit or you do not. The higher your overall score towards 1.0, the more frail you are considered5. Think of it as a descriptor of overall burden on a persons ability to cope. The model has high predictive ability for mortality in both men and women[7].
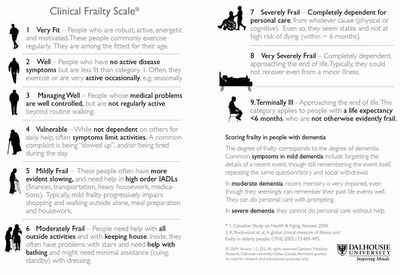
Clearly it is difficult to use this model in a quick glance or when meeting someone for first time. It requires time to accurately assess and understand the defecits an individual has therefore this is a useful model for primary care (GPs or Geriatricians) and where accurate detailed records of patients are kept. To make this model easier to use there are a number of developments. One being the electronic frailty index (eFI) which uses computer records to add up and accumulate the records giving a score quickly which is easily accessible. The other is the clinical frailty scale which is a really straightforward and accessible for clinicians of any speciality to use. It looks simpe, it is simple yet it is incredibly accurate at measuring a persons frailty score. As you can see the score uses a simple 1 to 9 scale with the pictures and words indicating the physcial abilities expected by people living with each level of frailty.
Particular attention should be payed to those who score 5 or more as this is the marker for requring a comprehensive geriatric assessment and often referral to geriatric or frailty specialists, A 2017 Cochrane review found that older people are more likely to be alive and in their own homes at follow-up if they received CGA on admission to hospital[8].
Conclusions[edit | edit source]
Both theoretical frameworks can be referenced and are valid in the literature. Fried’s criteria focusses solely on the physical aspects of frailty whereas Rockwood considers other deficits and chronic conditions.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Buxton S. An Introduction to Frailty course. Physioplus. 2020.
- ↑ Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabel R et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013. 14(6): 392-7.
- ↑ 3.0 3.1 Clegg A, Bates C, Young J, Ryan R, Nichols L, Teale EA et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age and Ageing. 2016; 45(3): 353–60, https://doi.org/10.1093/ageing/afw039.
- ↑ 4.0 4.1 Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in older people, The Lancet. 2013; 381(9868): 752-62. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4098658/
- ↑ Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T et al. Frailty in older adults: evidence for a phenotype. J Gerontol. 2001. 56A(3): 146-56.
- ↑ Fried LP, Xue QL, Cappola AR, Ferrucci L, Chanves P, Varadhan R, Guralnik JM, Leng SX, Semba RD, et al. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol. 2009. 64(10): 1049-57.
- ↑ Song X, Mitnitski A, Rockwood MD. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010. 58: 681-7.
- ↑ Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, Conroy SP, Kircher T, Somme D, Saltvedt I, Wald H. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane database of systematic reviews. 2017(9). Available from: https://www.cochrane.org/CD006211/EPOC_comprehensive-geriatric-assessment-older-adults-admitted-hospital (last accessed 4.5.2019)