Introduction to Burns: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "PhysioPlus " to "Plus ") |
No edit summary |
||
| (31 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter] | <div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== What is a Burn? == | == What is a Burn? == | ||
A burn is an injury to the skin or other organic tissue primarily caused by exposure to heat or other causative agents (radiation, electricity, chemicals).<ref name=":5">Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. [https://www.nature.com/articles/s41572-020-0145-5 Burn injury.] Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.</ref> According to WHO, it is a global public health problem, | A '''burn''' is an injury to the skin or other organic tissue primarily caused by exposure to heat or other causative agents (radiation, electricity, chemicals).<ref name=":5">Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. [https://www.nature.com/articles/s41572-020-0145-5 Burn injury.] Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.</ref> It is the result of energy transfer to the body. According to the World Health Organization (WHO), it is a global public health problem, causing an estimated 180,000 deaths annually.<ref name=":4">World Health Organization. [https://www.who.int/news-room/fact-sheets/detail/burns Burns]. 2020. Available from: <nowiki>https://www.who.int/news-room/fact-sheets/detail/burns</nowiki> [Accessed 29th May 2022].</ref> It is among the leading causes of disability in low and middle-income countries and almost two-thirds of burns occur in the WHO African and South-East Asia regions. Burn injuries occur in all genders, however females have slightly higher rates of death as compared to males. They also affect all age groups and are the fifth most common cause of non-fatal childhood injuries.<ref name=":4" /> | ||
== Types of | Burn injuries do not only affect the skin. They can also affect tissue, organ and system networks (e.g. from smoke inhalation) and have psychological effects. | ||
For a review of skin anatomy and physiology, please read [https://www.physio-pedia.com/Skin_Anatomy,_Physiology,_and_Healing_Process?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#Skin_Anatomy_and_Physiology this article]. | |||
For a list of wound care terminology, please see [https://www.physio-pedia.com/Wound_Care_Terminology?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal this article]. | |||
== Types of Burn Injuries == | |||
==== 1. Thermal Burns ==== | ==== 1. Thermal Burns ==== | ||
Thermal burn injuries '''are caused by exposure to an external heat source or hot liquids'''. An external heat source can be a hot solid object or even a cold object. Scalds are caused by wet | Thermal burn injuries '''are caused by exposure to an external heat source or hot liquids'''. An external heat source can be a hot, solid object or even a cold object. Scalds are caused by something wet, such as hot water, steam from hot water or cold water. The types of thermal burns are: | ||
===== 1.1 Flame Burns ===== | ===== 1.1 Flame Burns ===== | ||
Flame burns '''are caused by | Flame burns '''are caused by exposure to an open fire'''. These burns are often associated with an inhalation injury and trauma. They tend to be mostly full-thickness burns. Flame burns are common in adults, but they are also associated with abuse in children, domestic violence and certain rituals.<ref name=":6">Hettiaratchy S, Dziewulski P. ABC of burns: pathophysiology and types of burns. BMJ. 2004;328(7453):1427-9.</ref> | ||
===== 1.2 Contact Burns ===== | ===== 1.2 Contact Burns ===== | ||
Contact burns '''are caused by contact with an extremely hot object or surface''', commonly | Contact burns '''are caused by contact with an extremely hot object or surface''', commonly stoves, heaters and irons. Contact burns tend to be deep dermal or full-thickness burns. They are often seen in people with epilepsy, those who misuse addictive substances or in older people after a loss of consciousness. | ||
===== 1.3 Frostbite or Ice Burns ===== | ===== 1.3 Frostbite or Ice Burns ===== | ||
Frostbite '''occurs when the skin is exposed to cold''', typically any temperature below -0.55C (31F), for an extended period of time. This causes the water in the cells of the skin and underlying tissue to freeze and crystalise. | Frostbite '''occurs when the skin is exposed to cold''', typically any temperature below -0.55C (31F), for an extended period of time. This causes the water in the cells of the skin and underlying tissue to freeze and crystalise. This crystallisation causes direct cellular injury.<ref>Nguyen, C. M., Chandler, R., Ratanshi, I. & Logsetty, S. In: Jeschke, MG, Kamolz LP, Sjöberg F. & Wolf SE. editor. Handbook of Burns Vol. 1. Springer, 2020:p529–547.</ref> Indirect injury occurs when the tissue becomes ischaemic. Frostbite can affect any part of the body, but the extremities, such as the hands, feet, ears, nose and lips, are most likely to be affected. If frostbite penetrates the deeper skin layers, impacting tissue and bone, it can cause permanent damage. | ||
An ice | An ice burn (also known as a snow burn) is '''caused by ice or a frozen object coming into contact with the skin for an extended period of time'''. Prolonged exposure to freezing temperatures, snow, or high-velocity winds can increase the chance of this type of burn injury. Ice burns can also be caused in the clinical setting by applying ice or cold packs directly against the skin when treating an injury or sore muscles. | ||
===== 1.4 Scalds ===== | ===== 1.4 Scalds ===== | ||
Scalds '''are caused by hot liquids''' | Scalds '''are caused by hot liquids''', such as boiling water and cooking oil coming into direct contact with the skin. Common mechanisms of injury include spilling of a hot drink or cooking oil, or being exposed to hot bath water. Scalds tend to cause superficial to superficial partial burns. Scald burns cause about 70% of burns in children. They often occur in older adults as well.<ref name=":6" /> This type of injury can be a sign of abuse and should be assessed accordingly. | ||
===== 1.5 Friction Burn ===== | |||
A friction burn is '''an abrasion injury that occurs when the skin rubs against another surface'''. A friction burn is not a true burn. However, because friction can generate heat, in extreme cases, a patient can present with burns to the outer layer of the skin. Common causes are rope burn, rug burn, chafing or skinning, or "road rash" from fallen cyclists or motorcycle accidents. | |||
==== 2. Electrical Burns ==== | ==== 2. Electrical Burns ==== | ||
An electrical burn is '''an injury caused by heat produced when an electrical current passes through | An electrical burn is '''an injury caused by heat, which is produced when an electrical current passes through the body'''. This can cause deep tissue injuries. Injury severity depends on many factors, including the pathway of the current, the resistance of the current in the tissues, and the strength and duration of the flow. AC (Alternating Current) and DC (Direct Current) are both potentially lethal,<ref>Dalziel CF. [https://staff.mq.edu.au/intranet/science-and-engineering/people-and-processes/research-and-laboratory-health-and-safety/documents/1956_Dalziel_Effects_of_Electric_Shock_on_Man-IRE-TransMedElec-PGME-5-P44.pdf Effects of electric shock on man.] IRE Transactions on Medical Electronics. 1956 Jul:44-62.</ref> but there are differences in presentation. A DC current can cause a single strong contraction which will often expel the individual from the source, for example, touching a car battery. An AC current injury is often of a lower frequency and the patient is often unable to let go. AC injuries are more common as these are found in most home power sockets.<ref>Bounds EJ, West B, Kok SJ. [https://www.ncbi.nlm.nih.gov/books/NBK519514/ Electrical burns].2022</ref><ref>Nowak K, Paduszyński K. [https://yadda.icm.edu.pl/baztech/element/bwmeta1.element.baztech-a074bb4c-3808-4547-9029-df0d538f02be/c/4-Nowak-Paduszynski_analiza_elektryka_2018.pdf Analysis of factors and hazards associated with electric shock]. Prace Naukowe Politechniki Śląskiej. Elektryka. 2018.</ref>There will be an entry and exit wound. The amount of internal damage depends on the pathway taken by the electrical current as it passes through the body. | ||
Electrical burns are often associated with [[Cardiac Arrest|cardiac arrest]], [[Ventricular Fibrillation|ventricular fibrillation]], and tetanic muscle contractions.<ref name=":5" /> | |||
For more information, please see [https://www.brighthubengineering.com/power-plants/89792-ac-and-dc-shock-comparison/#effects-of-an-ac-or-dc-currents-on-the-human-body AC and DC Electric Shock Effects Compared] | For more information, please see [https://www.brighthubengineering.com/power-plants/89792-ac-and-dc-shock-comparison/#effects-of-an-ac-or-dc-currents-on-the-human-body AC and DC Electric Shock Effects Compared] | ||
==== 3. Chemical Burns ==== | ==== 3. Chemical Burns ==== | ||
Chemical burns or caustic burns '''are injuries | Chemical burns or caustic burns '''are injuries that are caused by the skin coming into direct contact with a chemical agent'''.<ref name=":5" /> These can be strong acids, alkaline, or organic compounds. Chemical compounds can have different effects on human tissue depending on the following: | ||
* The strength or concentration of the chemical | * The strength or concentration of the chemical | ||
| Line 38: | Line 49: | ||
* Duration of exposure | * Duration of exposure | ||
* Chemical process | * Chemical process | ||
** Acids can causes "coagulation necrosis" of the tissue | ** Acids can causes "'''coagulation necrosis'''" of the tissue | ||
** Alkaline burns can cause "liquefaction necrosis" | *** Coagulation necrosis is when blood flow to a certain area stops or slows, causing ischaemia and subsequent cell death | ||
** Alkaline burns can cause "'''liquefaction necrosis'''" | |||
*** Liquefaction necrosis is a chemical process in which the necrotic tissue softens, becoming liquid/viscous. This can cause the burn to spread deeper than originally thought and should be monitored. | |||
==== 4. Radiation Burns ==== | ==== 4. Radiation Burns ==== | ||
A radiation burn '''is damage due to prolonged exposure to radiation'''. The most common type of radiation burn is sunburn caused by prolonged exposure to ultraviolet rays (UV). | A radiation burn '''is damage due to prolonged exposure to radio frequency energy or ionising radiation'''. The most common type of radiation burn is sunburn caused by prolonged exposure to ultraviolet rays (UV). Radiation burns can also occur with exposure to high power radio transmitters, repeated high exposure to X-rays for medical imaging, and interventional radiology procedures or radiotherapy for the treatment of cancer. Radiation burns resulting from therapeutic radiation are rare.<ref>Waghmare CM. [https://www.sciencedirect.com/science/article/pii/S0305417912003014 Radiation burn—from mechanism to management]. Burns. 2013 Mar 1;39(2):212-9.</ref> | ||
==== 5. Inhalation Burns/Injury ==== | ==== 5. Inhalation Burns/Injury ==== | ||
[[Inhalation Injury|Inhalation injury]] '''refers to pulmonary injury resulting from inhalation of smoke or chemical products of combustion'''.<ref name=":0">Dries DJ, Endorf FW. [https://link.springer.com/article/10.1186/1757-7241-21-31 Inhalation injury: epidemiology, pathology, treatment strategies.] Scandinavian journal of trauma, resuscitation and emergency medicine. 2013 Dec;21(1):1-5.</ref> Inhalation injury results in direct cellular damage, alterations in regional blood circulation and perfusion, obstruction of the airways, and the release of pro-inflammatory cytokine and toxin release.<ref>Reper P, Heijmans W. [https://www.sciencedirect.com/science/article/abs/pii/S0305417914001727 High-frequency percussive ventilation and initial biomarker levels of lung injury in patients with minor burns after smoke inhalation injury.] Burns. 2015; 41:65–70. [PubMed: 24986596]</ref><ref>Kadri SS, Miller AC, Hohmann S, Bonne S, Nielsen C, Wells C, Gruver C, Quraishi SA, Sun J, Cai R, Morris PE. [https://www.sciencedirect.com/science/article/abs/pii/S0012369216502566 Risk factors for in-hospital mortality in smoke inhalation-associated acute lung injury: data from 68 United States hospitals.] Chest. 2016 Dec 1;150(6):1260-8.</ref> Inhalation injuries also | [[Inhalation Injury|Inhalation injury]] '''refers to a pulmonary injury resulting from inhalation of smoke or chemical by-products of combustion'''.<ref name=":0">Dries DJ, Endorf FW. [https://link.springer.com/article/10.1186/1757-7241-21-31 Inhalation injury: epidemiology, pathology, treatment strategies.] Scandinavian journal of trauma, resuscitation and emergency medicine. 2013 Dec;21(1):1-5.</ref> Inhalation injury results in direct cellular damage, alterations in regional blood circulation and perfusion, obstruction of the airways, and the release of pro-inflammatory cytokine and toxin release.<ref>Reper P, Heijmans W. [https://www.sciencedirect.com/science/article/abs/pii/S0305417914001727 High-frequency percussive ventilation and initial biomarker levels of lung injury in patients with minor burns after smoke inhalation injury.] Burns. 2015; 41:65–70. [PubMed: 24986596]</ref><ref>Kadri SS, Miller AC, Hohmann S, Bonne S, Nielsen C, Wells C, Gruver C, Quraishi SA, Sun J, Cai R, Morris PE. [https://www.sciencedirect.com/science/article/abs/pii/S0012369216502566 Risk factors for in-hospital mortality in smoke inhalation-associated acute lung injury: data from 68 United States hospitals.] Chest. 2016 Dec 1;150(6):1260-8.</ref> Inhalation injuries also affect mucociliary clearance and weaken the alveolar macrophages.<ref>Al Ashry HS, Mansour G, Kalil AC, Walters RW, Vivekanandan R. [https://www.sciencedirect.com/science/article/abs/pii/S030541791600084X Incidence of ventilator associated pneumonia in burn patients with inhalation injury treated with high frequency percussive ventilation versus volume control ventilation: A systematic review.] Burns. 2016 Sep 1;42(6):1193-200.</ref> This injury can be split into three categories: | ||
===== '''5.1 Heat Injury to the Upper Airway''' ===== | ===== '''5.1 Heat Injury to the Upper Airway''' ===== | ||
The greatest complication of a heat injury to the upper airway is | The greatest complication of a heat injury to the upper airway is obstruction due to extensive swelling of the tongue, epiglottis, and aryepiglottic folds. Heat injuries do not commonly extend into the lower airway. Oedema/swelling can take a several hours to develop. Regular reassessment of a patient's airways is recommended as the presentation may change after the initial evaluation as fluid resuscitation commences. | ||
===== '''5.2 Chemical Injury to the Lower Airways''' ===== | ===== '''5.2 Chemical Injury to the Lower Airways''' ===== | ||
Chemical combustion results in the creation of materials toxic to the respiratory tract. This may cause local irritation in the respiratory tract.<ref name=":0" /> | |||
Common | Common chemical irritants created by combustion include: | ||
* Smoke produces toxins that may damage both the airway epithelial cells and capillary endothelial cells which can cause acute respiratory distress syndrome<ref>Trunkey DD. [https://ohsu.pure.elsevier.com/en/publications/inhalation-injury-2 Inhalation injury]. Surgical Clinics of North America. 1978 Jan 1;58(6):1133-40.</ref><ref name=":1">McCall JE, Cahill TJ. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/jbcr/article-abstract/26/3/200/4733941&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9818607520447678033&ei=XFwxYpPGEYjwyAS2o4mYAw&scisig=AAGBfm0ZbJTyYToooBENNki7v7cGynFnag Respiratory care of the burn patient.] Journal of Burn Care & Rehabilitation. 2005 May 1;26(3):200-6</ref><ref>Shubert J, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK513261/ Inhalation injury]. 2018</ref> | * Smoke produces toxins that may damage both the airway epithelial cells and capillary endothelial cells which can cause '''acute respiratory distress syndrome'''<ref>Trunkey DD. [https://ohsu.pure.elsevier.com/en/publications/inhalation-injury-2 Inhalation injury]. Surgical Clinics of North America. 1978 Jan 1;58(6):1133-40.</ref><ref name=":1">McCall JE, Cahill TJ. [https://scholar.google.com/scholar_url?url=https://academic.oup.com/jbcr/article-abstract/26/3/200/4733941&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9818607520447678033&ei=XFwxYpPGEYjwyAS2o4mYAw&scisig=AAGBfm0ZbJTyYToooBENNki7v7cGynFnag Respiratory care of the burn patient.] Journal of Burn Care & Rehabilitation. 2005 May 1;26(3):200-6</ref><ref>Shubert J, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK513261/ Inhalation injury]. 2018</ref> | ||
* Burning rubber and plastic produces sulfur dioxide, nitrogen dioxide, ammonia and chlorine which | * Burning rubber and plastic produces sulfur dioxide, nitrogen dioxide, ammonia and chlorine, which '''affect the respiratory airways and alveoli''' | ||
* Burning laminated furniture may contain glues that | * Burning laminated furniture - this furniture may contain glues that release cyanide gas during combustion | ||
* Burning cotton or wool produces aldehydes | * Burning cotton or wool produces aldehydes that are toxic to the human body<ref>Ahmed Laskar A, Younus H. [https://pubmed.ncbi.nlm.nih.gov/30514131/ Aldehyde toxicity and metabolism: the role of aldehyde dehydrogenases in detoxification, drug resistance and carcinogenesis.] Drug metabolism reviews. 2019 Jan 2;51(1):42-64.</ref> | ||
For more information on chemical irritants causing acute inhalation injury: their effects and sources of exposure, please see [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261306/pdf/eajm-42-1-28.pdf Acute Inhalation Injury].<ref>Hasarı AI, Gorguner M, Akgun M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261306/pdf/eajm-42-1-28.pdf Acute inhalation injury.] EAJM. 2010;42:28-35.</ref> | |||
===== '''5.3 Systemic Toxicity due to Carbon Monoxide or Cyanide Exposure''' ===== | ===== '''5.3 Systemic Toxicity due to Carbon Monoxide or Cyanide Exposure''' ===== | ||
Carbon monoxide (CO) is produced during a fire | Carbon monoxide (CO) is produced during a fire when any carbon-based product is not completely burned. When inhaled, CO binds with haemoglobin in the blood stream and reduces oxygen delivery.<ref name=":3">Culnan DM, Craft-Coffman B, Bitz GH, Capek KD, Tu Y, Lineaweaver WC, Kuhlmann-Capek MJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5825244/ Carbon monoxide and cyanide poisoning in the burned pregnant patient: an indication for hyperbaric oxygen therapy.] Annals of plastic surgery. 2018 Mar;80(3 Suppl 2):S106.</ref> Diagnosis involves taking an accurate history, recording any changes in mental status, and the presence of high carboxyhaemoglobin levels. Occasionally, patients may require [[Ventilation and Weaning|mechanical ventilation]] and treatment of [[shock]]. | ||
Common symptoms can include:<ref>Weaver LK. [https://europepmc.org/article/med/32176957 Carbon monoxide poisoning.] Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc. 2020 Jan 1;47(1):151-69.</ref> | Common symptoms can include:<ref>Weaver LK. [https://europepmc.org/article/med/32176957 Carbon monoxide poisoning.] Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc. 2020 Jan 1;47(1):151-69.</ref> | ||
* Headaches | * [[Headaches and Dizziness|Headaches]] | ||
* Nausea and vomiting | * Nausea and vomiting | ||
* Dizziness | * Dizziness | ||
* Exhaustion | * Exhaustion | ||
* Changes in mental state | * Changes in mental state | ||
* Chest pain | * [[Angina|Chest pain]] | ||
* Difficulty breathing | * Difficulty breathing | ||
* Myocardial ischaemia | * Myocardial ischaemia | ||
* Poisoning can lead to a brain injury with associated neurological problems. Symptoms include: | * Poisoning can lead to a brain injury with associated neurological problems. Symptoms include: | ||
** Cognitive sequelae | ** Cognitive sequelae | ||
** Anxiety and depression | ** Anxiety and [[depression]] | ||
** Persistent headaches, dizziness | ** Persistent headaches, dizziness | ||
** Sleep problems | ** [[Sleep Deprivation and Sleep Disorders|Sleep problems]] | ||
** Motor weakness | ** Motor weakness | ||
** Vestibular and balance problems | ** [[Vestibular Pathologies|Vestibular]] and balance problems | ||
** Gaze abnormalities | ** Gaze abnormalities | ||
** Peripheral neuropathies | ** Peripheral neuropathies | ||
** Hearing loss | ** Hearing loss | ||
** Tinnitus | ** [[Tinnitus]] | ||
** Parkinsonian-like symptoms | ** [[Parkinson's - Clinical Presentation|Parkinsonian-like symptoms]] | ||
Cyanide is often a byproduct of burning household materials. Cyanide intoxication | Cyanide is often a byproduct of burning household materials. Cyanide intoxication often occurs in conjunction with a CO inhalation injury. Cyanide intoxication lowers the lethal threshold of both cyanide and CO.<ref>Culnan DM, Craft-Coffman B, Bitz GH, Capek KD, Tu Y, Lineaweaver WC, Kuhlmann-Capek MJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5825244/ Carbon monoxide and cyanide poisoning in the burned pregnant patient: an indication for hyperbaric oxygen therapy.] Annals of plastic surgery. 2018 Mar;80(3 Suppl 2):S106.</ref> Diagnosis requires an accurate history, recording changes in mental status, carboxyhaemoglobin concentrations higher than 10%<ref>Moore SJ, Ho K, Hume AS. [https://scholar.google.com/scholar_url?url=https://www.sciencedirect.com/science/article/pii/0041008X9190004X&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=10620535349627570624&ei=0lwxYvbHGdCsywTntpO4CQ&scisig=AAGBfm1BvwRx1KTnOzW50DumOyrneuO4Lg Severe hypoxia produced by concomitant intoxication with sublethal doses of carbon monoxide and cyanide.] Toxicology and applied pharmacology. 1991 Jul 1;109(3):412-20.</ref><ref name=":2">Traber DL, Linares HA, Herndon DN, Prien T. [https://www.sciencedirect.com/science/article/pii/0305417988900034 The pathophysiology of inhalation injury—a review.] Burns. 1988 Oct 1;14(5):357-64.</ref><ref name=":1" /> and high lactate levels.<ref name=":3" /> | ||
For more information, please see [[Inhalation Injury]]. | |||
==== | == Burn Wound Classification == | ||
Burn injuries should be classified according to their severity, i.e. their depth and size.<ref name=":5" /> The characteristics of a burn injury can vary in terms of the amount of pain and colour of burn, depending on its depth. Always be on the look out for signs of inhalation burns, which are common in burns around the mouth or nose. Burns may have many complications and can cause shortness of breath, hoarseness of the voice, and stridor (noisy breathing due to airflow obstruction) or wheezing. Common symptoms are itchiness (a sign of healing), and numbness or tingling following an electrical injury. Burns can have a significant impact on an individual's mental health and this should always be taken into consideration. | |||
For more information on managing and assessing a patient's mental health following a burn injury or other trauma, please read [[The Stress Response Following Serious Injury or Illness: A Biopsychosocial Approach|this article]]. | |||
==== Classification by Depth ==== | ==== Classification by Depth ==== | ||
| Line 151: | Line 117: | ||
|'''Prognosis and Complications''' | |'''Prognosis and Complications''' | ||
|- | |- | ||
| | |'''Superficial''' | ||
(formerly first-degree burn) | |||
|Epidermis | |Epidermis | ||
|Red | | | ||
Dry | * Red | ||
* Dry | |||
Pain | * Pain | ||
* No blisters | |||
No blisters | |Re-epithelialisation takes 2-5 days | ||
| | | | ||
|Heals well | * Heals well | ||
* Repeated sunburns increase the risk of skin cancer later in life | |||
|- | |- | ||
| | |'''Superficial Partial Thickness''' | ||
|Epidermis and | (formerly second-degree burn) | ||
|Redness with a clear blister | |Epidermis and extends into the superficial dermis | ||
Generally moist | | | ||
* Redness with a clear blister | |||
Very painful | * Blanches with pressure, but shows rapid capillary refill when released | ||
| | * Generally moist | ||
| | * Very painful | ||
* Hair attachments are intact | |||
* Wound bed pink to red | |||
|Re-epithelialisation takes 1-2 weeks | |||
| | |||
* Low risk of infection unless patient is compromised | |||
* No scarring typically | |||
* Oedema is common | |||
|- | |- | ||
| | |'''Deep Partial Thickness''' | ||
(formerly deep second-degree burn) | |||
|Extends into deep (reticular) dermis | |Extends into deep (reticular) dermis | ||
| | |||
* Appears yellow or white. | |||
Less blanching than superficial. | * Less blanching than superficial. Sluggish capillary refill indicates vascular damage | ||
* Hair attachments are intact | |||
* Pain is often absent at this depth but is variable | |||
* Blisters are uncommon | |||
* Often moist and waxy | |||
* Wound bed shades of red, yellow, white | |||
|Re-epithelialisation takes 2-5 weeks. | |||
Some require surgical closure | |||
| | |||
* Scarring, contractures (may require excision and skin grafting) | |||
* Oedema | |||
* Circumferential burns at risk for compartment syndrome | |||
* Increased risk of infection due to depth and impaired blood flow | |||
|- | |||
|'''Full Thickness''' | |||
(formerly third-degree burn) | |||
|Extends through entire dermis and into the hypodermis | |||
| | |||
* Shades of brown, tan, waxy white, cherry red, sometimes with petechiae | |||
* Appearance can vary from waxy white, leathery grey or charred black. | |||
* Skin is dry, lacking in elasticity | |||
* No blanching | |||
* Not painful (nerve ending damage is common) | |||
* Stiff and white/brown | |||
* Initially painfree | |||
* Hair attachments absent | |||
* No blanch response indicates capillary destruction | |||
|Prolonged (months) and usually requires surgical interventions to ultimately close | |||
| | |||
* Increased risk of infection due to capillary destruction | |||
* Eschar, or the dead, denatured skin, is removed | |||
* Results in scarring and contractures | |||
|- | |||
|'''Subcutaneous''' | |||
(formerly fourth-degree burn) | |||
|Destruction of dermis and hypodermis, and into underlying fat, muscle and bone | |||
| | |||
* Charred with eschar | |||
* Dry | |||
* No elasticity | |||
* Initially painfree | |||
* Hair attachments absent | |||
* No blanch response indicates capillary destruction | |||
|Does not heal on its own | |||
Requires surgery and reconstruction | |||
| | |||
* Amputation | |||
* Significant functional impairment | |||
* Death | |||
|} | |||
''Information for table modified from: Merwarth, D. Management of Burn Wounds. Burn Wound Assessment Course. Plus. 2022.'' | |||
==== Total Body Surface Area ==== | |||
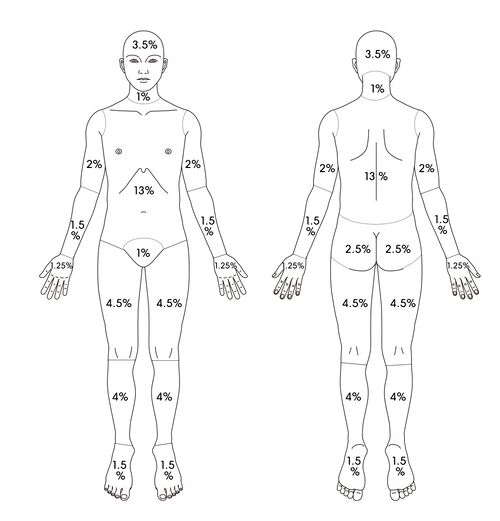
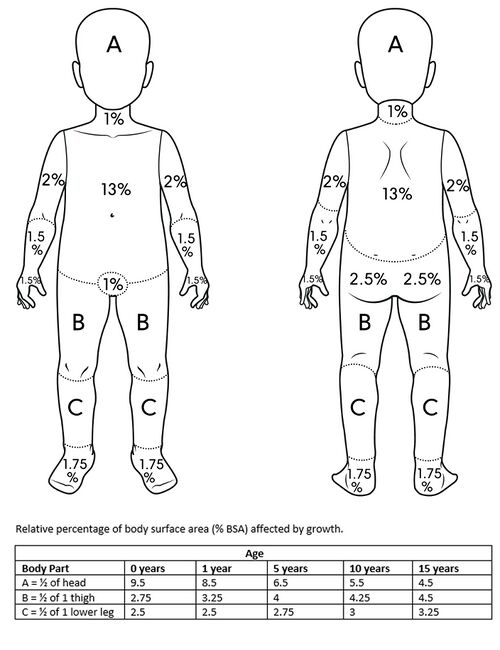
Total body surface area is an important figure when applying the Parkland Burn Formula. This formula is the most widely used formula to estimate the fluid resuscitation required by a patient with a burn wound upon on hospital admission. It is usually determined within the first 24 hours of admission. | |||
When applying this formula, the first step is to calculate the percentage of body surface area (BSA) damaged. This is commonly estimated using the "Wallace Rule of Nines" in adults<ref>Bereda G. [http://cmhrj.com/index.php/cmhrj/article/view/47 Burn Classifications with Its Treatment and Parkland Formula Fluid Resuscitation for Burn Management: Perspectives.] Clinical Medicine And Health Research Journal. 2022 May 12;2(3):136-41.</ref> and the Lund-Browder Method in children. The Lund-Browder Method uses different percentages to the Wallace Rule of Nines as children have a greater percentage surface area of their head and neck compared to an adult. | |||
The Parkland Burn Formula recommends 4 milliliters per kilogram of body weight in adults (3 milliliters per kilogram in children) per percentage burn of total body surface area (%TBSA) of crystalloid solution over the first 24 hours of care.<ref>Mehta M, Tudor GJ. [https://europepmc.org/article/NBK/nbk537190 Parkland formula]. 2019</ref><blockquote>4 mL/kg/%TBSA (3 mL/kg/%TBSA in children) = total amount of crystalloid fluid during first 24 hours</blockquote>The latest research has indicated that while this method is still used, fluid levels should be constantly monitored, while assessing the urine output,<ref>Ahmed FE, Sayed AG, Gad AM, Saleh DM, Elbadawy AM. [https://journals.ekb.eg/article_237338_719deabff050284526195f63d0c8ffae.pdf A Model for Validation of Parkland Formula for Resuscitation of Major Burn in Pediatrics.] The Egyptian Journal of Plastic and Reconstructive Surgery. 2022 Apr 1;46(2):155-8.</ref> to prevent over-resuscitation or under-resuscitation.<ref>Ete G, Chaturvedi G, Barreto E, Paul M K. [https://medcentral.net/doi/full/10.1016/j.cjtee.2019.01.006 Effectiveness of Parkland formula in the estimation of resuscitation fluid volume in adult thermal burns.] Chinese Journal of Traumatology. 2019 Apr 1;22(02):113-6.</ref> | |||
==== Calculation of Percentage Burn of Total Body Surface Area ==== | |||
# The Rule of Nine | |||
# Lund-Browder Method | |||
# Palmer Method | |||
===== The Rule of Nine and Lund-Browder Method Percentages ===== | |||
When using these methods, it is important to note that there are discrepancies in the percentage assigned to each area. Initially, all areas in the Rule of Nines were assigned 9%. This has evolved over the years and there has been an attempt to break down areas to get a more accurate estimate. Always remember that the team working with the patient must agree on which method everyone will use and, once agreed upon, this should be used throughout treatment. It is also important to note that these methods give an estimate for the Fluid Resuscitation calculation. Fluid Resuscitation will need to be closely monitored and adjusted by the dietitian. | |||
<div class="row"> | |||
|- | <div class="col-md-6">[[File:Rule of Nines - Adapted Shutterstock Image - ID 192650330-2.jpg|thumb|Rule of Nines|521x521px]]</div> | ||
| | <div class="col-md-6">[[File:Lund-Browder Chart - Paediatric - Adapted Shutterstock Image - ID 1968844102.jpg|thumb|650x650px|Lund-Browder Method]]</div> | ||
| | </div> | ||
| | |||
Please find blank copies of Burn Wound Assessment sheets below: | |||
* {{pdf|Burn Wound Assessment Sheet - Adult.pdf|Burn Wound Assessment Sheet - Adult}} | |||
* {{pdf|Burn Wound Assessment Sheet - Paediatric.pdf|Burn Wound Assessment Sheet - Paediatric}} | |||
{{#ev:youtube|2OWLc714x4U|300}}<ref> | |||
Medical Centric. What is Wallace rule of nines?. Available from: https://www.youtube.com/watch?v=2OWLc714x4U [last accessed 7/10/2022]</ref> | |||
===== Palmar Surface Method ===== | ===== Palmar Surface Method ===== | ||
The "Rule of Palm" or Palmar Surface Method can be used to estimate body surface area of a burn. This rule indicates that the palm of the patient, with the exclusion of the fingers and wrist, is approximately 1% of the | The "Rule of Palm" or Palmar Surface Method can be used to estimate body surface area of a burn. This rule indicates that the palm of the patient, with the exclusion of the fingers and wrist, is approximately 1% of the patient's body surface area. When a quick estimate is required, the percentage body surface area will be the number of the patient's own palm it would take to cover their injury. It is important to use the patient's palm and not the provider's palm. | ||
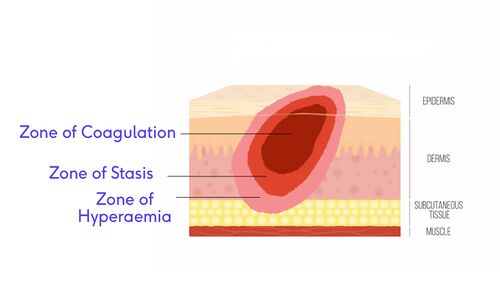
== Jackson's Burn Wound Model == | |||
== | Jackson's Burn Wound Model is a model used to understand the pathophysiology of a burn would. This model divides the wound into three zones. | ||
* '''<u>Zone of | * '''<u>Zone of Coagulation:</u>''' This is the area in the central part of the injury. This part of the burn experiences the greatest tissue damage.<ref name=":7" /> | ||
* '''<u>Zone of | * '''<u>Zone of Stasis or Zone of Ischaemia:</u>''' This area is adjacent to the zone of coagulation and as the name suggests, it is a zone in which the there is slowing of circulating blood due to the damage. This zone can usually be saved with the correct wound care.<ref name=":7" /> | ||
* '''<u>Zone of Hyperaemia:</u>''' This zone is circumferential and is characterised by superficial and superficial partial thickness burns and has a robust capillary refill. This is an area of increased circulation due to vasodilators, such as histamine, that are released in response to the burn injury. This tissue has a good recovery rate, as long as there are no complications, such as severe sepsis or prolonged hypo-perfusion.<ref name=":7" /> | |||
[[File:Jackson's Burn Model Adapted Shutterstock Image ID 686822944.jpg|500x500px|center|frameless]] | |||
For more information please see this article: [https://www.researchgate.net/profile/Morteza-Abazari-3/publication/342114619_A_Systematic_Review_on_Classification_Identification_and_Healing_Process_of_Burn_Wound_Healing/links/60269dcd92851c4ed56a85c1/A-Systematic-Review-on-Classification-Identification-and-Healing-Process-of-Burn-Wound-Healing.pdf A Systematic Review on Classification Identification and Healing Process of Burn Wound Healing]<ref name=":7">Abazari M, Ghaffari A, Rashidzadeh H, Badeleh SM, Maleki Y. [https://www.researchgate.net/profile/Morteza-Abazari-3/publication/342114619_A_Systematic_Review_on_Classification_Identification_and_Healing_Process_of_Burn_Wound_Healing/links/60269dcd92851c4ed56a85c1/A-Systematic-Review-on-Classification-Identification-and-Healing-Process-of-Burn-Wound-Healing.pdf A systematic review on classification, identification, and healing process of burn wound healing.] The International Journal of Lower Extremity Wounds. 2022 Mar;21(1):18-30.</ref> | |||
==Summary of the Pathophysiology of Burns== | |||
Please watch the video below for a summary of the pathophysiology of burns:<ref>Amando Hasudungan. Burns - Pathophysiology Available from: https://www.youtube.com/watch?v=Jaw8AKKVFRI</ref>{{#ev:youtube|Jaw8AKKVFRI}} | |||
== References == | == References == | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Burns]] | [[Category:Burns]] | ||
<references /> | |||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Rehabilitation]] | |||
Latest revision as of 11:36, 23 October 2023
Top Contributors - Carin Hunter, Jess Bell, Stacy Schiurring, Kim Jackson and Nikhil Benhur Abburi
What is a Burn?[edit | edit source]
A burn is an injury to the skin or other organic tissue primarily caused by exposure to heat or other causative agents (radiation, electricity, chemicals).[1] It is the result of energy transfer to the body. According to the World Health Organization (WHO), it is a global public health problem, causing an estimated 180,000 deaths annually.[2] It is among the leading causes of disability in low and middle-income countries and almost two-thirds of burns occur in the WHO African and South-East Asia regions. Burn injuries occur in all genders, however females have slightly higher rates of death as compared to males. They also affect all age groups and are the fifth most common cause of non-fatal childhood injuries.[2]
Burn injuries do not only affect the skin. They can also affect tissue, organ and system networks (e.g. from smoke inhalation) and have psychological effects.
For a review of skin anatomy and physiology, please read this article.
For a list of wound care terminology, please see this article.
Types of Burn Injuries[edit | edit source]
1. Thermal Burns[edit | edit source]
Thermal burn injuries are caused by exposure to an external heat source or hot liquids. An external heat source can be a hot, solid object or even a cold object. Scalds are caused by something wet, such as hot water, steam from hot water or cold water. The types of thermal burns are:
1.1 Flame Burns[edit | edit source]
Flame burns are caused by exposure to an open fire. These burns are often associated with an inhalation injury and trauma. They tend to be mostly full-thickness burns. Flame burns are common in adults, but they are also associated with abuse in children, domestic violence and certain rituals.[3]
1.2 Contact Burns[edit | edit source]
Contact burns are caused by contact with an extremely hot object or surface, commonly stoves, heaters and irons. Contact burns tend to be deep dermal or full-thickness burns. They are often seen in people with epilepsy, those who misuse addictive substances or in older people after a loss of consciousness.
1.3 Frostbite or Ice Burns[edit | edit source]
Frostbite occurs when the skin is exposed to cold, typically any temperature below -0.55C (31F), for an extended period of time. This causes the water in the cells of the skin and underlying tissue to freeze and crystalise. This crystallisation causes direct cellular injury.[4] Indirect injury occurs when the tissue becomes ischaemic. Frostbite can affect any part of the body, but the extremities, such as the hands, feet, ears, nose and lips, are most likely to be affected. If frostbite penetrates the deeper skin layers, impacting tissue and bone, it can cause permanent damage.
An ice burn (also known as a snow burn) is caused by ice or a frozen object coming into contact with the skin for an extended period of time. Prolonged exposure to freezing temperatures, snow, or high-velocity winds can increase the chance of this type of burn injury. Ice burns can also be caused in the clinical setting by applying ice or cold packs directly against the skin when treating an injury or sore muscles.
1.4 Scalds[edit | edit source]
Scalds are caused by hot liquids, such as boiling water and cooking oil coming into direct contact with the skin. Common mechanisms of injury include spilling of a hot drink or cooking oil, or being exposed to hot bath water. Scalds tend to cause superficial to superficial partial burns. Scald burns cause about 70% of burns in children. They often occur in older adults as well.[3] This type of injury can be a sign of abuse and should be assessed accordingly.
1.5 Friction Burn[edit | edit source]
A friction burn is an abrasion injury that occurs when the skin rubs against another surface. A friction burn is not a true burn. However, because friction can generate heat, in extreme cases, a patient can present with burns to the outer layer of the skin. Common causes are rope burn, rug burn, chafing or skinning, or "road rash" from fallen cyclists or motorcycle accidents.
2. Electrical Burns[edit | edit source]
An electrical burn is an injury caused by heat, which is produced when an electrical current passes through the body. This can cause deep tissue injuries. Injury severity depends on many factors, including the pathway of the current, the resistance of the current in the tissues, and the strength and duration of the flow. AC (Alternating Current) and DC (Direct Current) are both potentially lethal,[5] but there are differences in presentation. A DC current can cause a single strong contraction which will often expel the individual from the source, for example, touching a car battery. An AC current injury is often of a lower frequency and the patient is often unable to let go. AC injuries are more common as these are found in most home power sockets.[6][7]There will be an entry and exit wound. The amount of internal damage depends on the pathway taken by the electrical current as it passes through the body.
Electrical burns are often associated with cardiac arrest, ventricular fibrillation, and tetanic muscle contractions.[1]
For more information, please see AC and DC Electric Shock Effects Compared
3. Chemical Burns[edit | edit source]
Chemical burns or caustic burns are injuries that are caused by the skin coming into direct contact with a chemical agent.[1] These can be strong acids, alkaline, or organic compounds. Chemical compounds can have different effects on human tissue depending on the following:
- The strength or concentration of the chemical
- The site of contact (eye, skin, mucous membrane)
- Ingestion or inhalation
- Skin integrity
- Volume of substance
- Duration of exposure
- Chemical process
- Acids can causes "coagulation necrosis" of the tissue
- Coagulation necrosis is when blood flow to a certain area stops or slows, causing ischaemia and subsequent cell death
- Alkaline burns can cause "liquefaction necrosis"
- Liquefaction necrosis is a chemical process in which the necrotic tissue softens, becoming liquid/viscous. This can cause the burn to spread deeper than originally thought and should be monitored.
- Acids can causes "coagulation necrosis" of the tissue
4. Radiation Burns[edit | edit source]
A radiation burn is damage due to prolonged exposure to radio frequency energy or ionising radiation. The most common type of radiation burn is sunburn caused by prolonged exposure to ultraviolet rays (UV). Radiation burns can also occur with exposure to high power radio transmitters, repeated high exposure to X-rays for medical imaging, and interventional radiology procedures or radiotherapy for the treatment of cancer. Radiation burns resulting from therapeutic radiation are rare.[8]
5. Inhalation Burns/Injury[edit | edit source]
Inhalation injury refers to a pulmonary injury resulting from inhalation of smoke or chemical by-products of combustion.[9] Inhalation injury results in direct cellular damage, alterations in regional blood circulation and perfusion, obstruction of the airways, and the release of pro-inflammatory cytokine and toxin release.[10][11] Inhalation injuries also affect mucociliary clearance and weaken the alveolar macrophages.[12] This injury can be split into three categories:
5.1 Heat Injury to the Upper Airway[edit | edit source]
The greatest complication of a heat injury to the upper airway is obstruction due to extensive swelling of the tongue, epiglottis, and aryepiglottic folds. Heat injuries do not commonly extend into the lower airway. Oedema/swelling can take a several hours to develop. Regular reassessment of a patient's airways is recommended as the presentation may change after the initial evaluation as fluid resuscitation commences.
5.2 Chemical Injury to the Lower Airways[edit | edit source]
Chemical combustion results in the creation of materials toxic to the respiratory tract. This may cause local irritation in the respiratory tract.[9]
Common chemical irritants created by combustion include:
- Smoke produces toxins that may damage both the airway epithelial cells and capillary endothelial cells which can cause acute respiratory distress syndrome[13][14][15]
- Burning rubber and plastic produces sulfur dioxide, nitrogen dioxide, ammonia and chlorine, which affect the respiratory airways and alveoli
- Burning laminated furniture - this furniture may contain glues that release cyanide gas during combustion
- Burning cotton or wool produces aldehydes that are toxic to the human body[16]
For more information on chemical irritants causing acute inhalation injury: their effects and sources of exposure, please see Acute Inhalation Injury.[17]
5.3 Systemic Toxicity due to Carbon Monoxide or Cyanide Exposure[edit | edit source]
Carbon monoxide (CO) is produced during a fire when any carbon-based product is not completely burned. When inhaled, CO binds with haemoglobin in the blood stream and reduces oxygen delivery.[18] Diagnosis involves taking an accurate history, recording any changes in mental status, and the presence of high carboxyhaemoglobin levels. Occasionally, patients may require mechanical ventilation and treatment of shock.
Common symptoms can include:[19]
- Headaches
- Nausea and vomiting
- Dizziness
- Exhaustion
- Changes in mental state
- Chest pain
- Difficulty breathing
- Myocardial ischaemia
- Poisoning can lead to a brain injury with associated neurological problems. Symptoms include:
- Cognitive sequelae
- Anxiety and depression
- Persistent headaches, dizziness
- Sleep problems
- Motor weakness
- Vestibular and balance problems
- Gaze abnormalities
- Peripheral neuropathies
- Hearing loss
- Tinnitus
- Parkinsonian-like symptoms
Cyanide is often a byproduct of burning household materials. Cyanide intoxication often occurs in conjunction with a CO inhalation injury. Cyanide intoxication lowers the lethal threshold of both cyanide and CO.[20] Diagnosis requires an accurate history, recording changes in mental status, carboxyhaemoglobin concentrations higher than 10%[21][22][14] and high lactate levels.[18]
For more information, please see Inhalation Injury.
Burn Wound Classification[edit | edit source]
Burn injuries should be classified according to their severity, i.e. their depth and size.[1] The characteristics of a burn injury can vary in terms of the amount of pain and colour of burn, depending on its depth. Always be on the look out for signs of inhalation burns, which are common in burns around the mouth or nose. Burns may have many complications and can cause shortness of breath, hoarseness of the voice, and stridor (noisy breathing due to airflow obstruction) or wheezing. Common symptoms are itchiness (a sign of healing), and numbness or tingling following an electrical injury. Burns can have a significant impact on an individual's mental health and this should always be taken into consideration.
For more information on managing and assessing a patient's mental health following a burn injury or other trauma, please read this article.
Classification by Depth[edit | edit source]
| Type | Layers Involved | Signs and Symptoms | Healing Time | Prognosis and Complications |
| Superficial
(formerly first-degree burn) |
Epidermis |
|
Re-epithelialisation takes 2-5 days |
|
| Superficial Partial Thickness
(formerly second-degree burn) |
Epidermis and extends into the superficial dermis |
|
Re-epithelialisation takes 1-2 weeks |
|
| Deep Partial Thickness
(formerly deep second-degree burn) |
Extends into deep (reticular) dermis |
|
Re-epithelialisation takes 2-5 weeks.
Some require surgical closure |
|
| Full Thickness
(formerly third-degree burn) |
Extends through entire dermis and into the hypodermis |
|
Prolonged (months) and usually requires surgical interventions to ultimately close |
|
| Subcutaneous
(formerly fourth-degree burn) |
Destruction of dermis and hypodermis, and into underlying fat, muscle and bone |
|
Does not heal on its own
Requires surgery and reconstruction |
|
Information for table modified from: Merwarth, D. Management of Burn Wounds. Burn Wound Assessment Course. Plus. 2022.
Total Body Surface Area[edit | edit source]
Total body surface area is an important figure when applying the Parkland Burn Formula. This formula is the most widely used formula to estimate the fluid resuscitation required by a patient with a burn wound upon on hospital admission. It is usually determined within the first 24 hours of admission.
When applying this formula, the first step is to calculate the percentage of body surface area (BSA) damaged. This is commonly estimated using the "Wallace Rule of Nines" in adults[23] and the Lund-Browder Method in children. The Lund-Browder Method uses different percentages to the Wallace Rule of Nines as children have a greater percentage surface area of their head and neck compared to an adult.
The Parkland Burn Formula recommends 4 milliliters per kilogram of body weight in adults (3 milliliters per kilogram in children) per percentage burn of total body surface area (%TBSA) of crystalloid solution over the first 24 hours of care.[24]
4 mL/kg/%TBSA (3 mL/kg/%TBSA in children) = total amount of crystalloid fluid during first 24 hours
The latest research has indicated that while this method is still used, fluid levels should be constantly monitored, while assessing the urine output,[25] to prevent over-resuscitation or under-resuscitation.[26]
Calculation of Percentage Burn of Total Body Surface Area[edit | edit source]
- The Rule of Nine
- Lund-Browder Method
- Palmer Method
The Rule of Nine and Lund-Browder Method Percentages[edit | edit source]
When using these methods, it is important to note that there are discrepancies in the percentage assigned to each area. Initially, all areas in the Rule of Nines were assigned 9%. This has evolved over the years and there has been an attempt to break down areas to get a more accurate estimate. Always remember that the team working with the patient must agree on which method everyone will use and, once agreed upon, this should be used throughout treatment. It is also important to note that these methods give an estimate for the Fluid Resuscitation calculation. Fluid Resuscitation will need to be closely monitored and adjusted by the dietitian.
Please find blank copies of Burn Wound Assessment sheets below:
Palmar Surface Method[edit | edit source]
The "Rule of Palm" or Palmar Surface Method can be used to estimate body surface area of a burn. This rule indicates that the palm of the patient, with the exclusion of the fingers and wrist, is approximately 1% of the patient's body surface area. When a quick estimate is required, the percentage body surface area will be the number of the patient's own palm it would take to cover their injury. It is important to use the patient's palm and not the provider's palm.
Jackson's Burn Wound Model[edit | edit source]
Jackson's Burn Wound Model is a model used to understand the pathophysiology of a burn would. This model divides the wound into three zones.
- Zone of Coagulation: This is the area in the central part of the injury. This part of the burn experiences the greatest tissue damage.[28]
- Zone of Stasis or Zone of Ischaemia: This area is adjacent to the zone of coagulation and as the name suggests, it is a zone in which the there is slowing of circulating blood due to the damage. This zone can usually be saved with the correct wound care.[28]
- Zone of Hyperaemia: This zone is circumferential and is characterised by superficial and superficial partial thickness burns and has a robust capillary refill. This is an area of increased circulation due to vasodilators, such as histamine, that are released in response to the burn injury. This tissue has a good recovery rate, as long as there are no complications, such as severe sepsis or prolonged hypo-perfusion.[28]
For more information please see this article: A Systematic Review on Classification Identification and Healing Process of Burn Wound Healing[28]
Summary of the Pathophysiology of Burns[edit | edit source]
Please watch the video below for a summary of the pathophysiology of burns:[29]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.
- ↑ 2.0 2.1 World Health Organization. Burns. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/burns [Accessed 29th May 2022].
- ↑ 3.0 3.1 Hettiaratchy S, Dziewulski P. ABC of burns: pathophysiology and types of burns. BMJ. 2004;328(7453):1427-9.
- ↑ Nguyen, C. M., Chandler, R., Ratanshi, I. & Logsetty, S. In: Jeschke, MG, Kamolz LP, Sjöberg F. & Wolf SE. editor. Handbook of Burns Vol. 1. Springer, 2020:p529–547.
- ↑ Dalziel CF. Effects of electric shock on man. IRE Transactions on Medical Electronics. 1956 Jul:44-62.
- ↑ Bounds EJ, West B, Kok SJ. Electrical burns.2022
- ↑ Nowak K, Paduszyński K. Analysis of factors and hazards associated with electric shock. Prace Naukowe Politechniki Śląskiej. Elektryka. 2018.
- ↑ Waghmare CM. Radiation burn—from mechanism to management. Burns. 2013 Mar 1;39(2):212-9.
- ↑ 9.0 9.1 Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scandinavian journal of trauma, resuscitation and emergency medicine. 2013 Dec;21(1):1-5.
- ↑ Reper P, Heijmans W. High-frequency percussive ventilation and initial biomarker levels of lung injury in patients with minor burns after smoke inhalation injury. Burns. 2015; 41:65–70. [PubMed: 24986596]
- ↑ Kadri SS, Miller AC, Hohmann S, Bonne S, Nielsen C, Wells C, Gruver C, Quraishi SA, Sun J, Cai R, Morris PE. Risk factors for in-hospital mortality in smoke inhalation-associated acute lung injury: data from 68 United States hospitals. Chest. 2016 Dec 1;150(6):1260-8.
- ↑ Al Ashry HS, Mansour G, Kalil AC, Walters RW, Vivekanandan R. Incidence of ventilator associated pneumonia in burn patients with inhalation injury treated with high frequency percussive ventilation versus volume control ventilation: A systematic review. Burns. 2016 Sep 1;42(6):1193-200.
- ↑ Trunkey DD. Inhalation injury. Surgical Clinics of North America. 1978 Jan 1;58(6):1133-40.
- ↑ 14.0 14.1 McCall JE, Cahill TJ. Respiratory care of the burn patient. Journal of Burn Care & Rehabilitation. 2005 May 1;26(3):200-6
- ↑ Shubert J, Sharma S. Inhalation injury. 2018
- ↑ Ahmed Laskar A, Younus H. Aldehyde toxicity and metabolism: the role of aldehyde dehydrogenases in detoxification, drug resistance and carcinogenesis. Drug metabolism reviews. 2019 Jan 2;51(1):42-64.
- ↑ Hasarı AI, Gorguner M, Akgun M. Acute inhalation injury. EAJM. 2010;42:28-35.
- ↑ 18.0 18.1 Culnan DM, Craft-Coffman B, Bitz GH, Capek KD, Tu Y, Lineaweaver WC, Kuhlmann-Capek MJ. Carbon monoxide and cyanide poisoning in the burned pregnant patient: an indication for hyperbaric oxygen therapy. Annals of plastic surgery. 2018 Mar;80(3 Suppl 2):S106.
- ↑ Weaver LK. Carbon monoxide poisoning. Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc. 2020 Jan 1;47(1):151-69.
- ↑ Culnan DM, Craft-Coffman B, Bitz GH, Capek KD, Tu Y, Lineaweaver WC, Kuhlmann-Capek MJ. Carbon monoxide and cyanide poisoning in the burned pregnant patient: an indication for hyperbaric oxygen therapy. Annals of plastic surgery. 2018 Mar;80(3 Suppl 2):S106.
- ↑ Moore SJ, Ho K, Hume AS. Severe hypoxia produced by concomitant intoxication with sublethal doses of carbon monoxide and cyanide. Toxicology and applied pharmacology. 1991 Jul 1;109(3):412-20.
- ↑ Traber DL, Linares HA, Herndon DN, Prien T. The pathophysiology of inhalation injury—a review. Burns. 1988 Oct 1;14(5):357-64.
- ↑ Bereda G. Burn Classifications with Its Treatment and Parkland Formula Fluid Resuscitation for Burn Management: Perspectives. Clinical Medicine And Health Research Journal. 2022 May 12;2(3):136-41.
- ↑ Mehta M, Tudor GJ. Parkland formula. 2019
- ↑ Ahmed FE, Sayed AG, Gad AM, Saleh DM, Elbadawy AM. A Model for Validation of Parkland Formula for Resuscitation of Major Burn in Pediatrics. The Egyptian Journal of Plastic and Reconstructive Surgery. 2022 Apr 1;46(2):155-8.
- ↑ Ete G, Chaturvedi G, Barreto E, Paul M K. Effectiveness of Parkland formula in the estimation of resuscitation fluid volume in adult thermal burns. Chinese Journal of Traumatology. 2019 Apr 1;22(02):113-6.
- ↑ Medical Centric. What is Wallace rule of nines?. Available from: https://www.youtube.com/watch?v=2OWLc714x4U [last accessed 7/10/2022]
- ↑ 28.0 28.1 28.2 28.3 Abazari M, Ghaffari A, Rashidzadeh H, Badeleh SM, Maleki Y. A systematic review on classification, identification, and healing process of burn wound healing. The International Journal of Lower Extremity Wounds. 2022 Mar;21(1):18-30.
- ↑ Amando Hasudungan. Burns - Pathophysiology Available from: https://www.youtube.com/watch?v=Jaw8AKKVFRI