Introduction to Benign Paroxysmal Positional Vertigo: Difference between revisions
No edit summary |
No edit summary |
||
| (28 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/bernard-tonks/ Bernard Tonks]<br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
<div class="editorbox"> '''Original Editor '''- [[User: | |||
== Introduction == | == Introduction == | ||
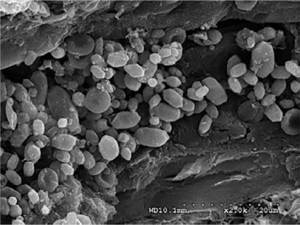
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo | [[File:Otoconia within the posterior canal endolymphatic duct.png|thumb|Figure 1. Otoconia within the posterior canal endolymphatic duct. ]] | ||
Benign paroxysmal positional vertigo (BPPV) is the most common cause of [[vertigo]] arising from peripheral [[Vestibular Pathologies|vestibular disorders]]. It accounts for 20 to 30 percent of all patients seen for vertigo in clinics that specialise in dizziness.<ref name=":0">von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2117684/ Epidemiology of benign paroxysmal positional vertigo: a population based study]. J Neurol Neurosurg Psychiatry. 2007;78(7):710-5. </ref> While the overall incidence of BPPV in the general population is around 2.5 percent,<ref name=":0" /> it is more common in older adults. Some studies show that 50 percent of [[Older People Introduction|older adults]] have BPPV.<ref name=":2">Balatsouras DG, Koukoutsis G, Fassolis A, Moukos A, Apris A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6223343/ Benign paroxysmal positional vertigo in the elderly: current insights]. ''Clin Interv Aging''. 2018;13:2251-66.</ref> | |||
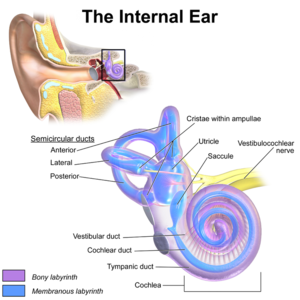
[[File:EarAnatomy InternalEar.png|thumb|Figure 2. Inner ear.]] | |||
BPPV is a [[Biomechanics|biomechanical]] problem that occurs when there is displacement of calcium-carbonate crystals or otoconia from the utricle into one of the three fluid-filled semicircular canals of the inner ear (see Figures 1 and 2).<ref name=":1" /><ref>Palmeri R, Kumar A. Benign Paroxysmal Positional Vertigo. [Updated 2020 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470308/ </ref> This causes the semi-circular canal (or canals) to be inappropriately excited, resulting in vertigo, nystagmus and occasionally nausea.<ref name=":1" /> For more information on the anatomy of the vestibular system, please click [[Introduction to Vestibular Rehabilitation|here]]. | |||
Symptoms tend to be provoked by head movements, such as:<ref name=":1">Tonks B. Benign Paroxysmal Positional Vertigo Course. Plus , 2021.</ref> | |||
Symptoms tend to be provoked by head movements, such as:<ref name=":1">Tonks B. Benign Paroxysmal Positional Vertigo Course. | |||
* Looking up | * Looking up | ||
* Lying down flat quickly | * Lying down to a flat position quickly | ||
* Bending forwards | * Bending forwards | ||
* Rolling in bed | * Rolling in bed | ||
BPPV is a | == Aetiology == | ||
It is not yet known what causes BPPV. The majority of cases are idiopathic<ref>You P, Instrum R, Parnes L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6383320/ Benign paroxysmal positional vertigo]. Laryngoscope investigative otolaryngology. 2019 Feb;4(1):116-23.</ref>, but it is more likely to occur in older adults.<ref name=":2" /> | |||
The two primary theories about its aetiology are that it is: | |||
# Related to ischaemia of the anterior vestibular artery and [[Cardiovascular Disease|cardiovascular disease]] primarily involving the posterior circulation<ref>Zhang D, Zhang S, Zhang H, Xu Y, Fu S, Yu M, Ji P. Evaluation of vertebrobasilar artery changes in patients with benign paroxysmal positional vertigo. Neuroreport. 2013;24(13):741-5. </ref> | |||
# Related to [[Vitamin D Deficiency|vitamin D deficiency]] and calcium metabolism (seasonal variations may be present)<ref>Jeong SH, Kim JS, Shin JW, Kim S, Lee H, Lee AY et al. [https://www.researchgate.net/publication/232699444_Decreased_serum_vitamin_D_in_idiopathic_benign_paroxysmal_positional_vertigo Decreased serum vitamin D in idiopathic benign paroxysmal positional vertigo]. J Neurol. 2013;260(3):832-8. </ref><ref name=":3">Chen J, Zhao W, Yue X, Zhang P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7324663/ Risk factors for the occurrence of benign paroxysmal positional vertigo: A systematic review and meta-analysis]. ''Front Neurol''. 2020;11:506. </ref> | |||
Predisposing factors include: | |||
* Head trauma in all age groups<ref name=":3" /><ref>Kim HJ, Park J, Kim JS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7684151/ Update on benign paroxysmal positional vertigo]. Journal of Neurology. 2021 May;268(5):1995-2000.</ref> | |||
** In a younger population, head trauma is a leading predisposing factor | |||
** The recurrence rate may be higher and treatment may not be as effective in this population<ref name=":1" /> | |||
* Surgical trauma to the inner ear<ref name=":4">Kansu L, Aydin E, Gulsahi K. Benign paroxysmal positional vertigo after nonotologic surgery: case series. J Maxillofac Oral Surg. 2015;14(Suppl 1):113-5.</ref> | |||
* Vestibular labyrinthitis / neuritis<ref name=":4" /> | |||
* [[Migraine Headache|Migraines]]<ref name=":0" /> | |||
* Ischaemia of the anterior vestibular artery and cardiovascular disease<ref name=":1" /><ref>Li S, Wang Z, Liu Y, Cao J, Zheng H, Jing Y et al. [https://journals.sagepub.com/doi/10.1177/0145561320943362?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Risk factors for the recurrence of benign paroxysmal positional vertigo: a systematic review and meta-analysis]. Ear Nose Throat J. 2020:145561320943362.</ref> | |||
It is estimated that 85 to 95 percent of BPPV occurs in the posterior canals. 5 to 15 percent occurs in the horizontal canals and 1 to 5 percent occurs in the anterior canals.<ref name=":5">Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T et al. [https://journals.sagepub.com/doi/10.1177/0194599816689667?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Clinical practice guideline: benign paroxysmal positional vertigo (update)]. Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1-S47.</ref> | |||
== Variants of BPPV == | |||
Two variants of BPPV can be present: | |||
# Cupulolithiasis | |||
# Canalithiasis | |||
=== Cupulolithiasis (i.e. ‘stuck crystals’) === | |||
* The debris adheres to the cupula of the affected canal, causing the cupula to be gravity sensitive | |||
* Changes in head position cause an inappropriate deflection of the cupula resulting in nystagmus, vertigo, and nausea | |||
* This is a relatively uncommon form of BPPV<ref name=":2" /> | |||
=== Canalithiasis (i.e. ‘free floating crystals’) === | |||
* This theory better explains the typical characteristics of BPPV | |||
* Otoconia are floating freely within the endolymph of the semi-circular canals | |||
* When the head is moved into the plane of the affected canal, the debris moves into the most dependent portion causing movement of the endolymph which deflects the cupula producing vertigo, nystagmus and nausea<ref name=":2" /> | |||
The key characteristics of these two variants of BPPV are summarised in Table 1. | |||
{| class="wikitable" | |||
|+ | |||
Table 1. Characteristics of BPPV variants.<ref name=":1" /> | |||
! | |||
!Canalithiasis | |||
!Cupulolithiasis | |||
|- | |||
|Latency of onset | |||
|>1 second before the onset of vertigo and nystagmus | |||
|No latency | |||
|- | |||
|Duration | |||
|Vertigo and nystagmus lasts < 60 seconds | |||
|Vertigo and nystagmus persist > 1minute | |||
|- | |||
|Direction of nystagmus | |||
|Characteristic nystagmus depending on which canal is involved | |||
|Characteristic nystagmus depending on which canal is involved | |||
|- | |||
|Fatiguability | |||
|Decreased intensity of vertigo and nystagmus with repeated movement of the patient in provoking positions | |||
|Decreased intensity of vertigo and nystagmus with repeated movement of the patient in provoking positions | |||
|} | |||
== Assessment == | |||
=== Assessing the Vertical Canals === | |||
==== Dix-Hallpike Test ==== | |||
[[File:Bigstock-Vector-Illustration-Of-DH-379339705.jpg|thumb|Figure 3. Dix-Hallpike test. ]] | |||
The Dix-Hallpike (DH) test is used to assess BPPV (primarily the vertical canals). This test enables the therapist to identify the side of the lesion and frequently the specific canal involved (see Figure 3).<ref name=":1" /> | |||
* Patient is seated with his / her head turned 45 degrees toward the test side | |||
* The therapist moves the patient as rapidly as is possible (considering safety) into a supine position with his / her head extended 30 degrees<ref name=":1" /> | |||
** NB there are variations in the literature over the degree of extension required. Some texts recommend 20 degrees, but according to Tonks, 30 degrees appears to give better results clinically<ref name=":1" /> | |||
* The therapist asks the patient to look at his / her nose and observes the patient's eyes for nystagmus, noting the direction of the movement, latency, and duration of nystagmus (see Table 2) | |||
* Wait until the nystagmus stops | |||
* Typically, the therapist will then proceed into treatment (see below) if indicated | |||
* Some therapists will, however, slowly sit the patient up in order to assess the other side, but nausea can be a problem | |||
Kaplan and colleagues have found that shaking the head during the DH increases the diagnostic yield. Patients who have a negative DH, but a positive result when head shaking is introduced may have otoconia that are not moving well through the affected canal.<ref>Kaplan DM, Slovik Y, Joshua BZ, Puterman M, Kraus M. Head shaking during Dix-Hallpike exam increases the diagnostic yield of posterior semicircular canal BPPV. Otol Neurotol. 2013;34(8):1444-7. </ref> | |||
If BPPV is likely present, but the DH is negative, this test can be repeated a couple of times to ensure that it is negative (in cases of “sticky canalithiasis”). <ref name=":1" /> | |||
It is important to try to assess the unaffected side first if possible. You can reason which side this might be based on the patient’s subjective report - i.e. the side she / he does not like to lie on. However, often the patient will not be able to tell you which side is worse.<ref name=":1" /> | |||
{{#ev:youtube|8RYB2QlO1N4}}<ref>BMJ Learning. Vertigo - Dix-Hallpike Manoeuvre from BMJ Learning. Available from: https://www.youtube.com/watch?v=8RYB2QlO1N4&t=1s [last accessed 13/6/2021[</ref> | |||
==== Side Lying Test ==== | |||
* Patient is seated with head turned 45 degrees away from the side to be tested | |||
* Patient is moved quickly into side-lying on the side opposite to the side that the head is turned | |||
* Therapist observes patient's eyes for nystagmus | |||
* Repeat the test with the head turned to the other side | |||
This test is a valid alternative that can be used when the DH is not considered a viable option (e.g. if there are range of motion limitations).<ref>Cohen HS. [https://journals.lww.com/otology-neurotology/Abstract/2004/03000/Side_Lying_as_an_Alternative_to_the_Dix_Hallpike.8.aspx Side-lying as an alternative to the Dix-Hallpike test of the posterior canal]. Otol Neurotol. 2004;25(2):130-4.</ref> | |||
{{#ev:youtube|fe63hTHR2cw}}<ref>Physical Therapy Nation. Sidelying Test for Posterior Canal BPPV. Available from: https://www.youtube.com/watch?v=fe63hTHR2cw [last accessed 13/6/2021]</ref> | |||
=== Assessing the Horizontal Canals === | |||
==== Head Roll Test ==== | |||
The head roll test can be used to assess the horizontal canals as it places these canals in the plane of gravity. It is considered a positive test when:<ref name=":1" /> | |||
* Horizontal nystagmus is provoked (see Table 2) | |||
* The patient reports vertigo when rolling to both the right and left sides | |||
To perform the test:<ref name=":1" /><ref name=":5" /> | |||
* Patient lies supine with his / her head elevated 20 degrees on a pillow | |||
* Quickly roll the head 90 degrees to one side (NB it is possible to do whole body rolls) | |||
* Observe the patient’s eyes for nystagmus and note the direction, latency, and duration. Also watch for direction changing nystagmus | |||
* Bring the patient’s head back to the neutral position in supine and wait until his / her signs and symptoms settle. Then roll the head quickly to the other side and observe | |||
* Both side lying positions will be positive for vertigo and nystagmus (same pattern) in horizontal semi-circular canal BPPV | |||
There are two types of nystagmus associated with the horizontal canals and they can be used to differentiate between cupulolithiasis and canalithiasis: <ref name=":5" /> | |||
* Geotropic (quick phase towards the earth) | |||
** Associated with canalithiasis | |||
*** Will have latency before onset and be shorter in duration | |||
** If geotropic nystagmus is provoked, assume that the most symptomatic side is the affected side and treat this side<ref name=":1" /> | |||
* Ageotropic (quick phase towards the ceiling) | |||
** Associated with cupulolithiasis | |||
*** Will have immediate onset and prolonged duration | |||
** If ageotropic nystagmus is provoked, assume the less symptomatic side is the affected side and treat this side<ref name=":1" /> | |||
{{#ev:youtube|ns8XZ4rKiJc}}<ref>EducatedPT. Supine Roll Test for Horizontal Canal BPPV. Available from: https://www.youtube.com/watch?v=ns8XZ4rKiJc [last accessed 13/6/2021]</ref> | |||
{| class="wikitable" | |||
|+Table 2. Identification of canal involvement - nystagmus | |||
!Involved Canal | |||
!Dix-Hallpike (DH) and Head Roll Test | |||
|- | |||
|Right posterior | |||
Right DH | |||
|Up beating, right torsion | |||
|- | |||
|Right anterior | |||
Left DH | |||
|Down beating, right torsion | |||
|- | |||
|Left anterior | |||
Right DH | |||
|Down beating, left torsion | |||
|- | |||
|Left posterior | |||
Left DH | |||
|Up beating, left torsion | |||
|- | |||
|Right / left horizontal | |||
canals | |||
Head roll test | |||
|Horizontal nystagmus, no torsion | |||
|} | |||
== Distinguishing Between a Central Nervous System Lesion and BPPV == | |||
It is possible to distinguish central nervous system lesions with BPPV (see Table 3). Lesions of central origin often present with:<ref name=":1" /><ref name=":5" /> | |||
* Atypical nystagmus (sustained down beating, no torsion) | |||
* No fatiguability of the response with repeated testing | |||
* No decrease in the nystagmus +/- vertigo with prolonged DH position | |||
* No reversal phenomenon (reversal of nystagmus) | |||
{| class="wikitable" | |||
| | |||
|Central | |||
| colspan="2" |Peripheral | |||
|- | |||
| | |||
| | |||
|Cupulolithiasis | |||
|Canalithiasis | |||
|- | |||
|Latency | |||
|No | |||
|No | |||
|Yes (>1 second) | |||
|- | |||
|Duration | |||
|Persistent | |||
|1-2 minutes | |||
|< 60 seconds | |||
|- | |||
|Direction | |||
|Uniplanar | |||
|Multiplanar | |||
|Multiplanar | |||
|- | |||
|Fatiguability | |||
|No | |||
|Yes | |||
|Yes | |||
|} | |||
Table 3. Distinguishing central nervous system lesion and BPPV | |||
== Treatment == | |||
=== Vertical Canal Canalithiasis === | |||
==== Epley Manoeuvre ==== | |||
The Epley manoeuvre (also known as canalith repositioning treatment) is used to treat posterior and anterior canal canalithiasis.<ref name=":1" /> | |||
The manoeuvre is performed as follows:<ref name=":1" /> | |||
* The patient is moved into DH on his / her affected side | |||
* The therapist rotates the patient’s head through 90 degrees to the opposite side; maintaining 30 degrees of extension | |||
* The patient is rolled onto the unaffected side with his / her head looking down | |||
* Maintaining head rotation, the patient gently sits up at side of bed | |||
* Each position is held until the vertigo and nystagmus has stopped and then for an additional 2 to 3 minutes | |||
{{#ev:youtube|jBzID5nVQjk}}<ref>BMJ Learning. Vertigo - Epley manoeuvre from BMJ Learning. Available from: https://www.youtube.com/watch?v=jBzID5nVQjk [last accessed 13/6/2021]</ref> | |||
==== Gans Manoeuvre ==== | |||
The Gans manoeuvre is a modified Epley manoeuvre. It is performed as follows (assuming the right side is affected:<ref name=":1" /> | |||
* Patient is positioned in side lying test position - i.e. sitting. | |||
* Patient turns head 45 degrees to the left | |||
* Patient lies down quickly onto his / her right side (no pillow), and holds this position for 2-3 minutes until the vertigo / nystagmus resolves | |||
* The patient then rolls over onto his / her left side, while maintaining the same head position | |||
* Wait 2-3 minutes as above | |||
* The patient sits up to complete the manoeuvre | |||
==== Efficacy of Treatment for Vertical Canal BPPV ==== | |||
===== Epley Manoeuvre ===== | |||
The Epley manoeuvre is a safe and effective treatment for posterior canal BPPV (the most common variant) It can be effective for anterior canal canalithiasis as well, but it is not effective for horizontal canal canalithiasis or anterior, posterior or horizontal cupulolithiasis.<ref name=":1" /> It has no serious side effects, but there is no evidence that it provides long-term resolution of symptoms and recurrence rates are high.<ref name=":6">Hilton MP, Pinder DK. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003162.pub3/epdf/standard The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo]. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162. </ref> The Gans manoeuvre has been shown to have similar outcomes as the Epley.<ref name=":6" /> | |||
* 93.5 percent of patients treated with an Epley manoeuvre had positive responses compared to 50 percent of the control group<ref name=":9">Wolf M, Hertanu T, Novikov I, Kronenberg J. [https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2273.1999.00202.x?sid=nlm%3Apubmed Epley's manoeuvre for benign paroxysmal positional vertigo: a prospective study]. Clin Otolaryngol Allied Sci. 1999;24(1):43-6. </ref> | |||
* Macias and colleagues looked at 259 BPPV patients who received the Epley manoeuvre:<ref>Macias JD, Lambert KM, Massingale S, Ellensohn A, Fritz JA. [https://onlinelibrary.wiley.com/doi/full/10.1097/00005537-200011000-00029 Variables affecting treatment in benign paroxysmal positional vertigo]. Laryngoscope. 2000;110(11):1921-4. </ref> | |||
** 74.8 percent required only one treatment | |||
** 19 percent required two treatments | |||
** 98.4 percent of patients were successfully treated after three sessions | |||
Epley manoeuvre head positions in patients with posterior canal BPPV:<ref>Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE. [https://jhu.pure.elsevier.com/en/publications/single-treatment-approaches-to-benign-paroxysmal-positional-verti-3 Single treatment approaches to benign paroxysmal positional vertigo]. Archives of Otolaryngology ‐ Head & Neck Surgery 1993;119(4):450‐4. </ref> | |||
* During an Epley manoeuvre, if the patient was returned to a sitting position without rolling over onto his / her side with the head down at 45 degrees, the remission rate was found to be 50 percent | |||
* This suggests that the last component of the Epley manoeuvre facilitates the movement of the debris into the common crus<ref name=":1" /> | |||
===== Gans Manoeuvre ===== | |||
The Gans manoeuvre was developed because certain aspects of other BPPV manoeuvres, such as hyperextension of the neck during the Epley, are contraindicated for patients with vertebrobasilar insufficiency, cervical spondylosis, back problems etc.<ref name=":7">Roberts RA, Gans RE, Montaudo RL. [https://pubmed.ncbi.nlm.nih.gov/16999254/ Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo]. J Am Acad Audiol. 2006;17(8):598-604. </ref> Roberts and colleagues assessed the efficacy of the Gans manoeuvre and found that:<ref name=":7" /> | |||
* On average, 1.25 treatments were needed to resolve the posterior semi-circular canal BPPV | |||
* Most patients (80.2%) were cleared with one treatment | |||
* 95.6 percent were cleared after two treatments | |||
* The Gans is, therefore, a good option for patients who cannot have the Epley or liberatory manoeuvres (see below) | |||
=== Horizontal Canal Canalithiasis Treatment === | |||
There are two key treatments for horizontal canal canalithiasis: | |||
# Forced prolonged positioning (i.e. 8 to 12 hours) lying on the unaffected side | |||
# Barbeque roll (also known as the Lempert roll) | |||
==== Barbeque Roll ==== | |||
To perform this canalith repositioning treatment:<ref name=":1" /> | |||
# The patient is positioned in supine with his / her head elevated 20 degrees and turned toward the affected side | |||
# The therapist slowly rolls the patient’s head away from the affected side in 90 degree increments until the head has moved through 360 degrees | |||
# Each position is maintained until the vertigo has stopped plus an additional 15 seconds | |||
# The patient should have no vertigo or nystagmus once they are prone | |||
NB usually whole body rolls are performed instead of just neck rotations | |||
{{#ev:youtube|ufD_tcSx5dQ}}<ref>Ascension Via Christi. Barbeque Roll Lempert maneuver. Available from: https://www.youtube.com/watch?v=ufD_tcSx5dQ [last accessed 13/6/2021]</ref> | |||
==== Efficacy of Treatment for Horizontal Canal Canalithiasis ==== | |||
Nuti and colleagues compared these two techniques for horizontal canal canalithiasis with an untreated control group.<ref name=":8">Nuti D, Agus G, Barbieri MT, Passali D. [https://www.tandfonline.com/doi/abs/10.1080/00016489850154559 The management of horizontal-canal paroxysmal positional vertigo]. Acta Otolaryngol. 1998;118(4):455-60. </ref> | |||
* Barbeque roll – patients were rotated around the longitudinal axis in 90 degree stages | |||
* Prolonged positioning – patients lay on their uninvolved side for prolonged periods | |||
Both treatments had similar remission rates:<ref name=":8" /> | |||
* 71 percent in the rolling group | |||
* 73 percent in the forced prolonged positioning treatment | |||
* 33 percent in the control group | |||
A more recent study by Wang and colleagues also supports the use of the barbeque roll.<ref>Wang YH, Chan CY, Liu QH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6572671/ Benign paroxsymal positional vertigo - recommendations for treatment in primary care]. Ther Clin Risk Manag. 2019;15:719-725.</ref> | |||
=== Vertical Canal Cupulolithiasis === | |||
==== Liberatory (Semont) Manoeuvre ==== | |||
To treat posterior canal BPPV using the liberatory (semont) manoeuvre:<ref name=":1" /><ref name=":5" /> | |||
* The patient sits with his / her legs over the side of the bed | |||
* The patient's head is turned 45 degrees toward the unaffected side | |||
* The therapist quickly moves the patient into side-lying on the affected side | |||
* This position is held for 5 minutes | |||
* The patient is then quickly moved all the way back up and then down to the opposite side-lying position, maintaining his / her head position | |||
* This position is held for 5 minutes | |||
* In this second position, nystagmus and vertigo typically appear. If they do not, the head is abruptly shaken once or twice to free the debris<ref name=":1" /> | |||
* The patient is slowly sat back up | |||
{{#ev:youtube|pK9qaprUU64}}<ref>EducatedPT. Liberatory (Semont) Maneuver for BPPV. Available from: https://www.youtube.com/watch?v=pK9qaprUU64 [last accessed 13/6/2021]</ref> | |||
To treat anterior canal BPPV with the liberatory (semont) manoeuvre, the manoeuvre is similar, but the patient’s head is turned to the '''affected''' side to begin:<ref name=":1" /> | |||
* Patient sits with legs over the side of the bed | |||
* Patient's head is turned 45 degrees towards the affected side | |||
* The therapist quickly moves the patient into side-lying on the affected side - essentially, the patient is lying on his / her affected canal | |||
* This position is held for 5 minutes | |||
* The patient is then quickly moved all the way back up and then down to the opposite side-lying position, maintaining his / her head position | |||
* This position is held for 5 minutes | |||
* In this second position, nystagmus and vertigo typically appear. If they do not, the patient’s head is abruptly shaken once or twice to free the debris | |||
* The patient is slowly sat back up | |||
==== Efficacy of the Liberatory Manoeuvre ==== | |||
Semont and colleagues found that in 711 patients with BPPV there was complete remission in 84 percent of patients after one treatment and 93 percent after a second procedure one week later.<ref>Parnes LS, Agrawal SK, Atlas J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC202288/ Diagnosis and management of benign paroxysmal positional vertigo (BPPV)]. CMAJ. 2003;169(7):681-93.</ref> | |||
Salvinilli and colleagues also found that the liberatory manoeuvre had good results. They found there was a remission rate of 92.5 percent with one manoeuvre while the untreated control group had a remission rate of 37.5 percent.<ref name=":10">Salvinelli F, Casale M, Trivelli M, D'Ascanio L, Firrisi L, Lamanna F et al. [https://pubmed.ncbi.nlm.nih.gov/12854277/ Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semont's maneuver and no treatment strategy]. Clin Ter. 2003;154(1):7-11.</ref> | |||
=== Horizontal Canal Cupulolithiasis === | |||
The modified semont manoeuvre can be used to treat horizontal canal cupulolithiasis.<ref name=":11">Casani AP, Vannucci G, Fattori B, Berrettini S. [https://onlinelibrary.wiley.com/doi/abs/10.1097/00005537-200201000-00030 The treatment of horizontal canal positional vertigo: our experience in 66 cases]. Laryngoscope. 2002;112(1):172-8.</ref> It is performed as follows:<ref name=":1" /> | |||
* The patient starts in sitting on a bed. Lie him / her quickly down into side-lying on the affected side (i.e. the less symptomatic side to the patient) | |||
* Immediately at this point, conduct a 45 degree rotation downward | |||
* This position is held for 2 to 3 minutes | |||
* The patient is then quickly returned to the sitting position | |||
This modified semont manoeuvre was found to result in resolution of symptoms for 77.8 percent of patients with horizontal canal cupulolithiasis after three sessions.<ref name=":1" /><ref name=":11" /> | |||
The efficacy of these treatments for BPPV are summarised in Table 4. | |||
{| class="wikitable" | |||
|+Table 4. Efficacy of Treatment for BPPV | |||
!BPPV variant | |||
!Efficacy | |||
- one treatment applied | |||
- outcome complete resolution | |||
|- | |||
|Anterior / posterior canal canalithiasis | |||
|Epley manoeuvre: 93.5 percent <ref name=":9" /> | |||
Gans manoeuvre: 80.2 percent<ref name=":7" /> | |||
|- | |||
|Horizontal canal canalithiasis | |||
|Barbeque roll: 71 percent<ref name=":8" /> | |||
|- | |||
|Anterior / posterior canal cupulolithiasis | |||
|Liberatory manoeuvre: 92.5 percent<ref name=":10" /> | |||
|- | |||
|Horizontal canal cupulolithiasis | |||
|Modified semont manoeuvre: 77.8 percent<ref name=":11" /> | |||
(3 applications) | |||
|} | |||
=== Brandt-Daroff Treatment: Home exercise program for BPPV === | |||
To perform these exercise programme, patients are instructed to:<ref name=":1" /> | |||
* Turn their head 45 degrees away from the affected side and lie quickly onto the affected side | |||
* Hold this position until vertigo stops (+ 30 seconds) | |||
* Then return to sitting position and hold for 30 seconds or until the vertigo stops | |||
* Repeat these steps on the opposite side | |||
* Repeat this sequence 10-20 times, three times per day | |||
NB patients are advised they can stop the exercise when they have two consecutive days with no symptoms or if there has been no improvement within 2 weeks. | |||
==== Effectiveness of the Brandt-Daroff Exercises ==== | |||
Brandt and Daroff studied the effectiveness of these exercises on a series of 67 patients with BPPV. They found that after 3 to 14 days of exercises, 98% of the subjects had no symptoms of BPPV.<ref>Brandt T, Daroff RB. [https://pubmed.ncbi.nlm.nih.gov/7396795/ Physical therapy for benign paroxysmal positional vertigo]. Arch Otolaryngol. 1980;106(8):484-5.</ref> More recent studies have also found these exercises to be effective.<ref>Cetin YS, Ozmen OA, Demir UL, Kasapoglu F, Basut O, Coskun H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6041543/ Comparison of the effectiveness of Brandt-Daroff Vestibular training and Epley Canalith repositioning maneuver in benign Paroxysmal positional vertigo long term result: A randomized prospective clinical trial]. Pak J Med Sci. 2018;34(3):558-63.</ref> | |||
Clinically, however, this exercise programme often requires a prolonged period of time for patients to experience an improvement in their symptoms.<ref name=":1" /> | |||
=== Relevance of Postural Restrictions for BPPV === | |||
Postural restrictions post-Epley manoeuvre did not improve the efficacy of treatment or diminish the recurrence rate. At present, it is not, therefore, advised to place postural restrictions on patients after an Epley manoeuvre.<ref>Casqueiro JC, Ayala A, Monedero G. [https://journals.lww.com/otology-neurotology/Abstract/2008/08000/No_More_Postural_Restrictions_in_Posterior_Canal.24.aspx No more postural restrictions in posterior canal benign paroxysmal positional vertigo]. Otol Neurotol. 2008;29(5):706-9. </ref><ref>Balikci HH, Ozbay I. [https://www.aurisnasuslarynx.com/article/S0385-8146(14)00090-X/fulltext Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo]. Auris Nasus Larynx. 2014;41(5):428-31.</ref> | |||
=== Daily Epley Manoeuvres and BPPV === | |||
A daily routine of self-canalith repositioning exercises does not affect the time to recurrence or the rate of recurrence of posterior canal BPPV.<ref>Helminski JO, Janssen I, Hain TC. [https://journals.lww.com/otology-neurotology/Abstract/2008/10000/Daily_Exercise_Does_Not_Prevent_Recurrence_of.18.aspx Daily exercise does not prevent recurrence of benign paroxysmal positional vertigo]. Otol Neurotol. 2008;29(7):976-81.</ref> Patients should not, therefore, do the Epley manoeuvre as a home exercise to prevent recurrence of BPPV. <ref name=":1" /> | |||
=== Sleep Position and Laterality of BPPV === | |||
It has been found that there is an association between the ear affected by BPPV and the preferred head-lying side during sleep onset. Moreover, there are higher recurrence rates of BPPV in patients who sleep on their affected side.<ref>Korres SG, Papadakis CE, Riga MG, Balatsouras DG, Dikeos DG, Soldatos CR. [https://www.cambridge.org/core/journals/journal-of-laryngology-and-otology/article/abs/sleep-position-and-laterality-of-benign-paroxysmal-positional-vertigo/C67EF40361267C028A307DD2DBD69C74 Sleep position and laterality of benign paroxysmal positional vertigo]. J Laryngol Otol. 2008;122(12):1295-8. </ref><ref>Shigeno K, Ogita H, Funabiki K. [https://content.iospress.com/articles/journal-of-vestibular-research/ves00457 Benign paroxysmal positional vertigo and head position during sleep]. J Vestib Res. 2012;22(4):197-203. </ref><ref>Li S, Tian L, Han Z, Wang J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867465/ Impact of postmaneuver sleep position on recurrence of benign paroxysmal positional vertigo]. PLoS One. 2013;8(12):e83566. </ref> Patients may, therefore, want to change or vary the side they sleep on sleep on if BPPV is recurring.<ref name=":1" /> | |||
== Canal Conversion == | |||
During treatment of posterior semi-circular canal BPPV, debris may move from the posterior canal to the horizontal canal (usually) or to the anterior canal (rarely – 2.9%).<ref>Park S, Kim BG, Kim SH, Chu H, Song MY, Kim M. [https://journals.lww.com/otology-neurotology/Abstract/2013/12000/Canal_Conversion_Between_Anterior_and_Posterior.31.aspx Canal conversion between anterior and posterior semicircular canal in benign paroxysmal positional vertigo]. Otol Neurotol. 2013;34(9):1725-8. </ref> | |||
This will be obvious when a DH retest results in dramatically different nystagmus patterns after an Epley manoeuvre has been performed. If this occurs, it is necessary to re-evaluate and treat the newly involved canal.<ref name=":1" /> The Epley manoeuvre may have a higher rate of conversion than the liberatory manoeuvre.<ref>Anagnostou E, Stamboulis E, Kararizou E. [https://link.springer.com/article/10.1007%2Fs00415-014-7290-2 Canal conversion after repositioning procedures: comparison of Semont and Epley maneuver]. J Neurol. 2014;261(5):866-9. </ref> | |||
== What Happens to the Otoconia? == | |||
A number of theories have been proposed to explain where the otoconia go after repositioning techniques, including:<ref name=":1" /> | |||
* They simply dissolve<ref>Parker DE, Covell WP, von Gierke HE. Exploration of vestibular damage in guinea pigs following mechanical stimulation. Acta Otolaryngol. 1968:Suppl 239:7+. </ref> | |||
* The ‘dark cells’ of the labyrinth, which are adjacent to the utricle and crista, reabsorb the displaced otoconia<ref>Lim DJ The development and structure of otoconia. In: I Friedman, J Ballantyne (eds). Ultrastructural Atlas of the Inner Ear. London: Butterworth, 1984. p. 245-69.</ref> | |||
* They stick back to the utricle<ref>Otsuka K, Suzuki M, Shimizu S, Konomi U, Inagaki T, Iimura Y et al. Model experiments of otoconia stability after canalith repositioning procedure of BPPV. Acta Otolaryngol. 2010 Jul;130(7):804-9.</ref> | |||
== Management Issues in BPPV == | |||
* BPPV is frequently considered a self-limiting disorder as the spontaneous remission rate can be as high as 50 percent | |||
* However, for many individuals it persists for years if not decades | |||
* Recurrence rate varies from 18 to 37 percent | |||
* Antivertiginous drugs are not helpful | |||
* Some patients may experience increased dizziness, nausea and imbalance for a day or two after treatment – possibly due to an autonomic dysfunction<ref>Kim HA, Lee H. [https://www.sciencedirect.com/science/article/abs/pii/S1388245713009917?via%3Dihub Autonomic dysfunction as a possible cause of residual dizziness after successful treatment in benign paroxysmal positional vertigo]. Clin Neurophysiol. 2014;125(3):608-14.</ref> | |||
* It is important to bring a patient back for re-evaluation, usually in 3 to 5 days if possible | |||
* Evaluate the patient's postural control, vestibular function and motion sensitivity | |||
* If the patient has a vestibular hypofunction and BPPV, treat the BPPV first | |||
* Be alert to central signs and symptoms<ref name=":1" /> | |||
== References == | |||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
[[Category:Neurology]] | [[Category:Neurology]] | ||
<references /> | |||
[[Category:Vestibular System]] | |||
Latest revision as of 20:46, 4 January 2023
Top Contributors - Jess Bell, Kim Jackson, Robin Tacchetti, Tarina van der Stockt, Rucha Gadgil and Lucinda hampton
Introduction[edit | edit source]
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo arising from peripheral vestibular disorders. It accounts for 20 to 30 percent of all patients seen for vertigo in clinics that specialise in dizziness.[1] While the overall incidence of BPPV in the general population is around 2.5 percent,[1] it is more common in older adults. Some studies show that 50 percent of older adults have BPPV.[2]
BPPV is a biomechanical problem that occurs when there is displacement of calcium-carbonate crystals or otoconia from the utricle into one of the three fluid-filled semicircular canals of the inner ear (see Figures 1 and 2).[3][4] This causes the semi-circular canal (or canals) to be inappropriately excited, resulting in vertigo, nystagmus and occasionally nausea.[3] For more information on the anatomy of the vestibular system, please click here.
Symptoms tend to be provoked by head movements, such as:[3]
- Looking up
- Lying down to a flat position quickly
- Bending forwards
- Rolling in bed
Aetiology[edit | edit source]
It is not yet known what causes BPPV. The majority of cases are idiopathic[5], but it is more likely to occur in older adults.[2]
The two primary theories about its aetiology are that it is:
- Related to ischaemia of the anterior vestibular artery and cardiovascular disease primarily involving the posterior circulation[6]
- Related to vitamin D deficiency and calcium metabolism (seasonal variations may be present)[7][8]
Predisposing factors include:
- Head trauma in all age groups[8][9]
- In a younger population, head trauma is a leading predisposing factor
- The recurrence rate may be higher and treatment may not be as effective in this population[3]
- Surgical trauma to the inner ear[10]
- Vestibular labyrinthitis / neuritis[10]
- Migraines[1]
- Ischaemia of the anterior vestibular artery and cardiovascular disease[3][11]
It is estimated that 85 to 95 percent of BPPV occurs in the posterior canals. 5 to 15 percent occurs in the horizontal canals and 1 to 5 percent occurs in the anterior canals.[12]
Variants of BPPV[edit | edit source]
Two variants of BPPV can be present:
- Cupulolithiasis
- Canalithiasis
Cupulolithiasis (i.e. ‘stuck crystals’)[edit | edit source]
- The debris adheres to the cupula of the affected canal, causing the cupula to be gravity sensitive
- Changes in head position cause an inappropriate deflection of the cupula resulting in nystagmus, vertigo, and nausea
- This is a relatively uncommon form of BPPV[2]
Canalithiasis (i.e. ‘free floating crystals’)[edit | edit source]
- This theory better explains the typical characteristics of BPPV
- Otoconia are floating freely within the endolymph of the semi-circular canals
- When the head is moved into the plane of the affected canal, the debris moves into the most dependent portion causing movement of the endolymph which deflects the cupula producing vertigo, nystagmus and nausea[2]
The key characteristics of these two variants of BPPV are summarised in Table 1.
| Canalithiasis | Cupulolithiasis | |
|---|---|---|
| Latency of onset | >1 second before the onset of vertigo and nystagmus | No latency |
| Duration | Vertigo and nystagmus lasts < 60 seconds | Vertigo and nystagmus persist > 1minute |
| Direction of nystagmus | Characteristic nystagmus depending on which canal is involved | Characteristic nystagmus depending on which canal is involved |
| Fatiguability | Decreased intensity of vertigo and nystagmus with repeated movement of the patient in provoking positions | Decreased intensity of vertigo and nystagmus with repeated movement of the patient in provoking positions |
Assessment[edit | edit source]
Assessing the Vertical Canals[edit | edit source]
Dix-Hallpike Test[edit | edit source]
The Dix-Hallpike (DH) test is used to assess BPPV (primarily the vertical canals). This test enables the therapist to identify the side of the lesion and frequently the specific canal involved (see Figure 3).[3]
- Patient is seated with his / her head turned 45 degrees toward the test side
- The therapist moves the patient as rapidly as is possible (considering safety) into a supine position with his / her head extended 30 degrees[3]
- NB there are variations in the literature over the degree of extension required. Some texts recommend 20 degrees, but according to Tonks, 30 degrees appears to give better results clinically[3]
- The therapist asks the patient to look at his / her nose and observes the patient's eyes for nystagmus, noting the direction of the movement, latency, and duration of nystagmus (see Table 2)
- Wait until the nystagmus stops
- Typically, the therapist will then proceed into treatment (see below) if indicated
- Some therapists will, however, slowly sit the patient up in order to assess the other side, but nausea can be a problem
Kaplan and colleagues have found that shaking the head during the DH increases the diagnostic yield. Patients who have a negative DH, but a positive result when head shaking is introduced may have otoconia that are not moving well through the affected canal.[13]
If BPPV is likely present, but the DH is negative, this test can be repeated a couple of times to ensure that it is negative (in cases of “sticky canalithiasis”). [3]
It is important to try to assess the unaffected side first if possible. You can reason which side this might be based on the patient’s subjective report - i.e. the side she / he does not like to lie on. However, often the patient will not be able to tell you which side is worse.[3]
Side Lying Test[edit | edit source]
- Patient is seated with head turned 45 degrees away from the side to be tested
- Patient is moved quickly into side-lying on the side opposite to the side that the head is turned
- Therapist observes patient's eyes for nystagmus
- Repeat the test with the head turned to the other side
This test is a valid alternative that can be used when the DH is not considered a viable option (e.g. if there are range of motion limitations).[15]
Assessing the Horizontal Canals[edit | edit source]
Head Roll Test[edit | edit source]
The head roll test can be used to assess the horizontal canals as it places these canals in the plane of gravity. It is considered a positive test when:[3]
- Horizontal nystagmus is provoked (see Table 2)
- The patient reports vertigo when rolling to both the right and left sides
- Patient lies supine with his / her head elevated 20 degrees on a pillow
- Quickly roll the head 90 degrees to one side (NB it is possible to do whole body rolls)
- Observe the patient’s eyes for nystagmus and note the direction, latency, and duration. Also watch for direction changing nystagmus
- Bring the patient’s head back to the neutral position in supine and wait until his / her signs and symptoms settle. Then roll the head quickly to the other side and observe
- Both side lying positions will be positive for vertigo and nystagmus (same pattern) in horizontal semi-circular canal BPPV
There are two types of nystagmus associated with the horizontal canals and they can be used to differentiate between cupulolithiasis and canalithiasis: [12]
- Geotropic (quick phase towards the earth)
- Associated with canalithiasis
- Will have latency before onset and be shorter in duration
- If geotropic nystagmus is provoked, assume that the most symptomatic side is the affected side and treat this side[3]
- Associated with canalithiasis
- Ageotropic (quick phase towards the ceiling)
- Associated with cupulolithiasis
- Will have immediate onset and prolonged duration
- If ageotropic nystagmus is provoked, assume the less symptomatic side is the affected side and treat this side[3]
- Associated with cupulolithiasis
| Involved Canal | Dix-Hallpike (DH) and Head Roll Test |
|---|---|
| Right posterior
Right DH |
Up beating, right torsion |
| Right anterior
Left DH |
Down beating, right torsion |
| Left anterior
Right DH |
Down beating, left torsion |
| Left posterior
Left DH |
Up beating, left torsion |
| Right / left horizontal
canals Head roll test |
Horizontal nystagmus, no torsion |
Distinguishing Between a Central Nervous System Lesion and BPPV[edit | edit source]
It is possible to distinguish central nervous system lesions with BPPV (see Table 3). Lesions of central origin often present with:[3][12]
- Atypical nystagmus (sustained down beating, no torsion)
- No fatiguability of the response with repeated testing
- No decrease in the nystagmus +/- vertigo with prolonged DH position
- No reversal phenomenon (reversal of nystagmus)
| Central | Peripheral | ||
| Cupulolithiasis | Canalithiasis | ||
| Latency | No | No | Yes (>1 second) |
| Duration | Persistent | 1-2 minutes | < 60 seconds |
| Direction | Uniplanar | Multiplanar | Multiplanar |
| Fatiguability | No | Yes | Yes |
Table 3. Distinguishing central nervous system lesion and BPPV
Treatment[edit | edit source]
Vertical Canal Canalithiasis[edit | edit source]
Epley Manoeuvre[edit | edit source]
The Epley manoeuvre (also known as canalith repositioning treatment) is used to treat posterior and anterior canal canalithiasis.[3]
The manoeuvre is performed as follows:[3]
- The patient is moved into DH on his / her affected side
- The therapist rotates the patient’s head through 90 degrees to the opposite side; maintaining 30 degrees of extension
- The patient is rolled onto the unaffected side with his / her head looking down
- Maintaining head rotation, the patient gently sits up at side of bed
- Each position is held until the vertigo and nystagmus has stopped and then for an additional 2 to 3 minutes
Gans Manoeuvre[edit | edit source]
The Gans manoeuvre is a modified Epley manoeuvre. It is performed as follows (assuming the right side is affected:[3]
- Patient is positioned in side lying test position - i.e. sitting.
- Patient turns head 45 degrees to the left
- Patient lies down quickly onto his / her right side (no pillow), and holds this position for 2-3 minutes until the vertigo / nystagmus resolves
- The patient then rolls over onto his / her left side, while maintaining the same head position
- Wait 2-3 minutes as above
- The patient sits up to complete the manoeuvre
Efficacy of Treatment for Vertical Canal BPPV[edit | edit source]
Epley Manoeuvre[edit | edit source]
The Epley manoeuvre is a safe and effective treatment for posterior canal BPPV (the most common variant) It can be effective for anterior canal canalithiasis as well, but it is not effective for horizontal canal canalithiasis or anterior, posterior or horizontal cupulolithiasis.[3] It has no serious side effects, but there is no evidence that it provides long-term resolution of symptoms and recurrence rates are high.[19] The Gans manoeuvre has been shown to have similar outcomes as the Epley.[19]
- 93.5 percent of patients treated with an Epley manoeuvre had positive responses compared to 50 percent of the control group[20]
- Macias and colleagues looked at 259 BPPV patients who received the Epley manoeuvre:[21]
- 74.8 percent required only one treatment
- 19 percent required two treatments
- 98.4 percent of patients were successfully treated after three sessions
Epley manoeuvre head positions in patients with posterior canal BPPV:[22]
- During an Epley manoeuvre, if the patient was returned to a sitting position without rolling over onto his / her side with the head down at 45 degrees, the remission rate was found to be 50 percent
- This suggests that the last component of the Epley manoeuvre facilitates the movement of the debris into the common crus[3]
Gans Manoeuvre[edit | edit source]
The Gans manoeuvre was developed because certain aspects of other BPPV manoeuvres, such as hyperextension of the neck during the Epley, are contraindicated for patients with vertebrobasilar insufficiency, cervical spondylosis, back problems etc.[23] Roberts and colleagues assessed the efficacy of the Gans manoeuvre and found that:[23]
- On average, 1.25 treatments were needed to resolve the posterior semi-circular canal BPPV
- Most patients (80.2%) were cleared with one treatment
- 95.6 percent were cleared after two treatments
- The Gans is, therefore, a good option for patients who cannot have the Epley or liberatory manoeuvres (see below)
Horizontal Canal Canalithiasis Treatment[edit | edit source]
There are two key treatments for horizontal canal canalithiasis:
- Forced prolonged positioning (i.e. 8 to 12 hours) lying on the unaffected side
- Barbeque roll (also known as the Lempert roll)
Barbeque Roll[edit | edit source]
To perform this canalith repositioning treatment:[3]
- The patient is positioned in supine with his / her head elevated 20 degrees and turned toward the affected side
- The therapist slowly rolls the patient’s head away from the affected side in 90 degree increments until the head has moved through 360 degrees
- Each position is maintained until the vertigo has stopped plus an additional 15 seconds
- The patient should have no vertigo or nystagmus once they are prone
NB usually whole body rolls are performed instead of just neck rotations
Efficacy of Treatment for Horizontal Canal Canalithiasis[edit | edit source]
Nuti and colleagues compared these two techniques for horizontal canal canalithiasis with an untreated control group.[25]
- Barbeque roll – patients were rotated around the longitudinal axis in 90 degree stages
- Prolonged positioning – patients lay on their uninvolved side for prolonged periods
Both treatments had similar remission rates:[25]
- 71 percent in the rolling group
- 73 percent in the forced prolonged positioning treatment
- 33 percent in the control group
A more recent study by Wang and colleagues also supports the use of the barbeque roll.[26]
Vertical Canal Cupulolithiasis[edit | edit source]
Liberatory (Semont) Manoeuvre[edit | edit source]
To treat posterior canal BPPV using the liberatory (semont) manoeuvre:[3][12]
- The patient sits with his / her legs over the side of the bed
- The patient's head is turned 45 degrees toward the unaffected side
- The therapist quickly moves the patient into side-lying on the affected side
- This position is held for 5 minutes
- The patient is then quickly moved all the way back up and then down to the opposite side-lying position, maintaining his / her head position
- This position is held for 5 minutes
- In this second position, nystagmus and vertigo typically appear. If they do not, the head is abruptly shaken once or twice to free the debris[3]
- The patient is slowly sat back up
To treat anterior canal BPPV with the liberatory (semont) manoeuvre, the manoeuvre is similar, but the patient’s head is turned to the affected side to begin:[3]
- Patient sits with legs over the side of the bed
- Patient's head is turned 45 degrees towards the affected side
- The therapist quickly moves the patient into side-lying on the affected side - essentially, the patient is lying on his / her affected canal
- This position is held for 5 minutes
- The patient is then quickly moved all the way back up and then down to the opposite side-lying position, maintaining his / her head position
- This position is held for 5 minutes
- In this second position, nystagmus and vertigo typically appear. If they do not, the patient’s head is abruptly shaken once or twice to free the debris
- The patient is slowly sat back up
Efficacy of the Liberatory Manoeuvre[edit | edit source]
Semont and colleagues found that in 711 patients with BPPV there was complete remission in 84 percent of patients after one treatment and 93 percent after a second procedure one week later.[28]
Salvinilli and colleagues also found that the liberatory manoeuvre had good results. They found there was a remission rate of 92.5 percent with one manoeuvre while the untreated control group had a remission rate of 37.5 percent.[29]
Horizontal Canal Cupulolithiasis[edit | edit source]
The modified semont manoeuvre can be used to treat horizontal canal cupulolithiasis.[30] It is performed as follows:[3]
- The patient starts in sitting on a bed. Lie him / her quickly down into side-lying on the affected side (i.e. the less symptomatic side to the patient)
- Immediately at this point, conduct a 45 degree rotation downward
- This position is held for 2 to 3 minutes
- The patient is then quickly returned to the sitting position
This modified semont manoeuvre was found to result in resolution of symptoms for 77.8 percent of patients with horizontal canal cupulolithiasis after three sessions.[3][30]
The efficacy of these treatments for BPPV are summarised in Table 4.
| BPPV variant | Efficacy
- one treatment applied - outcome complete resolution |
|---|---|
| Anterior / posterior canal canalithiasis | Epley manoeuvre: 93.5 percent [20]
Gans manoeuvre: 80.2 percent[23] |
| Horizontal canal canalithiasis | Barbeque roll: 71 percent[25] |
| Anterior / posterior canal cupulolithiasis | Liberatory manoeuvre: 92.5 percent[29] |
| Horizontal canal cupulolithiasis | Modified semont manoeuvre: 77.8 percent[30]
(3 applications) |
Brandt-Daroff Treatment: Home exercise program for BPPV[edit | edit source]
To perform these exercise programme, patients are instructed to:[3]
- Turn their head 45 degrees away from the affected side and lie quickly onto the affected side
- Hold this position until vertigo stops (+ 30 seconds)
- Then return to sitting position and hold for 30 seconds or until the vertigo stops
- Repeat these steps on the opposite side
- Repeat this sequence 10-20 times, three times per day
NB patients are advised they can stop the exercise when they have two consecutive days with no symptoms or if there has been no improvement within 2 weeks.
Effectiveness of the Brandt-Daroff Exercises[edit | edit source]
Brandt and Daroff studied the effectiveness of these exercises on a series of 67 patients with BPPV. They found that after 3 to 14 days of exercises, 98% of the subjects had no symptoms of BPPV.[31] More recent studies have also found these exercises to be effective.[32]
Clinically, however, this exercise programme often requires a prolonged period of time for patients to experience an improvement in their symptoms.[3]
Relevance of Postural Restrictions for BPPV[edit | edit source]
Postural restrictions post-Epley manoeuvre did not improve the efficacy of treatment or diminish the recurrence rate. At present, it is not, therefore, advised to place postural restrictions on patients after an Epley manoeuvre.[33][34]
Daily Epley Manoeuvres and BPPV[edit | edit source]
A daily routine of self-canalith repositioning exercises does not affect the time to recurrence or the rate of recurrence of posterior canal BPPV.[35] Patients should not, therefore, do the Epley manoeuvre as a home exercise to prevent recurrence of BPPV. [3]
Sleep Position and Laterality of BPPV[edit | edit source]
It has been found that there is an association between the ear affected by BPPV and the preferred head-lying side during sleep onset. Moreover, there are higher recurrence rates of BPPV in patients who sleep on their affected side.[36][37][38] Patients may, therefore, want to change or vary the side they sleep on sleep on if BPPV is recurring.[3]
Canal Conversion[edit | edit source]
During treatment of posterior semi-circular canal BPPV, debris may move from the posterior canal to the horizontal canal (usually) or to the anterior canal (rarely – 2.9%).[39]
This will be obvious when a DH retest results in dramatically different nystagmus patterns after an Epley manoeuvre has been performed. If this occurs, it is necessary to re-evaluate and treat the newly involved canal.[3] The Epley manoeuvre may have a higher rate of conversion than the liberatory manoeuvre.[40]
What Happens to the Otoconia?[edit | edit source]
A number of theories have been proposed to explain where the otoconia go after repositioning techniques, including:[3]
- They simply dissolve[41]
- The ‘dark cells’ of the labyrinth, which are adjacent to the utricle and crista, reabsorb the displaced otoconia[42]
- They stick back to the utricle[43]
Management Issues in BPPV[edit | edit source]
- BPPV is frequently considered a self-limiting disorder as the spontaneous remission rate can be as high as 50 percent
- However, for many individuals it persists for years if not decades
- Recurrence rate varies from 18 to 37 percent
- Antivertiginous drugs are not helpful
- Some patients may experience increased dizziness, nausea and imbalance for a day or two after treatment – possibly due to an autonomic dysfunction[44]
- It is important to bring a patient back for re-evaluation, usually in 3 to 5 days if possible
- Evaluate the patient's postural control, vestibular function and motion sensitivity
- If the patient has a vestibular hypofunction and BPPV, treat the BPPV first
- Be alert to central signs and symptoms[3]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710-5.
- ↑ 2.0 2.1 2.2 2.3 Balatsouras DG, Koukoutsis G, Fassolis A, Moukos A, Apris A. Benign paroxysmal positional vertigo in the elderly: current insights. Clin Interv Aging. 2018;13:2251-66.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 3.28 3.29 3.30 3.31 3.32 3.33 Tonks B. Benign Paroxysmal Positional Vertigo Course. Plus , 2021.
- ↑ Palmeri R, Kumar A. Benign Paroxysmal Positional Vertigo. [Updated 2020 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470308/
- ↑ You P, Instrum R, Parnes L. Benign paroxysmal positional vertigo. Laryngoscope investigative otolaryngology. 2019 Feb;4(1):116-23.
- ↑ Zhang D, Zhang S, Zhang H, Xu Y, Fu S, Yu M, Ji P. Evaluation of vertebrobasilar artery changes in patients with benign paroxysmal positional vertigo. Neuroreport. 2013;24(13):741-5.
- ↑ Jeong SH, Kim JS, Shin JW, Kim S, Lee H, Lee AY et al. Decreased serum vitamin D in idiopathic benign paroxysmal positional vertigo. J Neurol. 2013;260(3):832-8.
- ↑ 8.0 8.1 Chen J, Zhao W, Yue X, Zhang P. Risk factors for the occurrence of benign paroxysmal positional vertigo: A systematic review and meta-analysis. Front Neurol. 2020;11:506.
- ↑ Kim HJ, Park J, Kim JS. Update on benign paroxysmal positional vertigo. Journal of Neurology. 2021 May;268(5):1995-2000.
- ↑ 10.0 10.1 Kansu L, Aydin E, Gulsahi K. Benign paroxysmal positional vertigo after nonotologic surgery: case series. J Maxillofac Oral Surg. 2015;14(Suppl 1):113-5.
- ↑ Li S, Wang Z, Liu Y, Cao J, Zheng H, Jing Y et al. Risk factors for the recurrence of benign paroxysmal positional vertigo: a systematic review and meta-analysis. Ear Nose Throat J. 2020:145561320943362.
- ↑ 12.0 12.1 12.2 12.3 12.4 Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T et al. Clinical practice guideline: benign paroxysmal positional vertigo (update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1-S47.
- ↑ Kaplan DM, Slovik Y, Joshua BZ, Puterman M, Kraus M. Head shaking during Dix-Hallpike exam increases the diagnostic yield of posterior semicircular canal BPPV. Otol Neurotol. 2013;34(8):1444-7.
- ↑ BMJ Learning. Vertigo - Dix-Hallpike Manoeuvre from BMJ Learning. Available from: https://www.youtube.com/watch?v=8RYB2QlO1N4&t=1s [last accessed 13/6/2021[
- ↑ Cohen HS. Side-lying as an alternative to the Dix-Hallpike test of the posterior canal. Otol Neurotol. 2004;25(2):130-4.
- ↑ Physical Therapy Nation. Sidelying Test for Posterior Canal BPPV. Available from: https://www.youtube.com/watch?v=fe63hTHR2cw [last accessed 13/6/2021]
- ↑ EducatedPT. Supine Roll Test for Horizontal Canal BPPV. Available from: https://www.youtube.com/watch?v=ns8XZ4rKiJc [last accessed 13/6/2021]
- ↑ BMJ Learning. Vertigo - Epley manoeuvre from BMJ Learning. Available from: https://www.youtube.com/watch?v=jBzID5nVQjk [last accessed 13/6/2021]
- ↑ 19.0 19.1 Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 Dec 8;(12):CD003162.
- ↑ 20.0 20.1 Wolf M, Hertanu T, Novikov I, Kronenberg J. Epley's manoeuvre for benign paroxysmal positional vertigo: a prospective study. Clin Otolaryngol Allied Sci. 1999;24(1):43-6.
- ↑ Macias JD, Lambert KM, Massingale S, Ellensohn A, Fritz JA. Variables affecting treatment in benign paroxysmal positional vertigo. Laryngoscope. 2000;110(11):1921-4.
- ↑ Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE. Single treatment approaches to benign paroxysmal positional vertigo. Archives of Otolaryngology ‐ Head & Neck Surgery 1993;119(4):450‐4.
- ↑ 23.0 23.1 23.2 Roberts RA, Gans RE, Montaudo RL. Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2006;17(8):598-604.
- ↑ Ascension Via Christi. Barbeque Roll Lempert maneuver. Available from: https://www.youtube.com/watch?v=ufD_tcSx5dQ [last accessed 13/6/2021]
- ↑ 25.0 25.1 25.2 Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 1998;118(4):455-60.
- ↑ Wang YH, Chan CY, Liu QH. Benign paroxsymal positional vertigo - recommendations for treatment in primary care. Ther Clin Risk Manag. 2019;15:719-725.
- ↑ EducatedPT. Liberatory (Semont) Maneuver for BPPV. Available from: https://www.youtube.com/watch?v=pK9qaprUU64 [last accessed 13/6/2021]
- ↑ Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003;169(7):681-93.
- ↑ 29.0 29.1 Salvinelli F, Casale M, Trivelli M, D'Ascanio L, Firrisi L, Lamanna F et al. Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semont's maneuver and no treatment strategy. Clin Ter. 2003;154(1):7-11.
- ↑ 30.0 30.1 30.2 Casani AP, Vannucci G, Fattori B, Berrettini S. The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112(1):172-8.
- ↑ Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol. 1980;106(8):484-5.
- ↑ Cetin YS, Ozmen OA, Demir UL, Kasapoglu F, Basut O, Coskun H. Comparison of the effectiveness of Brandt-Daroff Vestibular training and Epley Canalith repositioning maneuver in benign Paroxysmal positional vertigo long term result: A randomized prospective clinical trial. Pak J Med Sci. 2018;34(3):558-63.
- ↑ Casqueiro JC, Ayala A, Monedero G. No more postural restrictions in posterior canal benign paroxysmal positional vertigo. Otol Neurotol. 2008;29(5):706-9.
- ↑ Balikci HH, Ozbay I. Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo. Auris Nasus Larynx. 2014;41(5):428-31.
- ↑ Helminski JO, Janssen I, Hain TC. Daily exercise does not prevent recurrence of benign paroxysmal positional vertigo. Otol Neurotol. 2008;29(7):976-81.
- ↑ Korres SG, Papadakis CE, Riga MG, Balatsouras DG, Dikeos DG, Soldatos CR. Sleep position and laterality of benign paroxysmal positional vertigo. J Laryngol Otol. 2008;122(12):1295-8.
- ↑ Shigeno K, Ogita H, Funabiki K. Benign paroxysmal positional vertigo and head position during sleep. J Vestib Res. 2012;22(4):197-203.
- ↑ Li S, Tian L, Han Z, Wang J. Impact of postmaneuver sleep position on recurrence of benign paroxysmal positional vertigo. PLoS One. 2013;8(12):e83566.
- ↑ Park S, Kim BG, Kim SH, Chu H, Song MY, Kim M. Canal conversion between anterior and posterior semicircular canal in benign paroxysmal positional vertigo. Otol Neurotol. 2013;34(9):1725-8.
- ↑ Anagnostou E, Stamboulis E, Kararizou E. Canal conversion after repositioning procedures: comparison of Semont and Epley maneuver. J Neurol. 2014;261(5):866-9.
- ↑ Parker DE, Covell WP, von Gierke HE. Exploration of vestibular damage in guinea pigs following mechanical stimulation. Acta Otolaryngol. 1968:Suppl 239:7+.
- ↑ Lim DJ The development and structure of otoconia. In: I Friedman, J Ballantyne (eds). Ultrastructural Atlas of the Inner Ear. London: Butterworth, 1984. p. 245-69.
- ↑ Otsuka K, Suzuki M, Shimizu S, Konomi U, Inagaki T, Iimura Y et al. Model experiments of otoconia stability after canalith repositioning procedure of BPPV. Acta Otolaryngol. 2010 Jul;130(7):804-9.
- ↑ Kim HA, Lee H. Autonomic dysfunction as a possible cause of residual dizziness after successful treatment in benign paroxysmal positional vertigo. Clin Neurophysiol. 2014;125(3):608-14.