Intervertebral disc: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors - | '''Original Editors - <br>''' | ||
'''Top Contributors''' - | '''Top Contributors''' - Alexander Chan (PhD, MPH, etc.) B Physiotherapy (Hons) Professor, Program Director, etc.) | ||
<br></div> | <br></div> | ||
== Definition/Description == | == Definition/Description == | ||
| Line 22: | Line 22: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
<u>Morphology</u> | |||
The IVD consists of three distinct components (Figure 2): <br>• a central nucleus pulposus (NP);<br>• a peripheral annulus fibrosus (AF);<br>• two vertebral endplates (VEPs). | The IVD consists of three distinct components (Figure 2): <br>• a central nucleus pulposus (NP);<br>• a peripheral annulus fibrosus (AF);<br>• two vertebral endplates (VEPs). | ||
| Line 34: | Line 34: | ||
<br> | <br> | ||
''Nucleus Pulposus'' | |||
The nucleus pulposus is a gel-like mass composed of water and proteoglycans held by randomly arranged fibres of collagen <ref name="Bogduk">Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.</ref> <ref name="Gruber">Gruber, H.E. and E.N. Hanley, Jr., Recent advances in disc cell biology. Spine (Phila Pa 1976), 2003. 28(2): p. 186-93.</ref> <ref name="Humzah">Humzah, M.D. and R.W. Soames, Human intervertebral disc: structure and function. Anat Rec, 1988. 220(4): p. 337-56.</ref>. With it’s water-attracting properties, any attempt to deform the nucleus causes the applied pressure to be dispersed into various directions, similar to a person on a waterbed. | The nucleus pulposus is a gel-like mass composed of water and proteoglycans held by randomly arranged fibres of collagen <ref name="Bogduk">Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.</ref> <ref name="Gruber">Gruber, H.E. and E.N. Hanley, Jr., Recent advances in disc cell biology. Spine (Phila Pa 1976), 2003. 28(2): p. 186-93.</ref> <ref name="Humzah">Humzah, M.D. and R.W. Soames, Human intervertebral disc: structure and function. Anat Rec, 1988. 220(4): p. 337-56.</ref>. With it’s water-attracting properties, any attempt to deform the nucleus causes the applied pressure to be dispersed into various directions, similar to a person on a waterbed. | ||
| Line 40: | Line 40: | ||
<br> | <br> | ||
''Annulus Fibrosus'' | |||
The annulus fibrosus consists of “lamellae” or concentric layers of collagen fibres <ref name="Marchand">Marchand, F. and A.M. Ahmed, Investigation of the laminate structure of lumbar disc anulus fibrosus. Spine (Phila Pa 1976), 1990. 15(5): p. 402-10.</ref>. The fibre orientation of each layer of lamellae alternate and therefore allow effective resistance of multidirectional movements. | The annulus fibrosus consists of “lamellae” or concentric layers of collagen fibres <ref name="Marchand">Marchand, F. and A.M. Ahmed, Investigation of the laminate structure of lumbar disc anulus fibrosus. Spine (Phila Pa 1976), 1990. 15(5): p. 402-10.</ref>. The fibre orientation of each layer of lamellae alternate and therefore allow effective resistance of multidirectional movements. | ||
| Line 46: | Line 46: | ||
<br> | <br> | ||
''Vertebral endplate'' | |||
The vertebral endplate is a plate of cartilage that acts as a barrier between the disc and the vertebral body. They cover the superior and inferior aspects of the annulus fibrosus and the nucleus pulposus. | The vertebral endplate is a plate of cartilage that acts as a barrier between the disc and the vertebral body. They cover the superior and inferior aspects of the annulus fibrosus and the nucleus pulposus. | ||
<br> | <br><u>Innervation</u> | ||
The disc is innervated in the outer few millimetres of the annulus fibrosus <ref name="Roberts">Roberts, S., et al., Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am, 2006. 88 Suppl 2(Supplement 2): p. 10-4.</ref>. | The disc is innervated in the outer few millimetres of the annulus fibrosus <ref name="Roberts">Roberts, S., et al., Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am, 2006. 88 Suppl 2(Supplement 2): p. 10-4.</ref>. | ||
<br> | <br><u>Vascular supply and nutrition</u> | ||
The IVD is largely avascular, with no major arterial branches to the disc <ref name="Urban4">Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.</ref>. The outer annular layers are supplied by small branches from metaphysial arteries [1]. Due to the avascular nature of the disc, the nutrition is dependent on metabolite diffusion <ref name="Urban">Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.</ref> <ref name="Urban 2">Urban, J., S. Holm, and A. Maroudas, Diffusion of small solutes into the intervertebral disc. Biorheology, 1978. 15(3-4): p. 203-21.</ref> <ref name="Urban 3">Urban, J.P., S. Smith, and J.C. Fairbank, Nutrition of the intervertebral disc. Spine (Phila Pa 1976), 2004. 29(23): p. 2700-9.</ref>. | The IVD is largely avascular, with no major arterial branches to the disc <ref name="Urban4">Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.</ref>. The outer annular layers are supplied by small branches from metaphysial arteries [1]. Due to the avascular nature of the disc, the nutrition is dependent on metabolite diffusion <ref name="Urban">Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.</ref> <ref name="Urban 2">Urban, J., S. Holm, and A. Maroudas, Diffusion of small solutes into the intervertebral disc. Biorheology, 1978. 15(3-4): p. 203-21.</ref> <ref name="Urban 3">Urban, J.P., S. Smith, and J.C. Fairbank, Nutrition of the intervertebral disc. Spine (Phila Pa 1976), 2004. 29(23): p. 2700-9.</ref>. | ||
| Line 60: | Line 60: | ||
<br> | <br> | ||
<u>Biomechanics</u> | |||
<br> | <br> ''Weight bearing'' | ||
The disc is subjected to various loads, including compressive, tensile and shear stresses <ref name="Stokes">Stokes, I. and J. Iatridis, Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976), 2004. 29(23): p. 2724-32.</ref> <ref name="White">White, A.A. and M.M. Panjabi, Clinical biomechanics of the spine. Vol. 446. 1990: Lippincott Philadelphia.</ref>. During compressive loading, hydrostatic pressure develops within the NP, which thereby disperses the forces towards the endplates as well as the AF <ref name="Reuber">Reuber, M., et al., Bulging of lumbar intervertebral disks. J Biomech Eng, 1982. 104(3): p. 187-92.</ref> <ref name="Broberg">Broberg, K.B., On the mechanical behaviour of intervertebral discs. Spine (Phila Pa 1976), 1983. 8(2): p. 151-65.</ref> <ref name="Reuber">Reuber, M., et al., Bulging of lumbar intervertebral disks. J Biomech Eng, 1982. 104(3): p. 187-92.</ref>. This mechanism slows the rate applied loads are transmitted to the adjacent vertebra, giving the disc its shock absorbing abilities <ref name="Shah">Shah, J.S., W.G. Hampson, and M.I. Jayson, The distribution of surface strain in the cadaveric lumbar spine. J Bone Joint Surg Br, 1978. 60-B(2): p. 246-51.</ref>. | The disc is subjected to various loads, including compressive, tensile and shear stresses <ref name="Stokes">Stokes, I. and J. Iatridis, Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976), 2004. 29(23): p. 2724-32.</ref> <ref name="White">White, A.A. and M.M. Panjabi, Clinical biomechanics of the spine. Vol. 446. 1990: Lippincott Philadelphia.</ref>. During compressive loading, hydrostatic pressure develops within the NP, which thereby disperses the forces towards the endplates as well as the AF <ref name="Reuber">Reuber, M., et al., Bulging of lumbar intervertebral disks. J Biomech Eng, 1982. 104(3): p. 187-92.</ref> <ref name="Broberg">Broberg, K.B., On the mechanical behaviour of intervertebral discs. Spine (Phila Pa 1976), 1983. 8(2): p. 151-65.</ref> <ref name="Reuber">Reuber, M., et al., Bulging of lumbar intervertebral disks. J Biomech Eng, 1982. 104(3): p. 187-92.</ref>. This mechanism slows the rate applied loads are transmitted to the adjacent vertebra, giving the disc its shock absorbing abilities <ref name="Shah">Shah, J.S., W.G. Hampson, and M.I. Jayson, The distribution of surface strain in the cadaveric lumbar spine. J Bone Joint Surg Br, 1978. 60-B(2): p. 246-51.</ref>. | ||
| Line 68: | Line 68: | ||
<br> | <br> | ||
''Movements'' | |||
The disc is also involved in permitting movements between vertebral bodies, which include: <br>• axial compression / distraction;<br>• flexion / extension;<br>• axial rotation;<br>• lateral flexion. | The disc is also involved in permitting movements between vertebral bodies, which include: <br>• axial compression / distraction;<br>• flexion / extension;<br>• axial rotation;<br>• lateral flexion. | ||
| Line 74: | Line 74: | ||
<br> | <br> | ||
''Nuclear migration'' | |||
Asymmetric compressive loading disc can cause the NP to migrate in a direction opposite to the compression <ref name="Krag">Krag, M.H., et al., Internal displacement distribution from in vitro loading of human thoracic and lumbar spinal motion segments: experimental results and theoretical predictions. Spine (Phila Pa 1976), 1987. 12(10): p. 1001-7.</ref> <ref name="Shah">Shah, J.S., W.G. Hampson, and M.I. Jayson, The distribution of surface strain in the cadaveric lumbar spine. J Bone Joint Surg Br, 1978. 60-B(2): p. 246-51.</ref> <ref name="Schnebel">Schnebel, B.E., et al., A digitizing technique for the study of movement of intradiscal dye in response to flexion and extension of the lumbar spine. Spine (Phila Pa 1976), 1988. 13(3): p. 309-12.</ref> <ref name="Fennell">Fennell, A., A. Jones, and D. Hukins, Migration of the nucleus pulposus within the intervertebral disc during flexion and extension of the spine. Spine (Phila Pa 1976), 1996. 21(23): p. 2753-7.</ref>. For example, during forward bending (or flexion) of the lumbar spine, the NP migrates posteriorly or backwards (Figure 4). Conversely, during backwards bending (or extension), the nucleus is squeezed anteriorly or forwards. This concept is known as the dynamic disc model <ref name="Kolber">Kolber, M.J. and W.J. Hanney, The dynamic disc model: a systematic review of the literature. Phys Ther Rev, 2009. 14(3): p. 181-189.</ref>. Although NP migration has been shown to behave predictably in asymptomatic discs, a variable pattern of migration occurs in people with symptomatic and/or degenerative IVDs <ref name="Kolber" />. | Asymmetric compressive loading disc can cause the NP to migrate in a direction opposite to the compression <ref name="Krag">Krag, M.H., et al., Internal displacement distribution from in vitro loading of human thoracic and lumbar spinal motion segments: experimental results and theoretical predictions. Spine (Phila Pa 1976), 1987. 12(10): p. 1001-7.</ref> <ref name="Shah">Shah, J.S., W.G. Hampson, and M.I. Jayson, The distribution of surface strain in the cadaveric lumbar spine. J Bone Joint Surg Br, 1978. 60-B(2): p. 246-51.</ref> <ref name="Schnebel">Schnebel, B.E., et al., A digitizing technique for the study of movement of intradiscal dye in response to flexion and extension of the lumbar spine. Spine (Phila Pa 1976), 1988. 13(3): p. 309-12.</ref> <ref name="Fennell">Fennell, A., A. Jones, and D. Hukins, Migration of the nucleus pulposus within the intervertebral disc during flexion and extension of the spine. Spine (Phila Pa 1976), 1996. 21(23): p. 2753-7.</ref>. For example, during forward bending (or flexion) of the lumbar spine, the NP migrates posteriorly or backwards (Figure 4). Conversely, during backwards bending (or extension), the nucleus is squeezed anteriorly or forwards. This concept is known as the dynamic disc model <ref name="Kolber">Kolber, M.J. and W.J. Hanney, The dynamic disc model: a systematic review of the literature. Phys Ther Rev, 2009. 14(3): p. 181-189.</ref>. Although NP migration has been shown to behave predictably in asymptomatic discs, a variable pattern of migration occurs in people with symptomatic and/or degenerative IVDs <ref name="Kolber" />. | ||
| Line 102: | Line 102: | ||
== Key Research == | == Key Research == | ||
Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone. | Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.<br> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
Revision as of 12:43, 6 October 2014
Original Editors -
Top Contributors - Alexander Chan (PhD, MPH, etc.) B Physiotherapy (Hons) Professor, Program Director, etc.)
Definition/Description[edit | edit source]
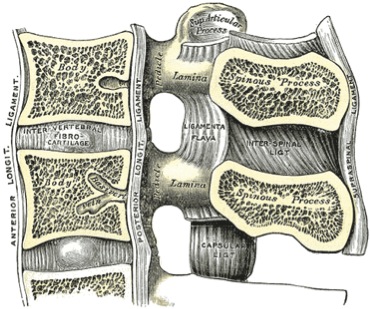
The intervertebral disc (IVD) is important in the normal functioning of the spine. It is a cushion of fibrocartilage and the principal joint between two vertebrae in the spinal column (Figure 1).
Figure 1: Segment of spinal column
There are 23 discs in the human spine: 6 in the cervical region (neck), 12 in the thoracic region (middle back), and 5 in the lumbar region (lower back).
Clinically Relevant Anatomy[edit | edit source]
Morphology
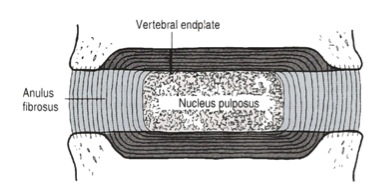
The IVD consists of three distinct components (Figure 2):
• a central nucleus pulposus (NP);
• a peripheral annulus fibrosus (AF);
• two vertebral endplates (VEPs).
Figure 2: Detailed structure of the IVD (adapted from Bogduk 2005)
Nucleus Pulposus
The nucleus pulposus is a gel-like mass composed of water and proteoglycans held by randomly arranged fibres of collagen [1] [2] [3]. With it’s water-attracting properties, any attempt to deform the nucleus causes the applied pressure to be dispersed into various directions, similar to a person on a waterbed.
Annulus Fibrosus
The annulus fibrosus consists of “lamellae” or concentric layers of collagen fibres [4]. The fibre orientation of each layer of lamellae alternate and therefore allow effective resistance of multidirectional movements.
Vertebral endplate
The vertebral endplate is a plate of cartilage that acts as a barrier between the disc and the vertebral body. They cover the superior and inferior aspects of the annulus fibrosus and the nucleus pulposus.
Innervation
The disc is innervated in the outer few millimetres of the annulus fibrosus [5].
Vascular supply and nutrition
The IVD is largely avascular, with no major arterial branches to the disc [6]. The outer annular layers are supplied by small branches from metaphysial arteries [1]. Due to the avascular nature of the disc, the nutrition is dependent on metabolite diffusion [7] [8] [9].
Biomechanics
Weight bearing
The disc is subjected to various loads, including compressive, tensile and shear stresses [10] [11]. During compressive loading, hydrostatic pressure develops within the NP, which thereby disperses the forces towards the endplates as well as the AF [12] [13] [12]. This mechanism slows the rate applied loads are transmitted to the adjacent vertebra, giving the disc its shock absorbing abilities [14].
Movements
The disc is also involved in permitting movements between vertebral bodies, which include:
• axial compression / distraction;
• flexion / extension;
• axial rotation;
• lateral flexion.
Nuclear migration
Asymmetric compressive loading disc can cause the NP to migrate in a direction opposite to the compression [15] [14] [16] [17]. For example, during forward bending (or flexion) of the lumbar spine, the NP migrates posteriorly or backwards (Figure 4). Conversely, during backwards bending (or extension), the nucleus is squeezed anteriorly or forwards. This concept is known as the dynamic disc model [18]. Although NP migration has been shown to behave predictably in asymptomatic discs, a variable pattern of migration occurs in people with symptomatic and/or degenerative IVDs [18].
Figure 4: Direction of nuclear migration within the IVD during spinal movements (adapted from McKenzie 1981)
Differential Diagnosis[edit | edit source]
Refer to Lumbar discogenic pain and Thoracic disc syndrome.
Diagnostic Procedures[edit | edit source]
Refer to Lumbar discogenic pain and Thoracic disc syndrome.
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
Refer to Lumbar discogenic pain.
Key Research[edit | edit source]
Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ Bogduk, N., Clinical anatomy of the lumbar spine and sacrum. 4th ed. 2005, New York: Churchill Livingstone.
- ↑ Gruber, H.E. and E.N. Hanley, Jr., Recent advances in disc cell biology. Spine (Phila Pa 1976), 2003. 28(2): p. 186-93.
- ↑ Humzah, M.D. and R.W. Soames, Human intervertebral disc: structure and function. Anat Rec, 1988. 220(4): p. 337-56.
- ↑ Marchand, F. and A.M. Ahmed, Investigation of the laminate structure of lumbar disc anulus fibrosus. Spine (Phila Pa 1976), 1990. 15(5): p. 402-10.
- ↑ Roberts, S., et al., Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am, 2006. 88 Suppl 2(Supplement 2): p. 10-4.
- ↑ Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.
- ↑ Urban, J.P., et al., Nutrition of the intervertebral disk. An in vivo study of solute transport. Clin Orthop Relat Res, 1977(129): p. 101-14.
- ↑ Urban, J., S. Holm, and A. Maroudas, Diffusion of small solutes into the intervertebral disc. Biorheology, 1978. 15(3-4): p. 203-21.
- ↑ Urban, J.P., S. Smith, and J.C. Fairbank, Nutrition of the intervertebral disc. Spine (Phila Pa 1976), 2004. 29(23): p. 2700-9.
- ↑ Stokes, I. and J. Iatridis, Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976), 2004. 29(23): p. 2724-32.
- ↑ White, A.A. and M.M. Panjabi, Clinical biomechanics of the spine. Vol. 446. 1990: Lippincott Philadelphia.
- ↑ 12.0 12.1 Reuber, M., et al., Bulging of lumbar intervertebral disks. J Biomech Eng, 1982. 104(3): p. 187-92.
- ↑ Broberg, K.B., On the mechanical behaviour of intervertebral discs. Spine (Phila Pa 1976), 1983. 8(2): p. 151-65.
- ↑ 14.0 14.1 Shah, J.S., W.G. Hampson, and M.I. Jayson, The distribution of surface strain in the cadaveric lumbar spine. J Bone Joint Surg Br, 1978. 60-B(2): p. 246-51.
- ↑ Krag, M.H., et al., Internal displacement distribution from in vitro loading of human thoracic and lumbar spinal motion segments: experimental results and theoretical predictions. Spine (Phila Pa 1976), 1987. 12(10): p. 1001-7.
- ↑ Schnebel, B.E., et al., A digitizing technique for the study of movement of intradiscal dye in response to flexion and extension of the lumbar spine. Spine (Phila Pa 1976), 1988. 13(3): p. 309-12.
- ↑ Fennell, A., A. Jones, and D. Hukins, Migration of the nucleus pulposus within the intervertebral disc during flexion and extension of the spine. Spine (Phila Pa 1976), 1996. 21(23): p. 2753-7.
- ↑ 18.0 18.1 Kolber, M.J. and W.J. Hanney, The dynamic disc model: a systematic review of the literature. Phys Ther Rev, 2009. 14(3): p. 181-189.