Integumentary System: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
* Hair | * Hair | ||
* Nails. | * Nails. | ||
In addition to its barrier function, this system performs many intricate functions such as body temperature regulation, cell fluid maintenance, synthesis of [[Vitamin D Deficiency|Vitamin D]], and detection of stimuli. The various components of this system work in conjunction to carry out these functions<ref>Kim JY, Dao H. [https://www.ncbi.nlm.nih.gov/books/NBK554386/ Physiology, Integument]. InStatPearls [Internet] 2020 Feb 17. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK554386/ (last accessed 23.10.2020)</ref>. | In addition to its barrier function, this system performs many intricate functions such as body temperature regulation, cell fluid maintenance, synthesis of [[Vitamin D Deficiency|Vitamin D]], and detection of stimuli. The various components of this system work in conjunction to carry out these functions<ref name=":0">Kim JY, Dao H. [https://www.ncbi.nlm.nih.gov/books/NBK554386/ Physiology, Integument]. InStatPearls [Internet] 2020 Feb 17. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK554386/ (last accessed 23.10.2020)</ref>. | ||
== An Introduction - Key Facts == | == An Introduction - Key Facts == | ||
#Skin accounts for about 16% of your total body weight <ref name="One" /> | #Skin accounts for about 16% of your total body weight <ref name="One">Martini FH, Nath, JL. Fundamentals of Anatomy and Physiology. 8th ed. Pearson. San Francisco: Benjamin Cummings. 2009</ref> | ||
#Its surface area covers between 1.5-2m<sup>2 </sup><ref name="One" /> | #Its surface area covers between 1.5-2m<sup>2 </sup><ref name="One" /> | ||
#Weighs approximately 3-5kg <ref name="Two">Turkington C, Dover JS. Skin Deep. 3rd ed. New York: Checkmark Books. 2007</ref> | #Weighs approximately 3-5kg <ref name="Two">Turkington C, Dover JS. Skin Deep. 3rd ed. New York: Checkmark Books. 2007</ref> | ||
| Line 26: | Line 26: | ||
#Skin is made up of the Epidermis and the Dermis, each having separate sublayers <ref name="p5">Mclafferty E Hendry C Farley A. The integumentary system: anatomy, physiology and function of skin. Nursing Standard 2010;27:35-42.</ref> | #Skin is made up of the Epidermis and the Dermis, each having separate sublayers <ref name="p5">Mclafferty E Hendry C Farley A. The integumentary system: anatomy, physiology and function of skin. Nursing Standard 2010;27:35-42.</ref> | ||
== General Function == | == General Function == | ||
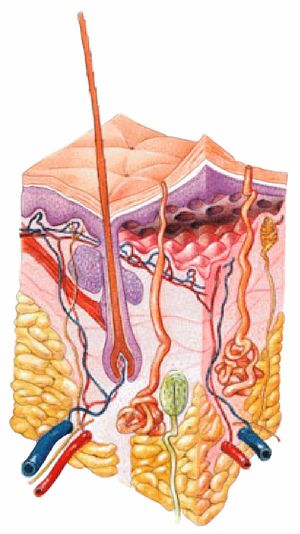
[[File:Integumentary system.jpg|right|frameless]] | [[File:Integumentary system.jpg|right|frameless|450x450px]] | ||
The skin has several functions that provide several purposes<ref name="one">Martini FH, Nath, JL. Fundamentals of Anatomy and Physiology. 8th ed. Pearson. San Francisco: Benjamin Cummings. 2009</ref> ; | The skin has several functions that provide several purposes<ref name="one">Martini FH, Nath, JL. Fundamentals of Anatomy and Physiology. 8th ed. Pearson. San Francisco: Benjamin Cummings. 2009</ref> ; | ||
* | *Physical protection: The integumentary is the covering of the human body and its' most apparent function is physical protection. The skin itself is a tightly knit network of cells, with each layer contributing to its strength. The epidermis has an outermost layer created by layers of dead keratin that can withstand wear and tear of the outer environment, the dermis provides the epidermis with blood supply and has nerves that bring danger to attention amongst other functions, the hypodermis provides physical cushioning to any mechanical trauma through adipose storage, and the glands secrete protective films throughout the body. The nails protect the digits, which are prone to repeated trauma by creating a hard covering and hairs throughout the body filter harmful particles from entering the eyes, ears, nose, etc. | ||
*Excretion | *Immunity: The skin is the body’s first line of defense acting as a physical barrier preventing direct entry of pathogens. Antimicrobial peptides (AMPs) and lipids on the skin also act as a biomolecular barrier that disrupts bacterial membranes. An additional aspect of the skin’s immunity lies in the resident immune cells. Both myeloid and lymphoid cells are present in the skin, and some, such as the Langerhans cells or dermal dendritic cells, possess the capability to travel to the periphery and activate the greater [[Immune System|immune system]]<ref name=":0" /> | ||
*Thermoregulation | *Excretion: Of salt, water and waste products through glands<ref name=":0" /> | ||
* | *Thermoregulation: The skin has a large surface area that is highly vascularized, which allows it to conserve and release heat through vasoconstriction and vasodilation, respectively<ref name=":0" />. | ||
*Fat | *Vitamin D synthesis: The primary sources of vitamin D are sun exposure and oral intake. With ultraviolet sunlight exposure, 7-dehydrocholesterol converts to vitamin D3 in the skin, which is then hydroxylated in the liver then kidney into its active metabolite form, 1,25-dihydroxy vitamin D (calcitriol). This metabolite ultimately leads to increased calcium absorption in the gut and is crucial for bone health<ref name=":0" />. | ||
*Sensation- | *Fat Storage | ||
*Sensation- Skin innervation is by various types of sensory nerve endings that discriminate pain, temperature, touch, and vibration. Each type of receptor and nerve fiber varies in its adaptive and conductive speeds, leading to a wide range of signals that can be integrated to create an understanding of the external environment and help the body to react appropriately<ref name=":0" />. | |||
If not working correctly, each of the functions can have important clinical implications and all should be considered when working with patients. For example an important clinical association with the breakdown of the ability of the skin to provide protection is [[Pressure Ulcers|pressure sores]]. | If not working correctly, each of the functions can have important clinical implications and all should be considered when working with patients. For example an important clinical association with the breakdown of the ability of the skin to provide protection is [[Pressure Ulcers|pressure sores]]. | ||
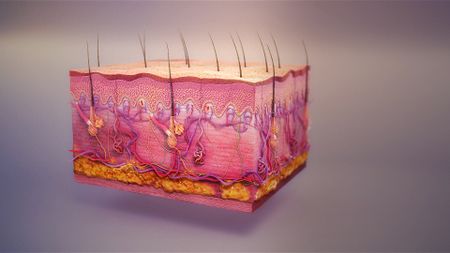
== Structure of the Skin == | == Structure of the Skin == | ||
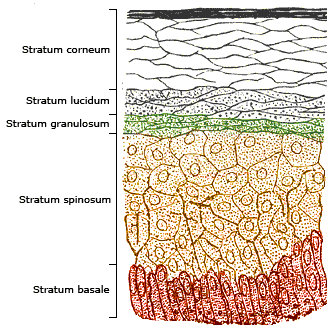
[[Image: | [[Image:Skinlayers.png|right|332x329px|A diagram Showing the Layers of the Epidermis|frameless]]The skin is made up of two layers—the superficial epidermis and the deeper dermis. | ||
Epidermis: | |||
* Tough, outer layer that acts as the first line of defense against the external environment | |||
* Regenerates from stem cells located in the basal layer that grow up towards the corneum. The epidermis itself is devoid of blood supply and derives its nutrition from the underlying dermis | |||
Composed of stratified squamous epithelial cells that further break down into four to five layers (see image R). From superficial to deep, the primary layers are the | |||
* Stratum corneum | |||
* Stratum granulosum | |||
* Stratum spinosum | |||
* Stratum basale | |||
* In the palms and soles where the skin is thicker, there is an additional layer of skin between the stratum corneum and stratum granulosum called the stratum lucidum. | |||
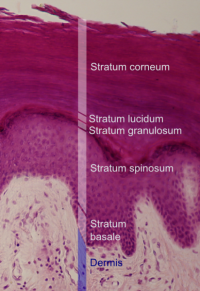
[[Image:EpidermalLayersHistology.png|thumb|right|200x350px|Layers of the Skin]]Dermis | |||
* Underlying connective tissue framework that supports the epidermis | |||
* The dermis as a whole contains blood and lymph vessels, nerves, sweat glands, hair follicles, and various other structures embedded within the connective tissue. | |||
Further subdivides into two layers | |||
* Superficial papillary dermis - forms finger-like projections into the epidermis, known as dermal papillae, and consists of highly vascularized, loose connective tissue. | |||
* Deep reticular layer - has dense connective tissue that forms a strong network<ref name=":0" />. | |||
The dermis | |||
== Links to other Areas or Topics to Consider == | == Links to other Areas or Topics to Consider == | ||
Revision as of 07:52, 23 October 2020
Original Editor - Scott Buxton
Top Contributors - Scott Buxton, Lucinda hampton, Wendy Walker, Admin, Kim Jackson, WikiSysop, Joao Costa, 127.0.0.1 and Vidya Acharya
The Integumentary System[edit | edit source]
The integumentary system is the largest organ of the body that forms a physical barrier between the external environment and the internal environment that it serves to protect and maintain.
The integumentary system includes
- Skin (epidermis, dermis)
- Hypodermis,
- Associated glands,
- Hair
- Nails.
In addition to its barrier function, this system performs many intricate functions such as body temperature regulation, cell fluid maintenance, synthesis of Vitamin D, and detection of stimuli. The various components of this system work in conjunction to carry out these functions[1].
An Introduction - Key Facts[edit | edit source]
- Skin accounts for about 16% of your total body weight [2]
- Its surface area covers between 1.5-2m2 [2]
- Weighs approximately 3-5kg [3]
- Is generally 1-2mm thick, but varies depending on its function, 0.5mm on eyelids but 3.4mm on soles of your feet [4]
- It is your body's first line of defence [2]
- The system contains all of the appendages including hair, nails, sebaceous glands and sweat glands[5]
- Skin is made up of the Epidermis and the Dermis, each having separate sublayers [6]
General Function[edit | edit source]
The skin has several functions that provide several purposes[7] ;
- Physical protection: The integumentary is the covering of the human body and its' most apparent function is physical protection. The skin itself is a tightly knit network of cells, with each layer contributing to its strength. The epidermis has an outermost layer created by layers of dead keratin that can withstand wear and tear of the outer environment, the dermis provides the epidermis with blood supply and has nerves that bring danger to attention amongst other functions, the hypodermis provides physical cushioning to any mechanical trauma through adipose storage, and the glands secrete protective films throughout the body. The nails protect the digits, which are prone to repeated trauma by creating a hard covering and hairs throughout the body filter harmful particles from entering the eyes, ears, nose, etc.
- Immunity: The skin is the body’s first line of defense acting as a physical barrier preventing direct entry of pathogens. Antimicrobial peptides (AMPs) and lipids on the skin also act as a biomolecular barrier that disrupts bacterial membranes. An additional aspect of the skin’s immunity lies in the resident immune cells. Both myeloid and lymphoid cells are present in the skin, and some, such as the Langerhans cells or dermal dendritic cells, possess the capability to travel to the periphery and activate the greater immune system[1]
- Excretion: Of salt, water and waste products through glands[1]
- Thermoregulation: The skin has a large surface area that is highly vascularized, which allows it to conserve and release heat through vasoconstriction and vasodilation, respectively[1].
- Vitamin D synthesis: The primary sources of vitamin D are sun exposure and oral intake. With ultraviolet sunlight exposure, 7-dehydrocholesterol converts to vitamin D3 in the skin, which is then hydroxylated in the liver then kidney into its active metabolite form, 1,25-dihydroxy vitamin D (calcitriol). This metabolite ultimately leads to increased calcium absorption in the gut and is crucial for bone health[1].
- Fat Storage
- Sensation- Skin innervation is by various types of sensory nerve endings that discriminate pain, temperature, touch, and vibration. Each type of receptor and nerve fiber varies in its adaptive and conductive speeds, leading to a wide range of signals that can be integrated to create an understanding of the external environment and help the body to react appropriately[1].
If not working correctly, each of the functions can have important clinical implications and all should be considered when working with patients. For example an important clinical association with the breakdown of the ability of the skin to provide protection is pressure sores.
Structure of the Skin[edit | edit source]
The skin is made up of two layers—the superficial epidermis and the deeper dermis.
Epidermis:
- Tough, outer layer that acts as the first line of defense against the external environment
- Regenerates from stem cells located in the basal layer that grow up towards the corneum. The epidermis itself is devoid of blood supply and derives its nutrition from the underlying dermis
Composed of stratified squamous epithelial cells that further break down into four to five layers (see image R). From superficial to deep, the primary layers are the
- Stratum corneum
- Stratum granulosum
- Stratum spinosum
- Stratum basale
- In the palms and soles where the skin is thicker, there is an additional layer of skin between the stratum corneum and stratum granulosum called the stratum lucidum.
Dermis
- Underlying connective tissue framework that supports the epidermis
- The dermis as a whole contains blood and lymph vessels, nerves, sweat glands, hair follicles, and various other structures embedded within the connective tissue.
Further subdivides into two layers
- Superficial papillary dermis - forms finger-like projections into the epidermis, known as dermal papillae, and consists of highly vascularized, loose connective tissue.
- Deep reticular layer - has dense connective tissue that forms a strong network[1].
Links to other Areas or Topics to Consider[edit | edit source]
- Burns
- Pressure Sores
- Pain
- Skin Grafts
- Trauma
- Diabetes Mellitus
- Corticosteroids and other medications
- Patient interaction
- Psychological impact of skin disorders
Other Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Kim JY, Dao H. Physiology, Integument. InStatPearls [Internet] 2020 Feb 17. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK554386/ (last accessed 23.10.2020)
- ↑ 2.0 2.1 2.2 Martini FH, Nath, JL. Fundamentals of Anatomy and Physiology. 8th ed. Pearson. San Francisco: Benjamin Cummings. 2009
- ↑ Turkington C, Dover JS. Skin Deep. 3rd ed. New York: Checkmark Books. 2007
- ↑ Tortora GJ, Derrickson BH. Principles of Anatomy and Physiology: Organisation, Support and Movement and Control Systems of the Human Body. Volume 1. 12th ed. Hoboken: John Wiley and Sons. 2009
- ↑ National Library of Medicine. Medical Subject Headings (MESH) http://www.nlm.nih.gov/cgi/mesh/2011/MB_cgi?modeterm=Integumentary+System (accessed 11 June 2013)
- ↑ Mclafferty E Hendry C Farley A. The integumentary system: anatomy, physiology and function of skin. Nursing Standard 2010;27:35-42.
- ↑ Martini FH, Nath, JL. Fundamentals of Anatomy and Physiology. 8th ed. Pearson. San Francisco: Benjamin Cummings. 2009