Injury and Healing Within Sports Physiotherapy
Top Contributors - Wanda van Niekerk, Robin Tacchetti, Lucinda hampton, Kim Jackson, Jess Bell, Tarina van der Stockt and Ewa Jaraczewska
Introduction[edit | edit source]
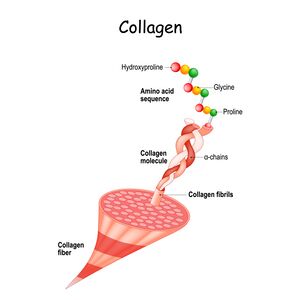
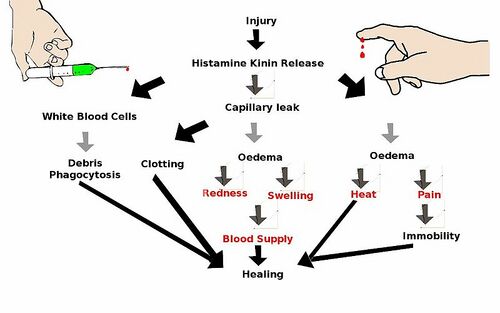
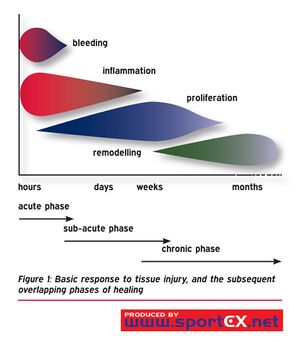
Soft tissues provide support and protective function in the body. These tissues are made of cells, fibres and non-cellular matrix material with collagen being the most abundant component. When soft tissue has been injured, the cardinal signs of inflammation occurs: redness, swelling, pain, loss of motion and heat.[1][2] Healing is a process of moving through stages of inflammation, repair and lastly to remodelling. Each phase of healing overlaps and has no definitive time frame.[3]
Connective Tissue[edit | edit source]
As physiotherapists involved in the prevention and management of sports injuries it is important to understand the biological and mechanical nature of tendons, ligaments and capsules (collectively these are known as connective tissue). Two important functions of connective tissue are:
- protect
- support
Three elements are found in all connective tissues, namely cells, fibres and extra-cellular matrix. Collagen is the most typical fibre in connective tissues and is composed of smaller units called tropocollagen. There are many types of collagen and each have different properties. Tendons are mainly made up of type I collagen. Collagen resists elongation and stress whereas the extracellular matrix resists compression. Components of the extracellular matrix include:
- proteoglycans
- collagen fibrils
- ground substance
- tissue fluid
- non-collagen glycoprotein
Different types of tissue in the body are all derived from one basic cell, but differentiate into specialised cells based on the stimulus that is provided.[4] The mechanical behaviour of these different types of tissues is influenced by:
- the physical properties of collagen and other fibres[4]
- arrangement of fibres[4]
- size of collagen fibres
- proportion of collagen fibres and other fibres
- maturity of collagen fibres
- composition and hydration status of ground substance
Stages of Healing[edit | edit source]
Inflammatory Phase[edit | edit source]
The first stage injured soft tissue undergoes is inflammation. This phase, which generally peaks between day 1-3 is marked by redness, swelling, pain, heat and disruption of function of the affected tissue.[1] The purpose of the inflammatory phase is to[1]:
- control the effects of the injury
- return the injured tissue to its normal state
The aim during this time period is to prevent excessive inflammation and move through the next stages of healing to full recovery.[5]
Physiologically the inflammatory process consists of the following events:
- Histamine is released from damaged capillaries causing increased permeability and vessel dilation
- Prostaglandins maintain vasodilation
- Amines cause contraction of smooth muscle
- Phagocytes clear debris
- Mediators are released to stimulate proliferative phase[5]
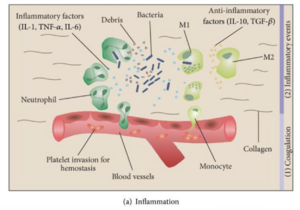
Inflammation can be seen as unwelcome, but it is the first step to healing. The inflammatory phase prepares the tissue for the repair process. This chemically controlled cascade is crucial for healing and optimal soft tissue regeneration is supported by this process. The use of NSAIDs during this crucial phase may negatively affect long-term tissue healing.[7][8]
When it becomes excessive there are treatments designed to limit the above chemical process. There are two drug classes used to inhibit the inflammatory process; non-steroidal (NSAIDs) and corticosteroids. NSAIDs not only have anti-inflammatory properties but are pain-relieving as well. Corticosteroids are usually injected to the site of pathology and can reduce inflammation and pain, but can cause inhibition of collagen synthesis affecting healing. [5]
Chronic Inflammation[edit | edit source]
Inflammation that continues on for several months to several years is referred to as chronic inflammation.[9] This phenomenon occurs when macrophages have been unable to clear the wounded area of foreign substances. This area becomes surrounded with collagen/scar to isolate it from the body called a granuloma.[5] [9]
Proliferation Phase[edit | edit source]
Once the inflammatory process is complete, tissue repair can occur. This phase consists of two actions, fibroplasia (fibrous material production) and angiogenesis (new blood vessel formation).[5]
Physiologically during this phase, the following occurs:
- Capillary buds form and grow towards the injured area
- Granulation tissue is created by capillary loops initiating blood flow
- Phagocytosis by specialized white blood cells
- Lymphatic vessels create a new drainage system
- Fibroblasts contract wound pulling edges towards each other[9]
Remodelling[edit | edit source]
The remodelling stage may last anywhere from 3 weeks to 12 months and overlaps the repair stage. The aim of remodelling is to decrease wound size, increase the scar strength and alter the direction of collagen fibres. Refining and altering collagen during this time facilitates increased fibre strength.[5] Physiologically the following occurs during this phase:
- Contraction of granulation tissue
- Fibroblasts form intercellular bonds
- Crossbonds between cells form increasing collagen strength
- Continuous turnover of collagen[9]
- Type three collagen is replaced by type one collagen[6]
The final collagen fibre tissue arrangement should match the function of the tissue. The alignment is dependent on stress imposed on the tissue during healing.[9]
Healing[edit | edit source]
Healing begins immediately, however collagen is generally not laid down until the 5th day post-injury. This period of time is referred to as the “lag phase”. During lag time, physiotherapy goals are directed toward oedema control and resolving pain. The graph on the right shows how the different phases of healing are not discrete and that they overlap.
Tissue mobilisation focused on realigning collagen fibres can begin once collagen synthesis has been initiated. Mild stress during this stage of rehabilitation is referred to as mechanical loading and is necessary to stimulate collagen fibre alignment.[9]
Mechanical Loading[edit | edit source]
Physiotherapists can play a key role in optimally influencing the healing process. The overall therapeutic aim of any stimulus is to affect two major processes:
- repair of the injured tissue
- adaptation of the tissue to load (or training stimulus in athletes)
Macro trauma (like an impact or collision injury in sports) or microtrauma (like an overuse injury) will elicit a tissue response. A corrective or adaptive load is necessary for the resolution of an injury.[3]
The goal of mechanical loading is to improve injured tissue tensile strength through compression, tension or shear force.[9] A load can be very light like a tickle, to a very high load like a manipulation.[3] If the load applied is too little or too much, it can result in a substandard repair and potentially lead to a chronic condition. As the tissue strengthens, the applied load can be enhanced by being cautious not to overload.[9] Too much tension can cause the collagen fibres to misalign developing adhesions leading to a regression of the inflammatory process.[3] [9]The video below provides a simple explanation of the relationship between load and tissue capacity and how this links to injury.
Read more on how mechanical load stimulates adaptation in this article (see Figure 1 in article):
Understanding Mechanobiology: Physical Therapists as a Force in Mechanotherapy and Musculoskeletal Regenerative Rehabilitation[11]
Physio Loading
Physiotherapists can apply mechanical loads to injured tissues with different techniques such as massage, ultrasound and exercise.[9] [3] These interventions promote repair and remodelling of injured tissues.[9] An indicator that the tissue is being stimulated and remodelled is the patient will feel mild discomfort. One example of mechanical loading is deep transverse friction massage which may improve adhesions and increase the tensile strength of the healing scar.[9] Please see the below video for an example of deep transverse friction massage by Ben Benjamin:
Loading Feedback[edit | edit source]
Patient feedback is critical during this stage to ensure collagen alignment and proper healing. Asking the patient to monitor for swelling, stiffness and pain for 24 hours can help the therapist gauge the correct loading intensity. In addition, therapists can monitor swelling using girth measurements.[3] See below for an example of a girth measurement of the ankle by CRT Technologies:
Summary Soft Tissue Injury[edit | edit source]
Traditional Acute Injury Management[edit | edit source]
Traditional treatment for soft tissue injury as been referred to as RICE, rest, ice, compression and elevation. Unfortunately, rest or immobilisation of soft tissue injury can result in joint stiffness, weak ligaments and delayed healing. Total immobilisation should be dedicated to bone injury or a complete rupture where movement could cause further damage. Conversely, exercise and pain-free movement within a protected support can strengthen ligaments and increase collagen turnover.[9] [7]
New thoughts on Acute Injury Management[edit | edit source]
Contemporary acronyms for soft tissue injury management is referred to as PEACE and LOVE[14]. See below for a better understanding of the various steps:
PEACE (day 1-3)
P: protect the area
E: elevate
A: avoid anti-inflammatories medication to allow for natural inflammatory process to occur
C: compression
E: educate the patient on an active approach to therapy versus a passive one[14]
LOVE (after a few days)
L: optimal loading to repair and remodel tissue
O: optimistic expectations by the patient coincide with better outcome
V: vascularization- pain-free aerobic exercise to increase blood flow
E: exercise- pain-free exercise[14]
Healing Times[edit | edit source]
With proper management, various tissues will take different amounts of time to heal fully. Understanding the specific tissue helps target the appropriate timing for incremental loading during the remodeling stage.[3] Ian Horsley[3] estimates the time expected to fully heal by tissue below:
Muscle: 6 months
Ligament: 1 year
Tendon: 2-3 years
Articular cartilage: greater than 3 years
Soft tissues need to go through the three stages of inflammatory, repair and remodel to fully heal. Physiotherapists can assist with healing by not only understanding the timeline of the involved tissue, but when and how much intensity to apply during the remodeling phase. Good clinical decision will be necessary to fine tune interventions and to monitor symptoms. All of these factors will provide for optimal soft tissue recovery.[3]
Resources[edit | edit source]
- Inflammation Acute and Chronic
- Wound Healing
- Figure Eight Measurement of the Hand
- Figure of Eight Method of Measuring Ankle Joint Swelling
- Peace and Love Principle
Reference[edit | edit source]
- ↑ 1.0 1.1 1.2 Basil MC, Levy BD. Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nature Reviews Immunology. 2016 Jan;16(1):51-67.
- ↑ Muire PJ, Mangum LH, Wenke JC. Time course of immune response and immunomodulation during normal and delayed healing of musculoskeletal wounds. Frontiers in immunology. 2020 Jun 4;11:1056.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Horsley, I. Injury and Healing in Sports Physiotherapy Course. Physioplus. 2022.
- ↑ 4.0 4.1 4.2 Muntz I, Fenu M, van Osch GJ, Koenderink GH. The role of cell–matrix interactions in connective tissue mechanics. Physical biology. 2022 Jan 18;19(2):021001.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Norris C. Sports and soft tissue injuries: A guide for students and therapists. Routledge; 2018 Sep 3.
- ↑ 6.0 6.1 Serra MB, Barroso WA, Silva NN, Silva SD, Borges AC, Abreu IC, Borges MO. From inflammation to current and alternative therapies involved in wound healing. International journal of inflammation. 2017 Oct;2017.
- ↑ 7.0 7.1 Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug 1;52(15):956-.
- ↑ Duchesne E, Dufresne SS, Dumont NA. Impact of inflammation and anti-inflammatory modalities on skeletal muscle healing: from fundamental research to the clinic. Physical therapy. 2017 Aug 1;97(8):807-17.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 Pahwa R, Goyal A, Bansal P, Jialal I. Chronic Inflammation. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. PMID: 29630225.
- ↑ British Journal of Sports Medicine (BJSM). Load vs Capacity and Injuries. Available from https://www.youtube.com/watch?v=H1rp_v4Dr3g&t=266s. (last accessed 25 February 2022)
- ↑ Thompson WR, Scott A, Loghmani MT, Ward SR, Warden SJ. Understanding mechanobiology: physical therapists as a force in mechanotherapy and musculoskeletal regenerative rehabilitation. Physical therapy. 2016 Apr 1;96(4):560-9.
- ↑ Ben Benjamin. Guidelines for Friction Therapy. Available from: https://www.youtube.com/watch?v=YezCxFFGJXQ&t=6s [last accessed 22/02/2022]
- ↑ CRT Technologies. Figure 8 Measurement. Available from: https://www.youtube.com/watch?v=cG-A3PbS5ow&t=3s [last accessed 22/02/2022]
- ↑ 14.0 14.1 14.2 Dubois B, Esculier JF. Soft-tissue injuries simply need PEACE and LOVE. British journal of sports medicine. 2020 Jan 1;54(2):72-3.