Implementation Science: Pre-Implementation Stage: Difference between revisions
(copying writeup over) |
No edit summary |
||
| Line 23: | Line 23: | ||
[[File:Implementation science box 1.png|center|thumb|800x800px|These key implementation challenges are based on the work of Leonard and colleagues in 2020]] | [[File:Implementation science box 1.png|center|thumb|800x800px|These key implementation challenges are based on the work of Leonard and colleagues in 2020]] | ||
== Resources | == Implementation Science Terms == | ||
* | Below are listed many terms that are used in the field of implementation science, please review and reflect upon these key implementation terms and definitions, as they are key thinking about facilitating the implementation of evidence-based rehabilitation interventions. | ||
* | [[File:Implementation science box 2.png|center|thumb|800x800px]] | ||
or | |||
== Understanding the Intervention == | |||
The questions in Box 3 were designed to encourage thought about evidence-based rehabilitation interventions, irrespective if it refers to adopting, implementing or sustaining a new rehabilitation intervention. | |||
[[File:Implementation science box 3.png|center|thumb|800x800px|Implementation facilitator questions that are key to exploring and understanding the intervention you want to implement ]] | |||
Rehabilitation intervention evidence is growing every day. Principles and guidance on rehabilitation interventions are increasingly available such as: | |||
# [https://www.england.nhs.uk/wp-content/uploads/2016/04/rehabilitation-comms-guid-16-17.pdf NHS Commissioning Guidance for Rehabilitation] | |||
# [https://www.who.int/rehabilitation/Package-of-rehab-interventions-info-sheet.pdf World Health Organization Package of Rehabilitation Interventions Information Sheet] | |||
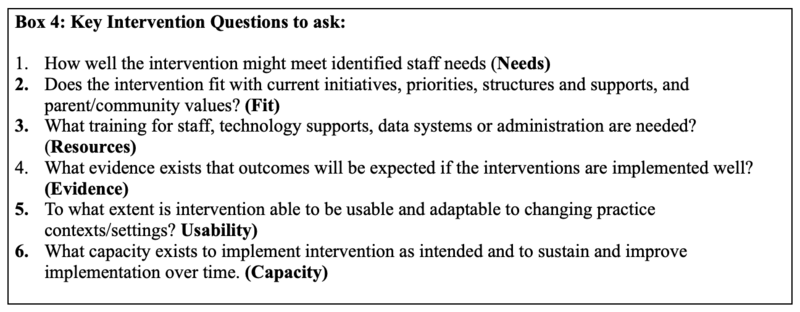
Despite the wealth of information, the uptake of this evidence into practice is a slow process, especially in lower-middle income countries. With so much available information, It is easy to become overwhelmed when deciding what interventions to implement. It is of great benefit to utilise using a comprehensive approach to explore and understand the intervention chosen to implement. This is done by focusing on six key intervention topics: | |||
# Needs | |||
# Fit | |||
# Resources | |||
# Evidence | |||
# Usability | |||
# Capacity | |||
[[File:Implementation science box 4.png|center|thumb|800x800px|Examples of key questions]] | |||
These SIX questions are based upon an existing Implementation Science exploration and planning tool that can also inform evaluation- the Hexagon Tool. | |||
== Hexagon Tool == | |||
== Understanding Context == | |||
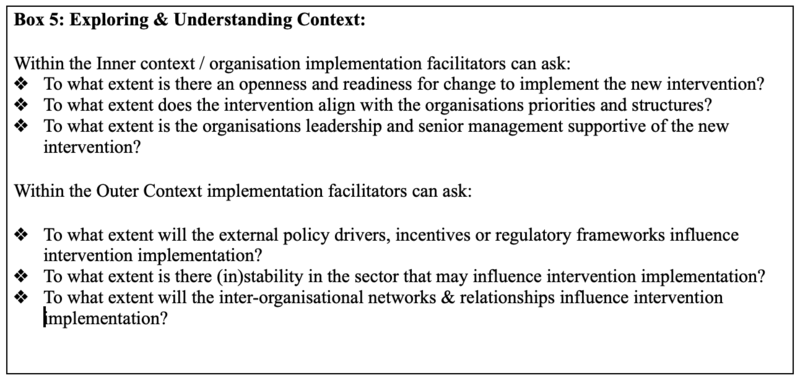
In implementation science the term ''context'' is used to describe and refer to all the potential factors or challenges that may influence adoption, effectiveness and sustainability of interventions. The questions in Box 5 were designed to encourage thinking about the context within which the evidence-based rehabilitation interventions is designed to help patients address the impact of physical, cognitive, psychosocial and mental health problems and conditions. | |||
[[File:Implementation science box 5.png|center|thumb|800x800px|Examples of implementation facilitator questions that are key to understanding the inner and outer context within which the intervention is to be implemented]] | |||
There are multiple contextual factors and levels (inner and outer) related to the organization that are instrumental to implementation. For example, the inner context is comprised of internal organization characteristics that drive implementation, such as the institution’s leadership, structures, resources, internal policies, staffing, practices, and provider factors (e.g., attitudes, beliefs). The outer context refers to the external environment that influences organizational implementation. These include policies outside the organization, consumers, relationships across organizations such as funding agencies, health departments, and advocacy groups. | |||
These inner and outer setting factors also interact with one another and the intervention itself (i.e., how it fits within the organization and culture) to influence implementation. Evidence is also building about ‘Bridging factors’ that refer to the relationships between the inner and outer contexts to guide implementation (e.g., academic-community partnerships). | |||
Given the increasing information about the Contextual challenges to implementing rehabilitation interventions it is easy to become overwhelmed when assessing what may be affected by the new implementation intervention. It is beneficial to use a more comprehensive approach to explore and understand the inner and outer contextual factors / challenges across the three implementation phases: Pre-Implementation, Implementation and Sustainment. | |||
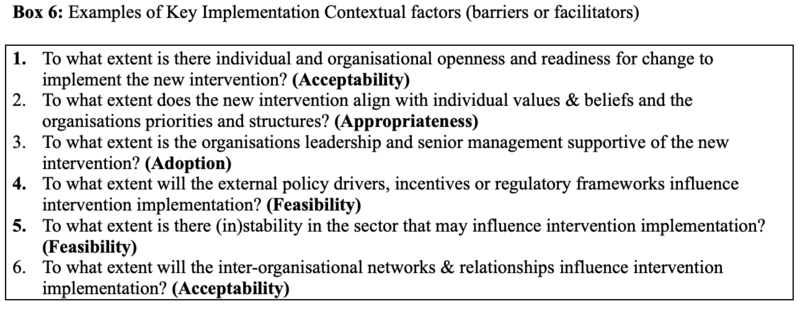
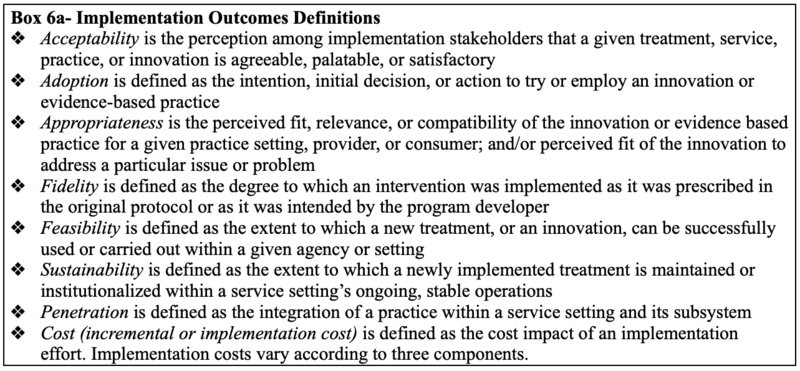
Box 6 provides examples of key inner and outer contextual factors (barriers or facilitators) at the individual and organisational level – framed as questions that are known to influence implementation outcomes, such as: feasibility, acceptability, appropriateness and fidelity of implementation. | |||
[[File:Implementation science box 6.png|center|thumb|800x800px|Examples of key implementation contextual factors]] | |||
These SIX questions are based upon several existing implementation science exploration and planning or determinants frameworks that can also inform evaluation. Listed below are commonly used implementation planning frameworks that can identify barriers and facilitators to key implementation outcomes, namely feasibility, acceptability, uptake, and fidelity.<blockquote>Please follow the listed links for more information on these implementation planning frameworks: | |||
* [https://cfirguide.org/ Consolidated Framework for Implementation Research] (CFIR) | |||
* [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0605-9 Theoretical Domains Framework] (TDF) | |||
* [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7310499/ Integrating Promoting Action on Research Implementation in Health Services] (iPARIHS) | |||
* [https://episframework.com/ Exploration, Preparation, Implementation and Sustainment] (EPIS) | |||
</blockquote> | |||
[[File:Implementation science box 6A.png|center|thumb|800x800px|Additional implementation outcome definitions]] | |||
== Stakeholders == | |||
In rehabilitation multiple key stakeholders are essential to the implementation process and can include: staff within a clinic or service, such as frontline rehabilitation professionals who deliver services; organisational managers and administration staff who support the delivery of rehabilitation services, clients who receive services, or staff external to the clinic or service such as policymakers who fund and make decisions that can support the implementation of interventions. | |||
Stakeholder engagement at the beginning and throughout the implementation process can enhance the acceptability of interventions to rehabilitation clients and providers and improve ''reach'' (the number of eligible people taking part in the intervention) and ''sustainability'' (changes over time in numbers of eligible people taking part in the intervention). | |||
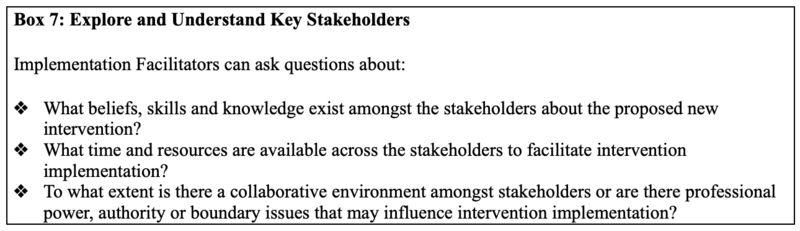
=== Understanding Key Stakeholders === | |||
It is important to understand the key stackholders, including their knowledge, beliefs and capacity to adopt them. | |||
[[File:Implementation science box 7.png|center|thumb|800x800px|Vital implementation facilitator questions for understanding the key stackholders]] | |||
The questions in Box 7 were designed to help understand the key Stakeholders who are key to implementing the evidence-based rehabilitation interventions, irrespective if it refers to adopting, implementing or sustaining a new rehabilitation intervention. | |||
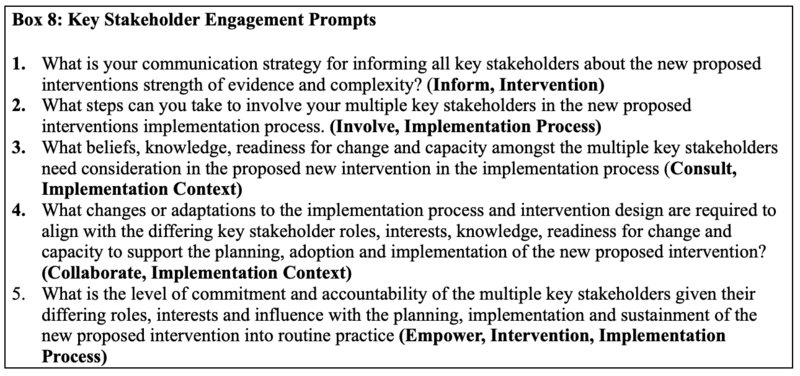
=== Engaging Key Stakeholders === | |||
Engaging key stakeholders is a critical part to successful implementation of evidence-based interventions. It is firstly important to recognise, that just as there are multiple stakeholders potentially key to implementation, the timing and nature of stakeholder engagement and engaging stakeholders across multiple levels of an implementation is recommended best practice for implementation. | |||
Engagement is a process, with differing phases that align and fit with the stakeholder’s differing roles, interests and influence and the implementation process itself. Stakeholders can be engaged by informing, involving, consulting, collaborating, or empowering them into the implementation process. These different levels or phases of engagement is based upon the [https://iap2.org.au/resources/spectrum/ International Association for Public Participation (IAP2) spectrum]. Thinking about stakeholder engagement in this way allows ofr the use an implementation science mindset to successfully engage multiple stakeholders across multiple levels of an implementation ecosystem (e.g., policy/legislative, funders, community, organizational, provider, client/patient). | |||
[[File:Implementation science box 8.png|alt=Key stakeholder engagement prompts|center|thumb|800x800px]] | |||
These five questions are based upon the International Association of Public Participation (IAP2) stakeholder engagement framework and the CFIR framework. | |||
== Conclusion == | |||
The pre-implementation stage of implementation science uses a comprehensive approach to explore and understand the intervention to be implemented in a given situation. This stage focusses on six key intervention topics: needs, fit, resources, evidence, usability and capacity to implement. | |||
Given the multiple challenges to implementing rehabilitation interventions, a comprehensive approach is needed to explore and understand the inner (organisational setting) and outer (external to the organisation) factors across the implementation phases: Pre-Implementation, Implementation and Sustainment. | |||
It is essential to consider who is needed to engage in what is implemented, and that by engaging the key stakeholders throughout the implementation process can enhance the acceptability, reach and sustainability of interventions to rehabilitation clients. | |||
== Resources == | |||
** PDF of Hexagon Tool handout [[/nirn.fpg.unc.edu/sites/nirn.fpg.unc.edu/files/imce/documents/NIRN Hexagon Discussion Analysis Tool September2020 1.pdf|https://nirn.fpg.unc.edu/sites/nirn.fpg.unc.edu/files/imce/documents/NIRN%20Hexagon%20Discussion%20Analysis%20Tool_September2020_1.pdf]] | |||
** Leonard et al 2020. Barriers and facilitators to implementing evidence-based health innovations in low- and middle-income countries: A systematic literature review. Evaluation and Program Planning. 82: 101832. file:///Users/lucio/Downloads/1-s2.0-S0149718920301361-main.pdf | |||
** Pare´ et al (2020). Clinicians’ perceptions of organizational readiness for change in the context of clinical information system projects: insights from two cross-sectional surveys. Implement Sci [Internet]. 2011 Feb 28 [cited 2017 Oct 2]; 6(1):15. [[/www.ncbi.nlm.nih.gov/pmc/articles/PMC3056827/pdf/1748-5908-6-15.pdf|https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056827/pdf/1748-5908-6-15.pdf]] | |||
** Holcomb et al (2021). Stakeholder Engagement in Adoption, Implementation, and Sustainment of an Evidence-Based Intervention to Increase Mammography Adherence Among Low-Income Women. Journal of Cancer Education. [[/link.springer.com/content/pdf/10.1007/s13187-021-01988-2.pdf|https://link.springer.com/content/pdf/10.1007/s13187-021-01988-2.pdf]] | |||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 04:27, 24 April 2022
Top Contributors - Stacy Schiurring, Tarina van der Stockt, Jess Bell and Kim Jackson
Introduction[edit | edit source]
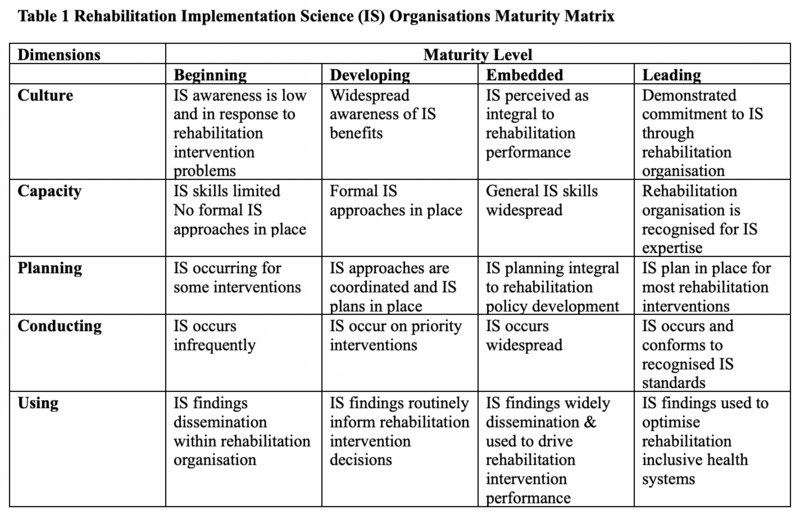
As rehabilitation is recognised as a complex multi-disciplinary process with many moving parts, within complex multi-level healthcare systems and involving multiple professionals, patients, families and carers (Morris 2019) pre-implementation efforts are important than ever. Adopting, implementing or sustaining any new rehabilitation interventions is challenging. Have you ever wondered why some professionals seem to adopt these interventions more easily, when others do not and why does this intervention work in some settings and not in others? When rehabilitation professionals implement new interventions in lower middle-income countries, they can experience a wide range of challenges at a systems, health care provider and or at a patient level. While many implementation challenges exist, implementation science can provide a way of thinking about these challenges and can facilitate implementation efforts.
This article can serve as a guide on how to plan implementation process efforts to adopt, adapt, spread or sustain new interventions.
Building Implementation Science Capability[edit | edit source]
The need to build implementation science expertise is recognised as urgently required to bridge the gap between evidence and practice, particularly in resource-poor or lower middle income countries (LMICs) (Alonge et al 2019, Ridde 2020, Semeere et al 2021)
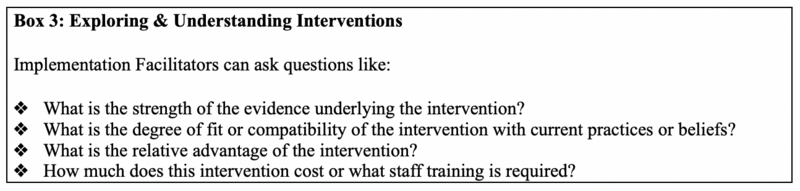
All rehabilitation leaders and stakeholders and their organisations have differing implementation science capability it is important to reflect upon the implementation science maturity of an organisation to establish a baseline, then set about identifying implementation science strengths, gaps, readiness and priorities.
Challenges to Implementing Evidenced-based Interventions in LMICs[edit | edit source]
Please read this page to review the challenges of implementing evidence-based rehabilitation interventions that are known to exist in LMICs.
Challenges exist at a:
- System level: lack of specific government policy, strategic planning, legislation and funding for rehabilitation services across all health system level
- Healthcare provider level: limited rehabilitation workforce, capacity, competing priorities and heavy workloads
- Patient level: knowledge and attitudes about interventions
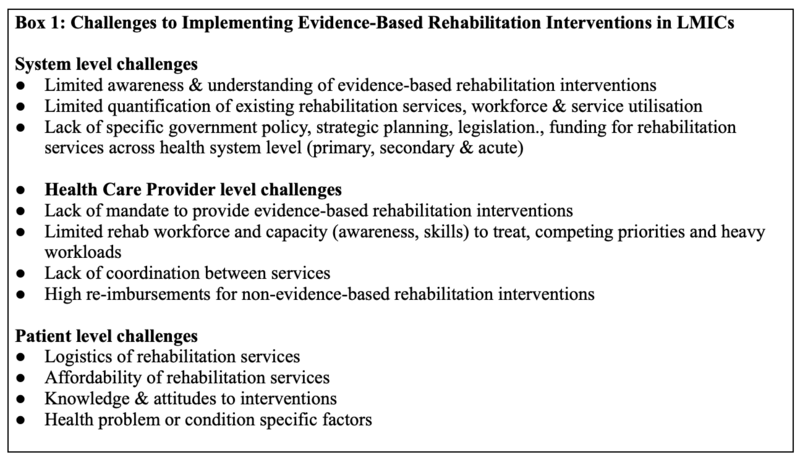
Implementation Science Terms[edit | edit source]
Below are listed many terms that are used in the field of implementation science, please review and reflect upon these key implementation terms and definitions, as they are key thinking about facilitating the implementation of evidence-based rehabilitation interventions.
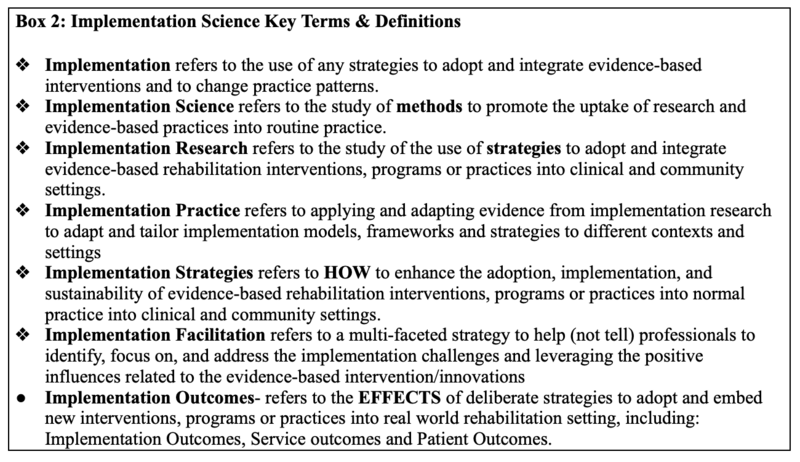
Understanding the Intervention[edit | edit source]
The questions in Box 3 were designed to encourage thought about evidence-based rehabilitation interventions, irrespective if it refers to adopting, implementing or sustaining a new rehabilitation intervention.
Rehabilitation intervention evidence is growing every day. Principles and guidance on rehabilitation interventions are increasingly available such as:
- NHS Commissioning Guidance for Rehabilitation
- World Health Organization Package of Rehabilitation Interventions Information Sheet
Despite the wealth of information, the uptake of this evidence into practice is a slow process, especially in lower-middle income countries. With so much available information, It is easy to become overwhelmed when deciding what interventions to implement. It is of great benefit to utilise using a comprehensive approach to explore and understand the intervention chosen to implement. This is done by focusing on six key intervention topics:
- Needs
- Fit
- Resources
- Evidence
- Usability
- Capacity
These SIX questions are based upon an existing Implementation Science exploration and planning tool that can also inform evaluation- the Hexagon Tool.
Hexagon Tool[edit | edit source]
Understanding Context[edit | edit source]
In implementation science the term context is used to describe and refer to all the potential factors or challenges that may influence adoption, effectiveness and sustainability of interventions. The questions in Box 5 were designed to encourage thinking about the context within which the evidence-based rehabilitation interventions is designed to help patients address the impact of physical, cognitive, psychosocial and mental health problems and conditions.
There are multiple contextual factors and levels (inner and outer) related to the organization that are instrumental to implementation. For example, the inner context is comprised of internal organization characteristics that drive implementation, such as the institution’s leadership, structures, resources, internal policies, staffing, practices, and provider factors (e.g., attitudes, beliefs). The outer context refers to the external environment that influences organizational implementation. These include policies outside the organization, consumers, relationships across organizations such as funding agencies, health departments, and advocacy groups.
These inner and outer setting factors also interact with one another and the intervention itself (i.e., how it fits within the organization and culture) to influence implementation. Evidence is also building about ‘Bridging factors’ that refer to the relationships between the inner and outer contexts to guide implementation (e.g., academic-community partnerships).
Given the increasing information about the Contextual challenges to implementing rehabilitation interventions it is easy to become overwhelmed when assessing what may be affected by the new implementation intervention. It is beneficial to use a more comprehensive approach to explore and understand the inner and outer contextual factors / challenges across the three implementation phases: Pre-Implementation, Implementation and Sustainment.
Box 6 provides examples of key inner and outer contextual factors (barriers or facilitators) at the individual and organisational level – framed as questions that are known to influence implementation outcomes, such as: feasibility, acceptability, appropriateness and fidelity of implementation.
These SIX questions are based upon several existing implementation science exploration and planning or determinants frameworks that can also inform evaluation. Listed below are commonly used implementation planning frameworks that can identify barriers and facilitators to key implementation outcomes, namely feasibility, acceptability, uptake, and fidelity.
Please follow the listed links for more information on these implementation planning frameworks:
Stakeholders[edit | edit source]
In rehabilitation multiple key stakeholders are essential to the implementation process and can include: staff within a clinic or service, such as frontline rehabilitation professionals who deliver services; organisational managers and administration staff who support the delivery of rehabilitation services, clients who receive services, or staff external to the clinic or service such as policymakers who fund and make decisions that can support the implementation of interventions.
Stakeholder engagement at the beginning and throughout the implementation process can enhance the acceptability of interventions to rehabilitation clients and providers and improve reach (the number of eligible people taking part in the intervention) and sustainability (changes over time in numbers of eligible people taking part in the intervention).
Understanding Key Stakeholders[edit | edit source]
It is important to understand the key stackholders, including their knowledge, beliefs and capacity to adopt them.
The questions in Box 7 were designed to help understand the key Stakeholders who are key to implementing the evidence-based rehabilitation interventions, irrespective if it refers to adopting, implementing or sustaining a new rehabilitation intervention.
Engaging Key Stakeholders[edit | edit source]
Engaging key stakeholders is a critical part to successful implementation of evidence-based interventions. It is firstly important to recognise, that just as there are multiple stakeholders potentially key to implementation, the timing and nature of stakeholder engagement and engaging stakeholders across multiple levels of an implementation is recommended best practice for implementation.
Engagement is a process, with differing phases that align and fit with the stakeholder’s differing roles, interests and influence and the implementation process itself. Stakeholders can be engaged by informing, involving, consulting, collaborating, or empowering them into the implementation process. These different levels or phases of engagement is based upon the International Association for Public Participation (IAP2) spectrum. Thinking about stakeholder engagement in this way allows ofr the use an implementation science mindset to successfully engage multiple stakeholders across multiple levels of an implementation ecosystem (e.g., policy/legislative, funders, community, organizational, provider, client/patient).
These five questions are based upon the International Association of Public Participation (IAP2) stakeholder engagement framework and the CFIR framework.
Conclusion[edit | edit source]
The pre-implementation stage of implementation science uses a comprehensive approach to explore and understand the intervention to be implemented in a given situation. This stage focusses on six key intervention topics: needs, fit, resources, evidence, usability and capacity to implement.
Given the multiple challenges to implementing rehabilitation interventions, a comprehensive approach is needed to explore and understand the inner (organisational setting) and outer (external to the organisation) factors across the implementation phases: Pre-Implementation, Implementation and Sustainment.
It is essential to consider who is needed to engage in what is implemented, and that by engaging the key stakeholders throughout the implementation process can enhance the acceptability, reach and sustainability of interventions to rehabilitation clients.
Resources[edit | edit source]
- PDF of Hexagon Tool handout https://nirn.fpg.unc.edu/sites/nirn.fpg.unc.edu/files/imce/documents/NIRN%20Hexagon%20Discussion%20Analysis%20Tool_September2020_1.pdf
- Leonard et al 2020. Barriers and facilitators to implementing evidence-based health innovations in low- and middle-income countries: A systematic literature review. Evaluation and Program Planning. 82: 101832. file:///Users/lucio/Downloads/1-s2.0-S0149718920301361-main.pdf
- Pare´ et al (2020). Clinicians’ perceptions of organizational readiness for change in the context of clinical information system projects: insights from two cross-sectional surveys. Implement Sci [Internet]. 2011 Feb 28 [cited 2017 Oct 2]; 6(1):15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056827/pdf/1748-5908-6-15.pdf
- Holcomb et al (2021). Stakeholder Engagement in Adoption, Implementation, and Sustainment of an Evidence-Based Intervention to Increase Mammography Adherence Among Low-Income Women. Journal of Cancer Education. https://link.springer.com/content/pdf/10.1007/s13187-021-01988-2.pdf