Hypokalemia: Difference between revisions
No edit summary |
No edit summary |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
One of the most common electrolyte disturbances seen in clinical practice is hypokalemia. Hypokalemia is | One of the most common [[Electrolytes|electrolyte]] disturbances seen in clinical practice is hypokalemia. Hypokalemia is an [[Electrolytes|electrolyte]] imbalance that is lower than normal level of potassium in the bloodstream.<ref name=":0">Castro D, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK482465/ Hypokalemia]. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/<nowiki/>(accessed 18.9.2021)</ref>The most common cause is excessive potassium loss in [[urine]] due to [[diuretics]], often prescribed for people who have [[hypertension]] or [[Heart Failure|heart disease]]<ref name=":2">Mayo clinic Hypokalemia Available:https://www.mayoclinic.org/symptoms/low-potassium/basics/causes/SYM-20050632?p=1 (accessed 3.6.2022)</ref>. | ||
* A normal blood potassium is 3.6 to 5.2 mmol/L. | * A normal blood potassium is 3.6 to 5.2 mmol/L. | ||
* Severe and life threatening hypokalemia level is known as <2.5mmol/L. <ref name="mayo">Low Potassium(hypokalemia)[Internet]. 2012 August 10 [cited 2013 March 27] Available from:http://www.mayoclinic.com/health/low-potassium/MY00760</ref> | * Severe and life threatening hypokalemia level is known as <2.5mmol/L. <ref name="mayo">Low Potassium(hypokalemia)[Internet]. 2012 August 10 [cited 2013 March 27] Available from:http://www.mayoclinic.com/health/low-potassium/MY00760</ref> | ||
Potassium helps | Potassium helps carry electrical signals to cells in your body. It is critical to the proper functioning of [[Neurone|nerve]] and [[Muscle Cells (Myocyte)|muscles cells]], particularly [[Muscle: Cardiac|heart muscle cells]]<ref name=":2" />. | ||
Few people meet the daily recommended potassium intake (3,400 mg for men and 2,600 mg for women), however hypokalemia is rarely caused by dietary deficiency alone. It can be caused by a number of factors, including fluid loss, [[malnutrition]], [[shock]], using certain medications, and medical conditions eg [[Chronic Kidney Disease|kidney failure]].<ref name=":1">Healthline Hypokalemia Available: https://www.healthline.com/nutrition/potassium-deficiency-symptoms#bottom-line (accessed 3.6.2022)</ref> | |||
== Etiology == | == Etiology == | ||
Potential etiologies resulting in hypokalemia are put into the following categories: | |||
# Decreased potassium intake | # Decreased potassium intake | ||
# Transcellular shifts (increased intracellular uptake) | # Transcellular shifts (increased intracellular uptake) | ||
# Increased potassium loss (skin, gastrointestinal, and renal losses)<ref name=":0" /> | # Increased potassium loss ([[skin]], gastrointestinal, and [[Kidney|renal]] losses)<ref name=":0" /> | ||
Certain illnesses or other factors more likely the cause of hypokalemia, these include: | |||
* Chronic diarrhea. | |||
* Certain medications. eg diuretics, beta 2-agonists, theophylline, [[insulin]], [[Corticosteroid Medication|corticosteroids]], and [[antibiotics]] | |||
[[ | * Eating disorders. eg [[Anorexia Nervosa|anorexia nervosa,]] refeeding syndrome, purging, laxative abuse. | ||
* [[Cushing's Syndrome|Cushing’s syndrome]] | |||
* Hyperaldosteronism. | |||
* Kidney failure and Kidney disorders. | |||
* [[Hypomagnesemia]]. | |||
* Overconsumption of licorice | |||
* Excessive sweating | |||
== Signs and Symptoms == | |||
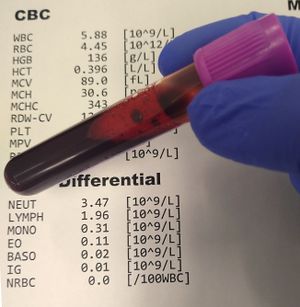
[[File:Blood test.jpg|thumb|Blood test]] | |||
In most cases, low potassium is found by a [[Blood Tests|blood test]] that is done because of an illness, or because of diuretics use. It is rare for low potassium to cause isolated symptoms. | |||
Hypokalemia symptoms may include: | |||
* Weakness | |||
* | * Fatigue | ||
* | * Muscle cramps | ||
* | * Constipation | ||
Abnormal heart rhythms ([[Heart Arrhythmias: Assessment|arrhythmias]]) are the most worrisome complication of very low potassium levels, particularly in people with underlying heart disease<ref>Mayo Clinic [https://www.mayoclinic.org/symptoms/low-potassium/basics/when-to-see-doctor/sym-20050632 Hypokalemia] Available: https://www.mayoclinic.org/symptoms/low-potassium/basics/when-to-see-doctor/sym-20050632 (accessed 19.9.2021)</ref>. | |||
== Diagnosis == | |||
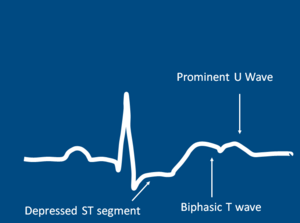
[[File:Hypokalemia.png|alt=|thumb|ECG Pattern Of Hypokalemia]]Hypokalemia is commonly found in a blood test, with <3.5mmol/L as mild hypokalemia and <2.5mmol/L as severe hypokalmia.<ref name="mayo" /> | |||
In severe cases, a 12-lead [[electrocardiogram]] may be necessary if to check for [[Heart Arrhythmias|cardiac arrythymias]]. Findings such as T-wave flattening or prominent U waves will result in hospital admission.<ref name="clinical">Hypokalemia [Internet]. 2012 [cited 2013 March 27] Available from:https://www.clinicalkey.com/topics/nephrology/hypokalemia.html#720089</ref> Other tests may include: | |||
*[[Arterial Blood Gases|Arterial blood gas]] | |||
*Basic or comprehensive metabolic panel | |||
| | |||
Blood tests will also be administered to check the following: glucose; magnesium; calcium; sodium; phosphorus; thyroxine; aldosterone levels.<ref name="medline">Hypokalemia [Internet]. 2013 March 22 [cited 2013 March 27] Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000479.htm</ref> | |||
== Management == | == Management == | ||
[[File:Magnesium Sulfate IV 1.jpg|thumb|Magnesium Sulfate IV]] | |||
The overarching goals of therapy for hypokalemia are to prevent or treat life-threatening complications, replace the potassium deficit, and to diagnose and correct the underlying cause.<ref name=":0" /> | The overarching goals of therapy for hypokalemia are to prevent or treat life-threatening complications, replace the potassium deficit, and to diagnose and correct the underlying cause.<ref name=":0" /> | ||
Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.<ref>Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ Hypokalemia: a clinical update. Endocrine connections]. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)</ref> | Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in [[Endocrine Disorders|endocrine]] related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.<ref>Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ Hypokalemia: a clinical update. Endocrine connections]. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)</ref> | ||
* Though diet alone usually will not resolve hypokalemia, it’s still beneficial to increase intake of potassium-rich foods, like fruits, vegetables, beans, and nuts<ref name=":1" />. | |||
* The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.<ref name="medline" /> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
Hypokalemia is not managed primarily by a physical therapist. Physical therapists should be mindful of common signs of symptoms of hypokalemia when working with patients. | Hypokalemia is not managed primarily by a physical therapist. Physical therapists should be mindful of common signs of symptoms of hypokalemia when working with patients. | ||
* Potassium levels < 3.2 mEq/L is contraindicated for physical therapy intervention due to the potential for arrhythmia . Due to muscle weakness and cramping, exercise is not effective during the state of hypokalemia. | * Potassium levels < 3.2 mEq/L is contraindicated for physical therapy intervention due to the potential for arrhythmia . Due to muscle weakness and cramping, [[Therapeutic Exercise|exercise]] is not effective during the state of hypokalemia. | ||
* Patients should be monitored for potassium levels in order to determine the appropriate time to participate in Physical Therapy.<ref name="Goodman">Goodman CC. Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641</ref> | * Patients should be monitored for potassium levels in order to determine the appropriate time to participate in Physical Therapy.<ref name="Goodman">Goodman CC. Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641</ref> | ||
| Line 126: | Line 72: | ||
* Bartter syndrome | * Bartter syndrome | ||
* Hyperthyroidism and thyrotoxicosis | * [[Hyperthyroidism]] and thyrotoxicosis | ||
* Hypocalcemia | * [[Hypocalcemia]] | ||
* Hypochloremic alkalosis | * Hypochloremic alkalosis | ||
* Hypomagnesemia | * [[Hypomagnesemia]] | ||
* Iatrogenic Cushing syndrome | * Iatrogenic [[Cushing's Syndrome|Cushing syndrome]] | ||
* Metabolic alkalosis<br> | * Metabolic alkalosis<br> | ||
Latest revision as of 05:44, 3 June 2022
Original Editors - Kara Lawless from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kara Lawless, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, Wendy Walker and WikiSysop
Introduction[edit | edit source]
One of the most common electrolyte disturbances seen in clinical practice is hypokalemia. Hypokalemia is an electrolyte imbalance that is lower than normal level of potassium in the bloodstream.[1]The most common cause is excessive potassium loss in urine due to diuretics, often prescribed for people who have hypertension or heart disease[2].
- A normal blood potassium is 3.6 to 5.2 mmol/L.
- Severe and life threatening hypokalemia level is known as <2.5mmol/L. [3]
Potassium helps carry electrical signals to cells in your body. It is critical to the proper functioning of nerve and muscles cells, particularly heart muscle cells[2].
Few people meet the daily recommended potassium intake (3,400 mg for men and 2,600 mg for women), however hypokalemia is rarely caused by dietary deficiency alone. It can be caused by a number of factors, including fluid loss, malnutrition, shock, using certain medications, and medical conditions eg kidney failure.[4]
Etiology[edit | edit source]
Potential etiologies resulting in hypokalemia are put into the following categories:
- Decreased potassium intake
- Transcellular shifts (increased intracellular uptake)
- Increased potassium loss (skin, gastrointestinal, and renal losses)[1]
Certain illnesses or other factors more likely the cause of hypokalemia, these include:
- Chronic diarrhea.
- Certain medications. eg diuretics, beta 2-agonists, theophylline, insulin, corticosteroids, and antibiotics
- Eating disorders. eg anorexia nervosa, refeeding syndrome, purging, laxative abuse.
- Cushing’s syndrome
- Hyperaldosteronism.
- Kidney failure and Kidney disorders.
- Hypomagnesemia.
- Overconsumption of licorice
- Excessive sweating
Signs and Symptoms[edit | edit source]
In most cases, low potassium is found by a blood test that is done because of an illness, or because of diuretics use. It is rare for low potassium to cause isolated symptoms.
Hypokalemia symptoms may include:
- Weakness
- Fatigue
- Muscle cramps
- Constipation
Abnormal heart rhythms (arrhythmias) are the most worrisome complication of very low potassium levels, particularly in people with underlying heart disease[5].
Diagnosis[edit | edit source]
Hypokalemia is commonly found in a blood test, with <3.5mmol/L as mild hypokalemia and <2.5mmol/L as severe hypokalmia.[3]
In severe cases, a 12-lead electrocardiogram may be necessary if to check for cardiac arrythymias. Findings such as T-wave flattening or prominent U waves will result in hospital admission.[6] Other tests may include:
- Arterial blood gas
- Basic or comprehensive metabolic panel
Blood tests will also be administered to check the following: glucose; magnesium; calcium; sodium; phosphorus; thyroxine; aldosterone levels.[7]
Management[edit | edit source]
The overarching goals of therapy for hypokalemia are to prevent or treat life-threatening complications, replace the potassium deficit, and to diagnose and correct the underlying cause.[1]
Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.[8]
- Though diet alone usually will not resolve hypokalemia, it’s still beneficial to increase intake of potassium-rich foods, like fruits, vegetables, beans, and nuts[4].
- The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.[7]
Physical Therapy Management[edit | edit source]
Hypokalemia is not managed primarily by a physical therapist. Physical therapists should be mindful of common signs of symptoms of hypokalemia when working with patients.
- Potassium levels < 3.2 mEq/L is contraindicated for physical therapy intervention due to the potential for arrhythmia . Due to muscle weakness and cramping, exercise is not effective during the state of hypokalemia.
- Patients should be monitored for potassium levels in order to determine the appropriate time to participate in Physical Therapy.[9]
Differential Diagnosis[edit | edit source]
- Bartter syndrome
- Hyperthyroidism and thyrotoxicosis
- Hypocalcemia
- Hypochloremic alkalosis
- Hypomagnesemia
- Iatrogenic Cushing syndrome
- Metabolic alkalosis
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Castro D, Sharma S. Hypokalemia. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/(accessed 18.9.2021)
- ↑ 2.0 2.1 Mayo clinic Hypokalemia Available:https://www.mayoclinic.org/symptoms/low-potassium/basics/causes/SYM-20050632?p=1 (accessed 3.6.2022)
- ↑ 3.0 3.1 Low Potassium(hypokalemia)[Internet]. 2012 August 10 [cited 2013 March 27] Available from:http://www.mayoclinic.com/health/low-potassium/MY00760
- ↑ 4.0 4.1 Healthline Hypokalemia Available: https://www.healthline.com/nutrition/potassium-deficiency-symptoms#bottom-line (accessed 3.6.2022)
- ↑ Mayo Clinic Hypokalemia Available: https://www.mayoclinic.org/symptoms/low-potassium/basics/when-to-see-doctor/sym-20050632 (accessed 19.9.2021)
- ↑ Hypokalemia [Internet]. 2012 [cited 2013 March 27] Available from:https://www.clinicalkey.com/topics/nephrology/hypokalemia.html#720089
- ↑ 7.0 7.1 Hypokalemia [Internet]. 2013 March 22 [cited 2013 March 27] Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000479.htm
- ↑ Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocrine connections. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)
- ↑ Goodman CC. Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641
see adding references tutorial.