Gout
Original Editors - Maggie Kraemer from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Gout is a metabolic disorder; however, because the clinical presentation closely resembles arthritis, gout is also classified as a form of crystal-induced arthritis. [1] [2]There are three main types of gout, all of which usually begin monoarticularly at the first metatarsophalangeal joint and are characterized by sudden pain, swelling, and redness.[1] [2] [3]
Prevalence[edit | edit source]
Effects over 2 million people in the US
The most common crystalopathy (in the US)
Rarely seen in children (< 10% of all cases) [1]
Predominantly seen in men (most common inflammatory disease in men over age 30)
Peak incidence in the 4th - 5th decades of life
Frequency increases in postmenopausal women (lack of estrogen) [1] [3]
Characteristics/Clinical Presentation[edit | edit source]
There are four stages of gout, although diagnosis does not require the presence or occurance of each stage. The four stages are:
- Asymptomatic hyperuricemia ( serum urate > 7mg/dl)
- Acute gouty arthritis
- Intercritical gout
- Chronic tophaceous gout[1]
- Asymtomatic hyperuricemia is the phase of gout prior to the first attack, when serum urate levels are elevated but no symptoms are present. [1]
- Acute gouty arthritis is the most common clincial presentation and is most often found (90%) at the first metatarsophalangeal joint. Symptoms generally begin with a sudden onset of localized, intense pain, often occuring at night. The pain may be great enough to awaken the patient. Redness, extreme tenderness, and swelling around the joint will occur within a few hours of the initial pain. Hypersensitivity, chills, tachycardia, malaise, and fever may also be present.[1] [2] [3] The skin may also become red or purplish, shiny, tense, and warm. [2]
Occasionally, acute gouty arthritis can also occur at the fingers, wrist, elbow, knee, ankle, and instep. Even more rarely, acute gouty arthritis may present at the cervical spine, sternoclavicular joint, shoulder, hip, and sacroilliac joint.[1] [2] [3] The initial attack may last a few days to 2 weeks, if left untreated. [2] [3] Attacks will recur; however time periods of months or years may elapse between them. As the attacks recur, they will become more intense and may spread to other joints in the body. [1] [2] [3] A patient may eventually exprience several attacks per year [1] [2]
Presentation of acute gout at the PIP joint
- The intercritical phase occurs after recovery from each episode. This phase is asymtomatic and may last for months to years at a time. It is important to note that although this is an aysmptomatic stage, serum urate levels are often still elevated and urate crystals may still be present. [1]
- As the gout attacks continue, tophi will develop in the joints, tendons, bursae, subchondral bone, cartilage, ligaments, subcutaneous tissue, and synovium.[1] Tophi are hard nodules of sodium urate deposits that may vary in number and location.[1] [3] [2] Although typically a painless structure, the formation of tophi can cause an acute inflammatory response within the tissue. [3] [2] As the tophi become enlarged they may cause deformities, and there is potential for them to protrude through the skin and exude a white chalky substance (urate crystals). [1] [3] [2] Some of the most common sites of enlarged tophi are the forearm, ear, knee and foot. [1]
Note: Prior to the use of urate-lowering drugs for the treatment of acute gouty arthritis, tophi developed in approximately 30 - 50% of patients. [3]
- Chronic tophaceous gout is characterized by increased pain, deformity (from tophi), decreased ROM, and subsequent functional loss.[1] [2] Due to the treatments used for gout today, chronic tophaceous gout is rare. [3]
Great pictures of the presentation of gout at various stages can also be found at:
www.skinsight.com/adult/gout.htm
[1][5]
Associated Co-morbidities
[edit | edit source]
None
Medications
[edit | edit source]
- NSAIDS, Corticosteroids[1] [2], or COX-2[2] inhibitors: for pain and inflammation management during an acute attack
- Allopurinol: to slow the rate of uric acid production and help prevent future attacks
- Cholchicine: occasionally used in the acute phase; however, use is less common due to frequency of side effects and narrow therapeutic range[2] [1]
- Supplementary analgesics
- Probenecid and sulfinpyrazone may be used to lower serum urate levels[2]
www.rxlist.com/script/main/hp.asp [6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
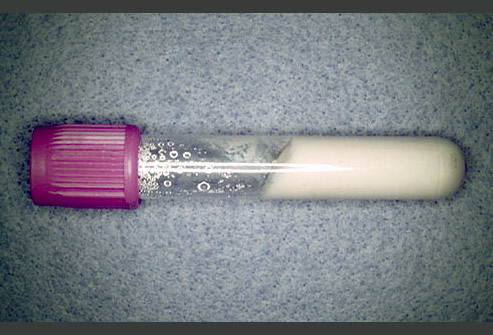
- Arthrocentesis and synovial fluid analysis: should be performed upon initial presentation. Positive results include: identification of needle shaped bifringent urate crystals that are engulfed by phagocytes or free floating[2] [1]; 2,000 - 100,000 WBCs/uL with over half of the WBCs as polymorphonuclear.[2]
- Gram stain and culture: to rule out infectious arthritis[2]
- Elevated serum urate levels may support diagnosis but are not sensitive or specific. Levels should be measured on several different occasions and it is possible for levels to be normal during and actute attack. Elevated levels are considered to be greater than 7mg/dL.[1] [2]
- 24 hour urate excretion: normal is 600-900 mg. This may help identify hyper production of uric acid or decreased excretion.[2]
- X-rays: to examine tophi. X-rays are not essential for diagnosis. [1] [2]
Causes[edit | edit source]
There are three types of hyperuricemia based on cause[1]:
- Primary hyperuricemia is an inherited form of the disorder.
- Idiopathic hyperuricemia does not have a known cause.
- Secondary hyperuricemia can result from a variety of causes including:
- renal dysfunction or disease (hemodialysis, polycystic kidney disease, renal insufficiency)[3] [2]
- leukemia, lymphomas, psoriasis[1] [2] [3]
- hematopoetic disorders (hemolytic anemia, myeloma, polycythemia vera, myeloproliferative disorder)[3]
- chemotherapy agents [1] [2] [3]
- obesity, fasting [1] [2] [3]
- medications (diuretics, salicylates, levodopa, cyclosporine, low dose asprin, vitamin B12)[1] [2] [3]
- heavy alcohol consumption[1] [2] [3]
- hypertension[1] [3]
- endocrine disorders: (hyperparathyroidism, hypoparathyroidism, hyperthyroidism, diabetes mellitus)[3]
- a diet rich in purines (shellfish, organ meats, beans, spinach, etc.)[1] [2] [3]
- medical stressors (surgery, trauma, infection, etc.)[2]
- fatigue or emotional stress [2]
- toxemia of pregnancy, hyperlipidemia, chondrocalcinosis [3]
Systemic Involvement[edit | edit source]
None
Medical Management (current best evidence)[edit | edit source]
There are three main goals of the medical management of gout:
1. Terminate acute attacks
2. Prevent recurrance
3. Correct and prevent further damage from hyperuricemia[1][2]
Termination of acute attacks - NSAIDs are the most common and generally effective treatment for acute attacks.[1][2] Cox-2 inhibitors are often the second choice for those who develop GI toxicity; however, they should be used with great caution with any patient with a history of CV complications or co-morbidities.[2] Intraarticular corticosteroid injection may also be effective for the management of an acute attack. Colchicine may also be used either po or by IV and may produce substantial pain relief if started immediately after onset of symptoms. Supplementary analgesics may also be recommended along with rest, elevation, and joint protection strategies. [1][2]
Prevention of recurrance - Daily low doses of NSAIDs or Cholcicine are commonly used to prevent recurrent attacks.[2]
Correction and prevention of hyperuricemia - Uricosuric drugs or allopurinol may be used alone or in conjunction. Hypouricemic therapy may also be used for patients with tophi and a higher recurrance rate. Dietary restriction of high-purine foods is a less effective treatment technique but is still recommended. Carbohydrate restrictions may also be helpful. Other treatment possibilties include hydration greater than 3 liters per day. Alkalinization of urine, extracorporeal shock wave lithotripsy, and surgical excision may also be beneficial.[2]
A list of high-purine foods can be found at: http://www.niams.nih.gov/Health_Info/Gout/default.asp. [7]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy management of gout falls under preferred practice pattern 4E: Impaired joint mobility, motor function, muscle performance, and range of motion associated with localized inflammation. [1]
The physical therapist should be aware that any patient with a history of gout, hyperuricemia, and/or a septic joint presentation should be refered for medical evaluation prior to treatment.[1]
During acute exacerbations the physical therapist should focus on reinforcement of management program and splinting, orthotics, or other assistive devices to protect the affected joint(s). [1]
A 2002 study in the Journal of Rheumatology found that the use of cryrotherapy to alleviate the pain associated with acute bouts of gout may be effective. [8]
During intercritical phases physical therapists may offer assistance with maintinance of ROM, strength, and function. The physical therapist can also assist the patient in the creation of a suitable exercise routine and keeping thier weight under control. [1][7]
Alternative/Holistic Management (current best evidence)[edit | edit source]
Few methods of alternative therapy have been thoroughly researched. However, some basic research does point to several possibilities for the success of alternative methods. More information can be found at: www.mayoclinic.com/health/gout/DS00090/DSECTION=alternative-medicine. [9]
Differential Diagnosis[edit | edit source]
Pseudogout - a form of arthritis that occurs 1/8th as often as gout. Symptoms are very similar to gout; however, the knee joint is primarily affected. Diagnosis is made by aspiration of synovial fluid.[3]

[edit | edit source]
Other differential diagnosis include RA, neoplasm, septic arthritis, infectious arthritis, acute rheumatic fever, juvenile RA, acute fracture, and palindromic rheumatism. [1][2]
Case Reports[edit | edit source]
One case report that presents interesting implications for the physical therapist involves an elderly patient with lumbar spondylodiscal pathology secondary to her polyarticular gout.
www.ncbi.nlm.nih.gov/pmc/articles/PMC1001146/ [11]
Interesting case report involving a middle aged man that developed symptoms of gout during a hospitalization.
www.ncbi.nlm.nih.gov/pmc/articles/PMC2572609/ [12]
Case report of a patient whose tophi were limiting the FDS tendon.
www.ncbi.nlm.nih.gov/pmc/articles/PMC2654956/ [13]
Case report involving presentation and differential diagnosis of acute monoarthritis.
www.ncbi.nlm.nih.gov/pmc/articles/PMC2612045/ [14]
A series of case reports that examine some of the negative effects of Colchicine as a form of pharmacological management.
www.ncbi.nlm.nih.gov/pmc/articles/PMC286251/ [15]
Resources
[edit | edit source]
http://www.webmd.com/a-to-z-guides/gout-topic-overview
www.mayoclinic.com/health/gout/DS00090
http://www.niams.nih.gov/Health_Info/Gout/default.asp
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zy4NRF93NhYRvPbm907MD3T3CE9MV0xZwipuu13CehWGKgg6M|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. Saint Louis, MO: Saunders; 2009.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 2.34 2.35 2.36 2.37 Beers MH, et. al. eds. The Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ 4.0 4.1 4.2 4.3 Brunilda, N. Gout Pictures Slideshow: Causes, Symptoms, and Treatments of Gout. 2008. http://arthritis.webmd.com/slideshow-gout. Accessed February 15, 2010.
- ↑ http://www.skinsight.com/adult/gout.htm
- ↑ http://www.rxlist.com/script/main/hp.asp
- ↑ 7.0 7.1 Gout. National Institute of Arthritis and Musculoskeletal and Skin Diseases. December 2006. http://www.niams.nih.gov/Health_Info/Gout/default.asp. Accessed March 2010.
- ↑ Schlesinger N, Detry MA, Holland BK, Baker DG, Beutler AM, Rull M, Hoffman BI, Schumacher HR Jr. Local ice therapy during bouts of acute gouty arthritis. J Rheumatol 2002; 29(2): 331-334
- ↑ Gout: Alternative Medicine. Mayo Clinic. November 2009. http://www.mayoclinic.com/health/gout/DS00090/DSECTION=alternative-medicine. Accessed March 2010.
- ↑ Wheeless, C R. Pseudogout and Chondrocalcinosis. Wheeless' Textbook of Orthopaedics. November 2008. www.wheelessonline.com/image9/cppd2.jpg. Accessed March 2010.
- ↑ Lagier R, Gee W M. Spondylodiscal erosions due to gout: anatomicoradiological study of a case. Annals of the Rheumatic Diseases. 1983 June; 42(3): 350-353.
- ↑ Dhoble A, Balakrishnan V, Smith R. Chronic tophaceous gout presenting as acute arthritis during an acute illness: a case report. Cases Journal. 2008; 1: 238.
- ↑ Sano K, et. al. Atypical Triggering at the Wrist due to Intratendinous Infiltration of Tophaceous Gout. Springer Hand. 2009 March; 4(1): 78-80.
- ↑ Ma L, Cranney A, and Holroyd-Leduc J. Acute monoarthritis: What is the cause of my patient's painful swollen joint. CMAJ. 2009 January; 180(1): 59-65.
- ↑ Morris I, Varughese G, and Mattingly P. Colchicine in acute gout. BMJ. 2003 November; 327(7426): 1275-1276.