Frail Elderly: The Physiotherapist's Role in Preventing Hospital Admission
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - <img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="1" _fck_mw_template="true">
Introduction
[edit | edit source]
This 10 hour online learning resource is tailored towards final year students and newly graduate physiotherapists, aiming to increase your knowledge and understanding of how you can use physiotherapy to prevent hospital admission in the community dwelling, frail elderly population. The module will also hopefully help you in applying this information in practice.
Aims[edit | edit source]
• To provide a learning resource for final year physiotherapy students or junior physiotherapists with an introduction to contemporary and emerging issues in the field of reducing hospital admissions in the frail elderly population and current management strategies.
• To provide you with an introduction and overview of the physiotherapists’ role in the prevention of hospital admissions in the frail elderly population by using a holistic, patient centred approach
Learning outcome[edit | edit source]
By the end of this Wiki module you will be able to…
• Synthesise current evidence and guidelines surrounding frailty and preventative pathways.
• Evaluate and reflect upon the physiotherapists’ role in the holistic assessment and treatment of frail persons to reduce the risk of hospital admission.
• Critically evaluate and reflect upon the skills and knowledge gained from this resource and recognise appropriate application in clinical practice.
Frailty[edit | edit source]
Definition[edit | edit source]
According to Fried et al (2001), frailty is defined as a “biological syndrome of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiological systems and causing vulnerability to adverse outcomes.” However it is also to be noted that despite the large proportion of the elderly population who are diagnosed as Frail, there is no standardised definition.
Fried et al. also provides a Phenotype for identifying those who are frail. It designates that to be considered frail the person must match three of five categories.
The categories are:
1. Shrinking, a drop in bodyweight of ≥10lbs/4.5kg in the past year or a drop in bodyweight of ≥5% in the past year. Can also be described as Sarcopenia or weight loss.
2. Weakness, measured using grip strength. A result within the lowest 20% according to gender and BMI indicates a weakness.
3. Reduced energy/endurance, self-reported. Can also be predictive of cardiovascular disease.
4. Slowness, the lowest 20% of the population according to gender and standing height based on a 15ft walking time.
5. Low Physical Activity, based on reported activity levels translated into a kilocalorie score. Again with a cut-off at the lowest 20% for each gender.
This can be a good way of describing the multiple physiological declines described in frail persons.
Assessment:
The Fried Frailty Index (FFI) as described above is commonly used to diagnose frail persons, those with 3 or more categories out of 5. It can also be used to designate persons as Intermediate frail or Pre-frail. Fried et al. suggests that those who score in 1 or 2 of the categories but not 3 are “Pre-frail”.
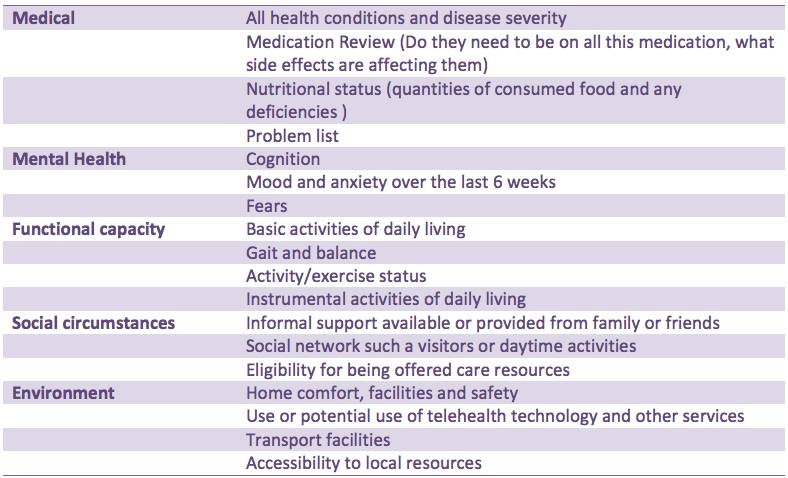
Another commonly used assessment tool is the Comprehensive Geriatric Assessment (CGA). This is a multidimensional assessment tool which is implemented by the multidisciplinary team. It can be used to determine a holistic treatment plan for frail persons looking at many aspects of their health such as; Medical condition, mental health, function, social circumstances and their environment. A physiotherapist will primarily be involved in the functional aspect of their assessment but they are not to neglect the other areas as this assessment tool puts real emphasis on the Holistic assessment/treatment approach.
• This assessment tool tends to be used upon acute hospital admission
• It is carried out by a number of AHP’s and medical staff with a coordinating consultant/specialist AHP/nurse
• It looks to link health and social care
• Holistic, patient centred approach
(Martin 2015)
Current Climate[edit | edit source]
Demographics[edit | edit source]
Costs[edit | edit source]
Length of stay and cost implications NHS
The latest published statistics which are being used in the literature relate to the years 2012 and 2013. Within this time frame 2,211,228 people over 60 were admitted to hospital in an emergency [1].
Graph 1 insert
Graph 2 insert
70% of day beds are occupied by people over 65; this is more than 51,000 beds at any one time. 85 year olds on average stay in hospital eight days longer than their younger counterparts (RCP 2012).
[edit | edit source]
[edit | edit source]
| A table to show the cost of average stays in hospital [1] | |||
|---|---|---|---|
| Type of stay | Short stay |
Extra bed day |
Visit to A and E |
| Cost |
£1489 |
£273 |
£114 |
Most emergency admissions to hospital happen through accident and emergency [1]. On average a person over 85 spends 11 days in hospital (RCP 2012). If they pass through accident and emergency the total spent is approximately £3241 per patient, per visit.
However, More than a 25% of over 85 year olds stay for 2 weeks and 10% stay longer than a month, when admitted as an emergency (Cornwall et al. 2012). This means that even more money is spent.
A table to show the cost of health care input needed from falls [2] | |
|---|---|
| Type of fall |
Cost to NHS in millions |
| falls on stairs |
£207 |
| falls on level ground |
£128 |
| Falls between levels |
£84 |
| Falls associated with baths |
£16 |
410,377 elderly persons were admitted to hospital due to a fall in 2013. Appropriate strategies could prevent this by up to 30% (Age UK, 2015).
Length of stay and cost implications worldwide
Across the world there are varying amounts of elderly people in hospitals, how much time they spend in hospital and how much it costs.
Graph 3 insert
In terms of falls 59,046 males and 113,632 females were admitted to hospital following a fall in Australia in 2013-2014 (AHIW 2015).
| A table to show statistics for hospital stays and costs in the United States of America (Weiss and Elixhauser 2014) | ||
|---|---|---|
| Over 65's |
Under 65's | |
| Hospital admissions |
34% |
66% |
| Average length of hospital stay |
5.2 days |
4.5 days |
| Cost of average hospital stay |
$10,200-$13,000 |
$5,000-$12,900 |
| Cost in 2012 |
$30,638.57 Million |
$346.86 Billion |
92% of this care was paid for by insurance companies (Weiss and Elixhauser 2014).
Comparing this to the UK we can see that although most people stay in hospital for fewer days than in the USA, in the UK elderly people remain in hospital for longer. This may have negative health impacts. The UK is 16th in the world when it comes to average length of stay in hospital (Health at a glance 2013).
Health and Social Care Integration[edit | edit source]
The Department of Health (2013b) report that although there are high numbers of emergency admissions through accident and emergency, which is very costly, at least one fifth could be dealt with in the community. Some ways of doing this are through: telemedicine, risk prediction tools, case management and alternatives to hospitals.
The integration of the health and social care systems in the UK was designed to improve service delivery and the effectiveness of care. There are nine outcomes which this incorporation is meant to achieve.
1. To allow people to look after and improve their own health
2. To allow as many people as possible to live independent lives
3. To ensure users have positive experiences of their health and social care
4. To maintain or improve users quality of life
5. To reduce health inequalities
6. To ensure unpaid carers are supported with their health and wellbeing needs
7. To ensure everyone; staff and users, are safe from harm at all times
8. To ensure staff employed in health and social care services feel involved in the work they do. They should also feel supported to implement change when needed.
9. To ensure that all resources are used effectively
The planning, resources and delivery of care will be now carried out together by the local authority or health board (The Scottish government 2015). This will mean that health and social care can run smoothly as one entity and users will experience a continuity of care.
One way this will have an effect is by reducing hospital admissions by allowing patient information to be shared more freely between hospitals and the community. This will allow for more effective multidisciplinary care in the community (Cornwall et al. 2012).
It has been said that better communication between health professionals, especially between those in hospitals and the social sector, may help reduce emergency admissions and help people return home sooner. However, there may be some barriers preventing this such as; differing funding levels, contrasting cultures, performance management and no sufficient way to share patient data. (DOH 2013b).
Policies and Guidelines[edit | edit source]
This section will present the most relevant guidelines and policies in relation to frailty and highlight the most useful points.
The policies and guidelines included in this wiki resource are:

|

| |
| Healthcare Improvement Scotland[3] | Think Frailty | Fit for Frailty |
For the purpose of this learning resource the chosen guidelines and policies were Scottish and UK related. If you intend to work or are currently working without the NHS you might be required to be familiar with policies in relation to your workplace.
Older People in Acute Care improvement programme (OPAC)[edit | edit source]
As the number of older people in the population is increasing, there is an increased need to ensure appropriate care for older people. Improving older people's acute care is a priority for the Scottish Government and in 2012 “The Older People’s Acute Care improvement programme (OPAC)” was commissioned by the Scottish Government.
The programme focuses on 2 key areas
- Frailty
- Delirium
In relation to frailty, the programme focused on identification and immediate management of frailty. This included screening for frailty and ensuring that older people who were identified as frail received a comprehensive geriatric assessment within 24 hours of admission. The document “Think Frailty” explored the strategies implemented in practice in more depth and will be discussed in Section 3.2 – Think Frailty
Healthcare Improvement Scotland (2015) reported the impact of the programme and found that:
- Frailty screening in 3 surgical wards at the Royal Infirmary of Edinburgh decreased the length of stay, number of falls and number of complaints
- A reduced length of stay in NHS Grampian
- 50% decrease in the number of falls per month in 2 wards in NHS Greater Glasgow and Clyde
The report emphasises the importance to continue building on this work and Healthcare Improvement Scotland is committed to continue working with NHS Boards and staff to support learning and improvement of skills in relation to the management of frailty and delirium (REF report)
Think Frailty[edit | edit source]
As mentioned above the Scottish Government provided funding for Healthcare Improvement Scotland's policy to improve health care for older people due to the rising numbers of unplanned admissions in older people and the strong evidence for the benefits of CGA for frail patients. The programme is aiming to ensure that 95% of frail patients have a CGA and are admitted or referred to a specialist unit within 24 hours of admission.
This case study report focuses on the work to identify frailty and ensure rapid CGA in four NHS boards in Scotland: NHS Ayrshire & Arran, NHS Grampian, NHS Lanarkshire and NHS Lothian.Common themes underpinning the success in the NHS boards mention in the report included:
Easy to use screening tool
The use of these should be at first point contact with older people; at the front door or at home
- Important to enable rapid identification and referral to CGA
- Valid screening tools reduces variability and increases the number of appropriate referrals to frailty services
Early intervention & Senior decision makers
- Senior decision makers were valued in particularly in NHS Ayrshire & Arran and NHS Grampian. As senior clinicians were more likely to use a wider range of care management options other than admission
- Early intervention focusing on discharge planning
Multidisciplinary team working
- Having a strong, integrated team was valued by all sites
- Good communication between the members of the MDT was important
- Common aim for all sites: Expanding the team. In particular physiotherapy and OT services so that a 7 day a week around the clock service is available
The sites involved in this project were able to show significant improvements in outcomes for frail elderly presenting at the hospital.
These outcomes included a reduction in the number of admissions and re-admissions to hospital.
To read more about each NHS board strategies to improve frailty identification and management access Think Frailty: Improving the identification and management of frailty
Fit for Frailty[edit | edit source]
Part 1: Recognition and management of frailty in individuals in community and outpatient settings
This part of the fit for frailty guidelines by the British Geriatric Society (BGS) (2014) intend to support health and social care professionals working with frail older people in the community. In order to recognise and identify frailty BGS (2014) recommends:
- During all encounters with health and social care professionals older people should be assessed for frailty
- There are 5 main syndromes of frailty; Falls, change in mobility, delirium, change in continence and susceptibility to side effects of medication. Encountering one of these should raise suspicion of frailty
- Gait speed, timed up and go test and the PRISMA questionnaire are recommended outcome measures to assess for frailty
For managing frailty in an individual BGS (2014) recommends:
- A Comprehensive Geriatric Assessment (CGA), which involves a holistic, multidimensional and multidisciplinary assessment of an individual
- The result of the CGA should be an individualised care and support plan (CSP).
- The CSP includes a named health or social care professional coordinating the person’s care. A plan for maintaining and optimising the person’s care as well as urgent, escalation and end of life care plans.
Gap in literature[edit | edit source]
Clinical guidelines provide evidence based recommendations in relation to the management of a specific condition or a syndrome. They are aiming to assists health and social care professionals in their decision making and help reduce undesirable variations in practice (Broughton and Rathbone 2001).
The guidelines on frailty discussed above are aimed to all health and social care professionals and it has been found that these rarely go in depth in their explanation of specific healthcare professional's role. As physiotherapists it can be difficult to identify what recommendations are most applicable to our practice in relation to the management of frailty.
The guidelines do not state the main role of physiotherapy in the management of frailty. However, exact guidance is challenging to provide as the assessment and treatment of frailty will vary depending on the individual, the setting and the situation.
The following sections of this wiki learning resource aims to critically synthesise evidence on the physiotherapy management of frailty in relation to preventing hospital admissions.
This aims to help “fill the gap” in the national clinical guidelines and make you as a final year physiotherapy student or recent graduate more aware of the physiotherapy role and practice in relation to frailty.
Physiotherapy assesment
[edit | edit source]
The comprehensive geriatric assessment[edit | edit source]
All the guidelines outlined above state a need for a comprehensive geriatric assessment (CGA) to be completed to diagnose patients who may be frail. From this assessment a holistic interdisciplinary treatment program can be devised to suit the problems and needs of the individual. The assessment is usually carried out by a geriatrician or another trained professional (Martin 2010; BGS 2014).
This assessment usually takes place when a patient is identified as possibly being frail; during acute illness, prior to surgery or when returning to a community environment. It is a multi-dimensional program, which looks at the patients; health (physical and mental), mobility and social status. This approach was introduced in 2001 by the Department of Health. There are five domains in which assessment takes place.
Below is a table adapted from Martin 2010 which identifies and outlines what should be included in each domain.
The methods used to achieve this are specific to the region of the UK in which you work. However, the measurement tools should be standardised and reliable. For example, the 6-minute walk test is commonly used to test gait and balance. Some measures identify problems while others examine their severity.
The assessment will allow health professionals to identify the associated effects of frailty to the patient, now and in the future. Once specific problems have been identified onward referral can be made to appropriate healthcare professionals. This can then allow for a more in depth assessment to be made around these problems. For example a patient may be referred to physiotherapy to help increase mobility (Martin 2010).
Follow up is part of the CGA and identifies effectiveness of treatment. These sessions usually occur when people are readmitted to hospital. A study examined whether a comprehensive assessment after an emergency admission is more effective when carried out by a team trained in a using a CGA. The paper showed that this approach reduced; costs, length of hospital stay, deterioration, mortality. Yet this approach is not yet taken in the community (Ellis 2011).
In hospitalised patients it has been shown to improve the accuracy of diagnosis and enhances management in both the long and short term (Ellis and Langhorne 2004; Sergi et al 2011). In the community completing a CGA can prevent reductions in mobility and problems which arise from poor mobility by implementing treatment programmes tailored to all the patients’ needs (Tikkanen et al. 2015). It can also reduce hospital stay, increase the likelihood of keeping patients out of hospital (Nikolaus et al. 1999; Barer 2011) and reduce mortality (Frese et al. 2012).
Quiz– How many of the key points can you recall? Who carries out a comprehensive geriatric assessment? Where can it take place? What are its key components? What effects can completing a CGA have?
Reflection- this activity should take 10 minutes to complete. Use the reading in this section and your prior knowledge to reflect upon any problems that you think may arise when carrying out this type of assessment.
Functional assessment of frail individuals[edit | edit source]
Not all of the papers reviewed below look at people diagnosed as being frail. As there is a lack of literature related to this population some literature has been extrapolated and applied to this population of patients.
What is it?
It is advised that frailty assessments should be carried out by an MDT. Physiotherapists have the knowledge and skill level to carry out the functional aspect. (The kings fund 2012; BGS 2014; Wyrko 2015).
Functional assessments are a way of determining health needs now and in the future. Assessments of patients with frailty should occur after every illness or injury to establish the effect the episode had on the patient’s functional ability (Fairhall et al. 2011). More specifically, functional assessments should be done on every patient over 75 (Mohile 2015). The functional assessment element of the comprehensive geriatric assessment compromises of; gait, balance, abilities to carry out activities of daily living (both fundamental and basic)and activity/exercise status (Martin 2010). All these areas should be assessed by the attending physiotherapist.
However, assessing frail elderly patients can be difficult as it takes a long time due to…
• A through assessment needs to be done (Top to toe including all elements of the ICF) (Wagstaff and Coakley 1988; Smyth 1990; Farrell 2004; BGS 2010).
• Are there any cognitive issues present? These include dementia and long-term or short-term memory problems. Cognitive function in the elderly has been shown to have a strong association with reduced functional performance (Morala 2006). It can also impact on how you carry out your assessment and communicate with the patient (Steven et al. 2002; Deary 2009).
• Auditory problems, affecting the patients’ ability to hear you (Fairhall et al. 2011)
• Visual problems, meaning the patient cannot see you or what you are trying to get them to do clearly. (Fairhall et al. 2011)
• Easily fatigued, causing patients to have reduced performance in activities which occur at the end of the assessment (Theou 2008). This may skew the results of any outcome measures used.
• Reduced / slow mobility (i.e. Sit-stand takes longer) (Theou 2008).
Subjective assessment
The subjective assessment will be very similar to that of any other patient. Yet, some specific questions related to age and frailty must be asked.
1. Has anything changed recently in terms of the patients’; visual, auditory, mobility, cognitive, medicative or activity levels (Baker 2015).
2. Questions should be asked regarding falls history and mobility status (Stokes 2004; Baker 2015).
3. It is useful to know how often the patient is eating what foods they consume. (Needle 2011).
4. Do they have help or support with activities of daily living from anyone? Do they give help or support to anyone? (Edwards 2002; Stokes 2004).
Activity: Think about why these questions are important to ask with this type of patient. This task should take 20 minutes.
Answers:
1. It’s important to know any changes which could affect the rest of your assessment and treatment plans. How could these changes have impacted on the patients’ life? Can we help to change any issues/problems?
2. We need to know about any previous falls. This will help determine their mobility status and how well they are coping. We can then tailor treatment where it is needed (Stubbs 2015; Sherrington and Tiedemann 2015).
3. Nutrition is important for these patients and it should be part of the physiotherapist assessment to check what and how often the patient is eating (Needle 2011). The physiotherapist can then reinforce good eating habits and if needed refer the patient to a dietician. It is also important to have an idea about how much the patient eats as this could contribute to increased fatigue. A reduced tolerance to activity is present in frail patients (Theou 2008) and so how much you include in your first assignment is crucial.
4. You can get an idea of what ADL’s they are able to do, how they are coping with these demands and how busy they are throughout the day (Edwards 2002; Stokes 2004).
Objective assessment
The objective assessment should begin by observing posture, skin condition and body shape (Wagstaff and Coakley 1988). This can give you clues as to their general health and the extent of their frailty.
Mobility
The dependency level of the patient should be established as high dependency can reduce quality of life (HAS 2005). This can be achieved by using outcome measures such as, the timed up and go which has been shown to have good reliability and validity as a tool for measuring the mobility status of patients who are frail (Podsiadlo 1991).
As gait speed is an important measure of frailty, it is important for physiotherapists to measure it. A speed of less than 0.8 m/sec indicates frailty (Fairhall et al. 2011; Woo 2015). Keeping track of the patient’s gait speed will enable the physiotherapist to see how recovery/ treatment are going.
Endurance can be tested by completing multiple sit to stands or by carrying out a six minute walk test. Monitoring the patients’ heart rate during this will give an indication of their bodies ability to respond to increased effort (HAS 2005). The six minute walk test has been shown to be valid and reliable within this population (Farrell 2004). Measuring endurance gives the physiotherapist an indication of how far the patient is likely to be able to walk, which can aid treatment planning and goal setting.
Analysing the persons gait is also important. However, the difference in gait in people who are frail has not been widely researched. As well as frail individuals having reduced gait speed, they also reduced stride length and cadence. Reductions in stride length are linked with the severity of frailty and come about due to sarcopenia and so lower limb weakness. It is advised that in order to truly assess gait the person should be asked to walk at a maximum speed (Schwenk 2014). Good indicators of falls risk are the berg balance scale and the Tinneti, as these look at functional balance (Farrell 2004; Lin 2004). Reduced balance is linked with increasing falls (Sherrington and Tiedemann 2015).
Balance should be assessed comprehensively as this will allow for individualised treatment. 75% of over 70’s have reduced, can increase falls (Sibley 2013). Physiotherapists prefer using their own observations to measure balance rather than outcome measures. Some use standardised outcome measures, but clinical decisions were based on observations. The Berg balance scale, single leg stance test and TUG were seen by physiotherapists as useful tools to measure functional ability. (Sibley 2013). Balance outcome measures were assessed in a systematic review for their psychometric properties. There are many which the physiotherapist can use; very few measure all aspects of balance. Testing a patients’ reactive balance was one area which was rarely examined. It is therefore important to know what aspects of balance and postural awareness are being tested by the OM so that treatment will be tailored to problems (Sibley 2014).
The patients’ ROM and strength should be assessed at every joint. Tibiotarsal range is important to measure as it can impact on posture and may therefore contribute to falls (HAS 2005). Grip strength can be tested by using a grip ball dynamometer and has been shown to be accurate and comfortable to use with people with frailty. It is important to measure grip strength as weakness can limit the patients’ ability to carry out activities of daily living (Chkeir et al. 2013). This type of dynamometer shows high validity and reliability (Chkeir et al. 2015)
Determining ROM is important with these patients as a link between reduced lower limb mobility and fall prevalence has been found. In this population dorsiflexion, plantar flexion, hip extension, internal rotation and abduction were found to be tight (Chiacchiero 2010). It is therefore important to establish if your patient has reduced ROM as tailored interventions may help reduce falls.
Activities of daily living (ADL’s) can help establish the range of motion and strength of frail patients. Two main types of ADL’s should be assessed, instrumental and basic (Martin 2010; Millán-Calenti 2010). Basic ADL’s are self-care tasks, whereas, instrumental ADL’s are activities which are needed for a person to live independently in the community (Ward 1998). IADL’s are important to measure as an inability to do these is a better indicator of dysfunction than ability to self-care (Ward 1998). The percentage of elderly people reported as being independent increased to 65.4% (from 46.5%) when looking at basic ADL’s when compared to IADLs. There are standardised outcome measures in which to assess IADLs, yet the specific activities needed to enable independence vary depending on the environment and social aspects of the patients’ life. It is therefore important to have a grasp of what the patients’ needs to be able to do to remain independent and them review these activities (Ward 1998). Functional dependence should be assessed as there are correlations between dependence and increased length of stay in hospital (Millán-Calenti 2010).
The Barthel index is a way to assess self-care. It was originally designed to use with stroke patients. Yet, research has shown that it is a reliable tool to use with geriatric patients (Richards et al. 1998). However, the Barthel index may be less reliable with individuals who have cognitive impairments (Sainsbury et al. 2005).
Optional reading: Ward, 1998 looked at different standardised IADL which can be used in practice.
Activity – should take 10 minutes.
What instrumental ADL do you think Mrs/Mr X need to be measured? (LINK TO CASESTUDY)
Activity levels
The therapist should have an idea as to what level of independence the patient has and how much physical activity they carry out on a daily basis. This can be achieved by functional tasks and by asking the patient and their families (Smyth 1990).
Outcome measures
Outcome measures may be useful to track the patient’s progress but also to assess the patient’s abilities (Jette et al. 2009; Kyte and Calvert 2015). There are many different outcome measures to choose in this population. Some were specifically designed for frailty while others were developed for other conditions but have been shown to have good psychometric properties with this population. The next section will review some commonly used outcome measures. However, this is not an exhortative list and will not necessarily be the best to use with each patient. It is up to the clinician to select the most appropriate measure for their practice.
| Outcome Measures (OM) |
Description of OM |
Psychometric properties |
|---|---|---|
| Frail elderly functional assessment (1995) |
Examines functional ability in the frail Nineteen point questionnaire |
-Valid -Reliable -Sensitive to change (Gloth et al. 1995, Gloth et al. 1999) |
| Ten Meter walk test |
-Excellent test-retest reliability and high concurrent validity when compared to the shorter 4 meter walking test (Peters et al. 2001). -High concurrent validity in the frail population with a 10 meter and 20 meter walk test (Leerar and Miller 2002). | |
| The Edmonton frail scale |
12 questions related to cognition, general health status, mobility, social status, medication use, nutrition, mood, continence and functional performance. It has a total score of 17 which depicts severe frailty. It is a very brief way of assessing for frailty and can be used to see whether a CGA should take place (Rolfson 2006). |
-Good inter-rater reliability -Takes less than 5 mins to complete -Good construct validity -Acceptable internal consistency |
| PRISMA 7 |
A questionnaire devised of seven yes/no questions that can be used when the patient is unable to carry out a stand up and go or a 10 meter walk test (NHS 2015). It was developed with a service in Canadian healthcare, to integrate frailty assessment and management and allow for increase patient-centred care. |
Using this approach can reduce hospitalisation and is an encouraged approach across systems (Hebert 2003). Its use is recommended by the BGS and can indicate frailty. (Fit for frailty reference). |
| The Barthel index |
It measures the patients’ ability to look after themselves by asking 10 questions and answers are graded on the amount of assistance needed to carry out the activity. |
The interrater reliability of this outcome is fair to good depending on which activity is being assessed (Richards et al. 1998). |
Both the Edmonton frail scale and the PRISMA 7 can be used by physiotherapists to determine whether a patient who displays symptoms of frailty is frail or not. If a positive result is found they could refer a patient back to their GP for further assessment.
Key points to take
• Assessment of known frail patients is important and should be carried out by physiotherapists at the first contact with every patient.
• Outcome measures should be regularly administered to review the physiotherapists’ effectiveness at improving frailty.
• There are specific elements which need to be measured with persons who are frail: list
• Doing these may help prevent hospital admissions.
Medical[edit | edit source]
As people age the number of medications taken by the elderly increases to help tackle the effects of aging, such as; heart problems, cholesterol, depression and discomfort.
Some of the causes of adverse drug reactions (ADRs) can occur with multiple medications or improper drug or dosage selection. Fall, distress, depression, anxiety, confusion and insomnia are a few of the symptoms of ADRs in elderly population[4].
Risk factors for ADR is such as:
- Age (≥85)
- Multiple prescribers
- Long duration of use
- Multiple chronic disease
- History of drug reactions
- Regular alcohol intake
Common medication and their side effects
| Medication | Conditions used to treat | Common side effects | Examples |
|---|---|---|---|
| Beta Blockers[5] | Angina, Heart failure, Atrial fibrillation and Heart attach | Angina, Heart failure, Atrial fibrillation and Heart attach Dizziness, tiredness, Blurred vision, slow heartbeat, diarrhoea and nausea | Atenolol, bisoprolol, acebutolol, metoprolol |
| Antidepressants[6] | Depression | Dizziness, insomnia, headaches, loss of appetite, anxious, feeling agitated and blurry vision | Tricyclic antidepressants, Selective serotonin reuptake inhibitors, Serotonin- noradrenaline reuptake inhibitors |
| Benzodiazepines[7] | Relief of severe anxiety | Drowsiness, difficulty concentrating, headaches and vertigo | Diazepam, lorazepam, Chlordiazepoxide |
| Non-Steroidal Anti- Inflammatory drugs[8] | Relieve pain, reduce inflammation and a high temperature | Short term use of NSAIDs is unlikely to have any side effects. However long term use causes indigestion and stomach ulcers | Ibuprofen, Aspirin, diclofenac, naproxen |
Side effects of medication such as drowsiness, blurred vision and insomnia can interfere with the treatment session and also delay any recovery, it is therefore important for physiotherapists to know if the patient is on any medication to modify treatments.
Physiotherapy treatment[edit | edit source]
Physical activity[edit | edit source]
Functional capacity declines with age and this is further accelerated by low levels of physical activity.
The recommendations for physical activity for older adults (65+) are:
- Older adults should aim to be active daily
- At least 150 minutes a week of moderate intensity activity
- Muscle strength training twice a week in addition to the 150 minutes of activity
- Balance training and co-ordination should be incorporated into activities to manage risk of falls
- Minimise sedentary time (Department of Health 2011 – Stay active)
Physical activity significantly decreases with age. In Scotland, 56% of men and 52% of women between the ages 65-74 met the recommendations for physical activity. This drops to only 31% of men and 21% of women over the age of 75 (The Scottish Government 2013).
Benefits of physical activity in frail older adults
Strength, endurance, balance and bone density is lost about 10% per decade, while muscle power reduces with around 30% per decade (BHF 2011). The loss of muscle mass and strength is called sarcopenia, which is highly prevalent among older adults and has been identified as a risk factor for frailty (Jansen et al. 2015).
Being physically active slows down these physiological changes associated with aging. Physical activity can also reduce the risk of falls, promote cognitive health and self-management of chronic diseases. As well as slowing down the deterioration in ability to perform ADLs and maintain quality of life in older adults (Chou et al. 2012; Weeks et al. 2008).
A meta-analysis by Chou et al. (2012) found that exercise is beneficial to improve balance, gait speed and abilities to carry out ADLs in the frail older adults.
Physiotherapists role in promoting physical activity in frail older adults
Due to their training and experience, physiotherapists are in a good position to promote health and well being of individuals and the community through education on physical activity and exercise prescription (Verhagen and Engbers 2009).
Recently there has been a shift in the general public health agenda towards the prevention of chronic conditions and enabling the aging population to stay active and manage conditions in the community. This have required a change in the role of physiotherapists towards addressing these issues through promotion of physical activity and other lifestyle changes (Spijker and MacInnes 2013).
Factors influencing participation in physical activity in older adults
Older peoples’ participation in physical activity can be effected by biological, demographic, physiological and social factors. These are important to be aware of when attempting to motivate older people to increase their activity levels.
- Men are more active then women
- A decline in physical activity with age is higher among: minority ethnic groups, those from lower socio-economic backgrounds, those with lower education and those living alone
- Older people might be less able due to pain, reduced mobility and the need of assistance to mobilise (Weeks et al. 2008)
- Physical activity can be influenced by trusted others such as health care professionals, care givers, family and friends
- Lack of transport often affects older peoples abilities to part take in activity
Psychological factors that can positively affect participation
- Beliefs and confidence in abilities to active
- General values, beliefs and attitudes
Psychological factors that can negatively affect participation
- Fear of falling and over exertion
- Safety concerns
=[edit | edit source]
===
Conclusion[edit | edit source]
Recent Related Research[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 DOH. Emergency admissions to hospital: merging the demand. http://www.nao.org.uk/wp-content/uploads/2013/10/10288-001-Emergency-admissions.pdf (accessed 20 dec 2015).
- ↑ AGE UK. Later in life United Kingdom. http://www.ageuk.org.uk/Documents/EN-GB/Factsheets (accessed 19 dec 2015).
- ↑ Healthcare Improvement Scotland. Older People in Acute Care improvement programme. http://www.healthcareimprovementscotland.org/our_work/person-centred_care/opac_improvement_programme.aspx (accessed 10 Nov 2015)
- ↑ Vervloet D, Durham S.Adverse reactions to drugs. BMJ 1998;316:1511-4. Full version: http://www.bmj.com/content/bmj/316/7143/1511.full.pdf (Accessed 12 Dec 2015).
- ↑ NHS. Beta- BlockersfckLRhttp://www.nhs.uk/Conditions/Beta-blockers/Pages/Introduction.aspx (Accessed 5 Jan 2016)
- ↑ NHS. Antidepressants.fckLRhttp://www.nhs.uk/Conditions/Antidepressant-drugs/Pages/Introduction.aspx (Accessed 2 Jan 2016)
- ↑ NHS. Generalised anxiety disorder in adults - Treatment. http://www.nhs.uk/Conditions/Anxiety/Pages/Treatment.aspx (Accessed 3 Jan 2016).
- ↑ NHS. Non-steroidal anti-inflammatory drugs (NSAIDS). http://www.nhs.uk/conditions/anti-inflammatories-non-steroidal/Pages/Introduction.aspx (Accessed 3 Jan 2016)