Frail Elderly: The Physiotherapist's Role in Preventing Hospital Admission: Difference between revisions
No edit summary |
No edit summary |
||
| Line 61: | Line 61: | ||
=== Fear of Falling === | === Fear of Falling === | ||
The prevalence of [[Fear of Falling|fear of falling]] in community-dwelling older adults ranges between 12% and 65%<ref>Legters K. Fear of falling. Phys Ther 2002; 82; 264-272</ref>. | The prevalence of [[Fear of Falling|fear of falling]] in community-dwelling older adults ranges between 12% and 65%<ref>Legters K. Fear of falling. Phys Ther 2002; 82; 264-272</ref>. The physiotherapist is in an ideal position to steer the individual towards the route of confrontation and recovery as opposed to activity avoidance and disability<ref name="CSP Falls 2016" />. There is high quality evidence from two systematic reviews highlighting the benefits of treatment to improve confidence and reduce fear of falling<ref>Zijlstra GAR, van Haastregt JCM, van Rossum E. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007; 55; 603-15</ref><ref>Rand D, Miller WC, Yiu J, et al. Interventions for addressing low balance confidence in older adults: a systematic review and meta-analysis. Age Ageing 2011; 40; 297-206</ref>. Recommended interventions include: exercise, including tai chi, and multi-component falls prevention programmes.<br> | ||
The physiotherapist is in an ideal position to steer the individual towards the route of confrontation and recovery as opposed to activity avoidance and disability<ref name="CSP Falls 2016" />. There is high quality evidence from two systematic reviews highlighting the benefits of treatment to improve confidence and reduce fear of falling<ref>Zijlstra GAR, van Haastregt JCM, van Rossum E. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007; 55; 603-15</ref><ref>Rand D, Miller WC, Yiu J, et al. Interventions for addressing low balance confidence in older adults: a systematic review and meta-analysis. Age Ageing 2011; 40; 297-206</ref>. Recommended interventions include: exercise, including tai chi, and multi-component falls prevention programmes.<br> | |||
=== Multi-Component Falls Prevention Programmes === | === Multi-Component Falls Prevention Programmes === | ||
| Line 78: | Line 70: | ||
== Self-Management == | == Self-Management == | ||
[[Image:Selfmanagement NHS.jpg|right]]For many people, older age is associated with long term conditions such as heart failure, dementia, chronic obstructive pulmonary disease (COPD) and diabetes. | [[Image:Selfmanagement NHS.jpg|right]]For many people, older age is associated with long term conditions such as heart failure, dementia, chronic obstructive pulmonary disease (COPD) and diabetes. An element of frailty is the decreased ability to withstand illness. Exacerbation of chronic conditions, an acute illness or a combination of both can trigger acute disability in frail older people and cause hospitalisation or institutionalisation<ref name="Think Frailty">Healthcare Improvement Scotland. Improving the identification and management of frailty. http://www.healthcareimprovementscotland.org/our_work/person-centred_care/opac_improvement_programme/frailty_report.aspx (accessed 19 Nov 2015)</ref>. | ||
Physiotherapist's have a role in promoting self-management of long term conditions and physical activity. Disease-related self-management abilities such as taking medication and exercise are often promoted by health care professionals. However, there may also be a need for interventions aimed at self-management of overall health and well-being to contribute to healthy ageing<ref name="Cramm2013">Cramm JM, Hartgerink JM, Steyerberg EW, Bakker TJ, Mackenbach JP, Nieboer AP. Understanding older patients’ self-management abilities: Functional loss, self-management, and well-being. Qual Life Res, 2013;22:85–92. http://www.ncbi.nlm.nih.gov/pubmed/22350532 (accessed 11 Jan 2016)</ref>. Older peoples’ abilities to self-manage the effects of the ageing process depends on physical, psychological and social aspects of their life<ref name="Cramm2014">Cramm JM, Twisk J, Nieboer AP. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMC Geriatrics 2014;14:28. http://bmcgeriatr.biomedcentral.com/articles/10.1186/1471-2318-14-28 (accessed 11 Jan 2016)</ref>. Physiotherapists working with frail older people could play a role in promoting healthy ageing. Evidence shows that interventions to promote healthy ageing can be used to the delay the onset of frailty and reduce its adverse outcomes among older people<ref name="Cramm2014" />. | Physiotherapist's have a role in promoting self-management of long term conditions and physical activity. Disease-related self-management abilities such as taking medication and exercise are often promoted by health care professionals. However, there may also be a need for interventions aimed at self-management of overall health and well-being to contribute to healthy ageing<ref name="Cramm2013">Cramm JM, Hartgerink JM, Steyerberg EW, Bakker TJ, Mackenbach JP, Nieboer AP. Understanding older patients’ self-management abilities: Functional loss, self-management, and well-being. Qual Life Res, 2013;22:85–92. http://www.ncbi.nlm.nih.gov/pubmed/22350532 (accessed 11 Jan 2016)</ref>. Older peoples’ abilities to self-manage the effects of the ageing process depends on physical, psychological and social aspects of their life<ref name="Cramm2014">Cramm JM, Twisk J, Nieboer AP. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMC Geriatrics 2014;14:28. http://bmcgeriatr.biomedcentral.com/articles/10.1186/1471-2318-14-28 (accessed 11 Jan 2016)</ref>. Physiotherapists working with frail older people could play a role in promoting healthy ageing. Evidence shows that interventions to promote healthy ageing can be used to the delay the onset of frailty and reduce its adverse outcomes among older people<ref name="Cramm2014" />. | ||
=== Physical Activity === | === Physical Activity === | ||
| Line 98: | Line 86: | ||
== Benefits of Physical Activity in Frail Older Adults == | == Benefits of Physical Activity in Frail Older Adults == | ||
Strength, endurance, balance and bone density is lost at a rate of 10% per decade, while muscle power reduces at around 30% per decade<ref name="BHF11">The British Heart Foundation National Centre for Physical Activity and Health. Interpreting the UK physical activity guidelines for older adults in transition. http://www.bhfactive.org.uk/older-adults-resources-and-publications-item/39/429/index.html (accessed 17 Oct 2015)</ref>. Sarcopenia is highly prevalent among older adults and has been identified as a risk factor for frailty<ref name="Jansen">Jansen FM, Prins RG, Etman A, van der Ploeg HP, de Vries SI, van Lenthe FJ, Pierik, FH. Physical Activity in Non-Frail and Frail Older Adults. PLoS One 2015;10:1-15. http://www.ncbi.nlm.nih.gov/pubmed/25910249 (accessed 27 Oct 2015)</ref>. [[Physical Activity in Older Adults|Being physically active]] slows down these physiological changes associated with ageing. Physical activity can also reduce the risk of falls, promote cognitive health and self-management of chronic diseases. It can also slow down the deterioration in ability to perform ADLs and maintain quality of life in older adults<ref name="Chou">Chou CH, Hwang CL, Wu YT. Effect of Exercise on Physical Function, Daily Living Activities and Quality of Life in the Frail Older Adults: A Meta Analysis. Arch Phys Med Rehabil 2012;93:237-44.http://www.sciencedirect.com/science/article/pii/S0003999311008173 (accessed 16 Oct 2015)</ref><ref name="Weeks">Weeks LE, Profit S, Campbell B, Graham H, Chircop A, Sheppard-LeMoine D. Participation in Physical Activity: Influences Reported by Seniors in the Community and in Long-Term Care Facilities. Journal of Gerontological Nursing 2008;34:36–43. http://www.healio.com/nursing/journals/jgn/2008-7-34-7/%7Bf65345f8-58ac-4381-a607-f663b5d57d53%7D/participation-in-physical-activity-influences-reported-by-seniors-in-the-community-and-in-long-term-care-facilities (accessed 7 Jan 2016)</ref>. A meta-analysis<ref name="Chou" /> | Strength, endurance, balance and bone density is lost at a rate of 10% per decade, while muscle power reduces at around 30% per decade<ref name="BHF11">The British Heart Foundation National Centre for Physical Activity and Health. Interpreting the UK physical activity guidelines for older adults in transition. http://www.bhfactive.org.uk/older-adults-resources-and-publications-item/39/429/index.html (accessed 17 Oct 2015)</ref>. Sarcopenia is highly prevalent among older adults and has been identified as a risk factor for frailty<ref name="Jansen">Jansen FM, Prins RG, Etman A, van der Ploeg HP, de Vries SI, van Lenthe FJ, Pierik, FH. Physical Activity in Non-Frail and Frail Older Adults. PLoS One 2015;10:1-15. http://www.ncbi.nlm.nih.gov/pubmed/25910249 (accessed 27 Oct 2015)</ref>. [[Physical Activity in Older Adults|Being physically active]] slows down these physiological changes associated with ageing. Physical activity can also reduce the risk of falls, promote cognitive health and self-management of chronic diseases. It can also slow down the deterioration in ability to perform ADLs and maintain quality of life in older adults<ref name="Chou">Chou CH, Hwang CL, Wu YT. Effect of Exercise on Physical Function, Daily Living Activities and Quality of Life in the Frail Older Adults: A Meta Analysis. Arch Phys Med Rehabil 2012;93:237-44.http://www.sciencedirect.com/science/article/pii/S0003999311008173 (accessed 16 Oct 2015)</ref><ref name="Weeks">Weeks LE, Profit S, Campbell B, Graham H, Chircop A, Sheppard-LeMoine D. Participation in Physical Activity: Influences Reported by Seniors in the Community and in Long-Term Care Facilities. Journal of Gerontological Nursing 2008;34:36–43. http://www.healio.com/nursing/journals/jgn/2008-7-34-7/%7Bf65345f8-58ac-4381-a607-f663b5d57d53%7D/participation-in-physical-activity-influences-reported-by-seniors-in-the-community-and-in-long-term-care-facilities (accessed 7 Jan 2016)</ref>. A meta-analysis<ref name="Chou" /> found that exercise is beneficial to improve balance, gait speed and abilities to carry out ADLs in the frail older adult population. See [[Physical Activity in Older Adults]] | ||
=== Factors Influencing Participation in Physical Activity in Older Adults === | === Factors Influencing Participation in Physical Activity in Older Adults === | ||
| Line 137: | Line 125: | ||
A Systematic Review of Randomized Controlled Trials<ref>Stares A, Bains M. [https://www.ncbi.nlm.nih.gov/pubmed/30762623 The Additive Effects of Creatine Supplementation and Exercise Training in an Aging Population: A Systematic Review of Randomized Controlled Trials.] Journal of geriatric physical therapy (2001). 2019 Feb.</ref> suggested that a low dose of creatine monohydrate along with resisted exercises may improve upper and lower extremities strength in healthy older adults. | A Systematic Review of Randomized Controlled Trials<ref>Stares A, Bains M. [https://www.ncbi.nlm.nih.gov/pubmed/30762623 The Additive Effects of Creatine Supplementation and Exercise Training in an Aging Population: A Systematic Review of Randomized Controlled Trials.] Journal of geriatric physical therapy (2001). 2019 Feb.</ref> suggested that a low dose of creatine monohydrate along with resisted exercises may improve upper and lower extremities strength in healthy older adults. | ||
== Motivation | == Motivation == | ||
Without goals, adherence to exercise is limited. The literature reinforces the fundamentals of effective goal setting: | |||
* [[Goal Setting in Rehabilitation|Patient-centred goals]] | * [[Goal Setting in Rehabilitation|Patient-centred goals]] | ||
* Small goals incrementally increasing to large goals e.g. short term and long term | * Small goals incrementally increasing to large goals e.g. short term and long term | ||
Revision as of 07:17, 13 November 2022
Frailty[edit | edit source]
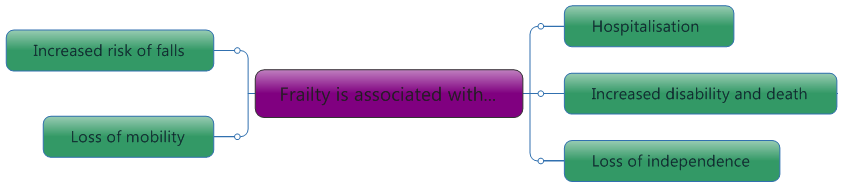
Frailty is a clinical state that is associated with an increased risk of falls, harm events, institutionalisation, care needs and disability/death.[1]The physiotherapist should be aware of the risk factors for frailty. If frailty is suspected, referral to other professionals may be required. Frailty and disability do not always co-exist, however they can be linked. In some cases, frailty may be a consequence of disability and in others, the causation of disability[2].
|
It is important to note that although frailty is age-related, it is not an inevitability[4]. In those aged 65 to 85, there is thought to be a 10% incidence of frailty. However, this figure increases to 25 to 50% in those aged 85 and over[5].
Ageing Population[edit | edit source]
People worldwide are living longer, with most people expected to live into their sixties and beyond. Every country in the world is experiencing growth in both the size and the proportion of older persons in the population. Older age may involve complex health states, commonly called geriatric syndromes, often the consequence of multiple underlying factors and include frailty, urinary incontinence, falls, delirium and pressure ulcers. So today with the growing older populations, healthcare services are required to transform to better meet the population’s needs[6][7].
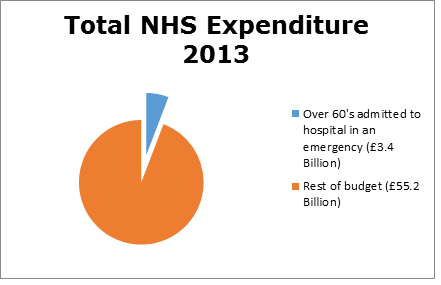
Costs[edit | edit source]
Health care costs already account for between 8% and 10% of GDP in developed countries. It is anticipated that even a modest increase in health care costs would generate significant pressure on the economy. For this reason every developed country is attempting to reform its health care system.[8]
The length of time frail people stay in hospital differs throughout the world. The UK is 16th shortest in the world when it comes to the average length of stay in hospital[9]. However, admittance to hospital and the cost implications of long term hospital stays are similar worldwide to the UK[10][11].
Relevance To Physiotherapy[edit | edit source]
With life expectancy continuing to rise globally there is an increasing public health focus on the maintenance of physical independence among all older adults. Identifying interventions that improve physical outcomes in pre-frail and frail older adults is imperative.[12]
Introduction to the Physiotherapist's Role[edit | edit source]
The nature of the physiotherapy profession is to help restore movement and function in someone affected by illness or injury[13]. Physiotherapist’s are expanding their service now to deliver interventions to several different settings; for example, within day hospitals, in the patient’s home and in community clinics.
- It has been suggested that physiotherapists could be stationed within hospital A&E departments to undertake frailty and falls risk screening and make rapid decisions on whether the patient can safely return to their pre-admission destination[14][15].
- The comprehensive geriatric assessment (an iterative collaborative multidimensional framework and process of assessment used to assess people living with frailty) may involve the physiotherapists. Their involvement in the delivery of a CGA is varied and ultimately depends on their speciality, which setting they work in, and the reasons for the patient being referred. If there has been a problem identified that can be able to acted upon it should be, if not a referral to an appropriate clinician is recommended[16].
- A randomized control trial[17] suggests home-based exercise and nutrition strategies have a positive outcome on the frailty score and physical perform
Physiotherapy Treatment[edit | edit source]
There are several clinical guidelines available for healthcare professionals to assist them in preventing hospital admissions providing quality care for patients. However, whilst they recommend physiotherapy intervention, these guidelines lack rigorous information and evidence surrounding treatment [18].
Injuries leading to hospitalisation are more common in people over 65 and they can be more critical and more often preventable. [19] Falls represent the most frequent and serious type of accident in people aged 65 and over in the UK [20]. As falls risk increases with age, it is important for the physiotherapist to identify those at risk early, recognise and modify risk factors and provide timely intervention to prevent falls and subsequent injury[21].
Falls Reduction In The Frail
Exercise (for strength and balance) has been shown to have the most effective outcomes in reduction of falls rates. As the majority of people who attend balance programmes relapse into old ways by six months, the physiotherapist should attempt to reinforce and encourage adherence to their home exercise program.
Examples of Physiotherapy Interventions below:
Resistance Training[edit | edit source]
A significant component of age-related weakness and frailty is sarcopenia. Sarcopenia increases the risk of frailty and falls and in turn, hospitalization in the older adult population[22]. Resistance training has been suggested as a potential treatment for sarcopenia and its prevention. Resistance training is designed to improve muscular fitness by exercising a muscle or a muscle group against resistance[23]. This could lead to improved function, increased quality of life and reduced likelihood for falls[24]. Resistance training programmes have consistently shown to improve muscle strength and mass in older adults[25][26], however, it is questionable whether this transfers to reducing the risk of falling.
Balance Re-education[edit | edit source]
Balance disorders are very common in frail older adults and are a key cause of falls in this population. They are associated with reduced level of function, as well as an increased risk of disease and death. Most balance disorders comprise of several contributing factors including long-term conditions and medication side effects[27].
See Balance Training, Otago Exercise Programme ,Inoculation Against Falls: Balance Intervention Strategies , Reactive Balance Training
Tai Chi[edit | edit source]
Tai chi is a newly emerging exercise incorporating breathing, relaxation and slow and gentle movements with strengthening and balance exercises.[28]. See Tai Chi and the Older Person
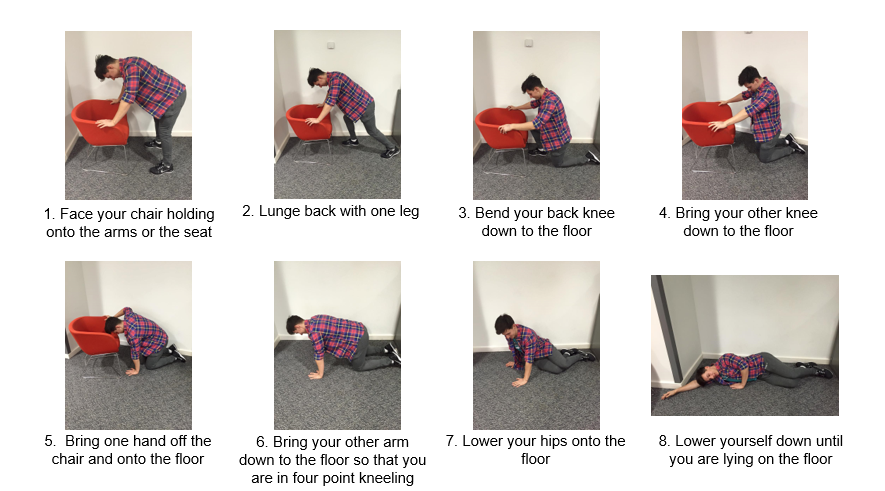
Backward Chaining[edit | edit source]
Backward-chaining (see link): Declining muscle function in older adults reduces their ability to rise from the floor following a fall and up to a half of all non-injured fallers are unable to get up[29]. When someone is unable to get up off the floor unassisted, the associated risks are far greater due to the complications that can occur from lying on the floor for an extended period of time – for example, dehydration, hypothermia, pneumonia, pressure sores, unavoidable incontinence and even death[30]. This inability to get up has a poor prognosis in terms of hospitalisation and mortality[30], thus, a long lie is one of the most serious consequences of a fall. It was found that the backward-chaining method significantly enhances ability in rising after an incidental fall (20-40%)[31]. This training falls within the physiotherapists domain.
Fear of Falling[edit | edit source]
The prevalence of fear of falling in community-dwelling older adults ranges between 12% and 65%[33]. The physiotherapist is in an ideal position to steer the individual towards the route of confrontation and recovery as opposed to activity avoidance and disability[21]. There is high quality evidence from two systematic reviews highlighting the benefits of treatment to improve confidence and reduce fear of falling[34][35]. Recommended interventions include: exercise, including tai chi, and multi-component falls prevention programmes.
Multi-Component Falls Prevention Programmes[edit | edit source]
As most falls are multifactorial in origin, they usually require several interventions[36]. Such interventions typically involve a combination of medication review and optimisation and education, environmental modification and exercise. This type of programme would be delivered by a multidisciplinary team in which the physiotherapist would be a key member. A Cochrane systematic review suggests that the physiotherapy treatment should combine all elements mentioned above; that is strengthening, balance, backward chaining, tai chi and confidence building with education, tailored to each individual. Clinic-based group exercise or individual exercise in the home setting is suitable. However, further research is needed into the effectiveness of medication management in preventing falls[37].
Additionally, in a systematic review, it was reported that for the greatest effect, exercise programmes should include a high level challenge to balance, alongside strength and walking training[38]. However, brisk walking training should not be prescribed to those at a high risk of falls. Furthermore, it was found that exercise should not only target those at high risk but also the general community and it should be performed for at least two hours per week on an ongoing basis.
Self-Management[edit | edit source]
For many people, older age is associated with long term conditions such as heart failure, dementia, chronic obstructive pulmonary disease (COPD) and diabetes. An element of frailty is the decreased ability to withstand illness. Exacerbation of chronic conditions, an acute illness or a combination of both can trigger acute disability in frail older people and cause hospitalisation or institutionalisation[39].
Physiotherapist's have a role in promoting self-management of long term conditions and physical activity. Disease-related self-management abilities such as taking medication and exercise are often promoted by health care professionals. However, there may also be a need for interventions aimed at self-management of overall health and well-being to contribute to healthy ageing[40]. Older peoples’ abilities to self-manage the effects of the ageing process depends on physical, psychological and social aspects of their life[41]. Physiotherapists working with frail older people could play a role in promoting healthy ageing. Evidence shows that interventions to promote healthy ageing can be used to the delay the onset of frailty and reduce its adverse outcomes among older people[41].
Physical Activity[edit | edit source]
Functional capacity declines with age and this is further accelerated by low levels of physical activity.
The recommendations for physical activity for older adults (65+)[42]:
- Older adults should aim to be active daily
- At least 150 minutes a week of moderate intensity activity
- Muscle strength training twice a week in addition to the 150 minutes of activity
- Balance training and co-ordination should be incorporated into activities to manage risk of falls
- Minimise sedentary time
Physical activity significantly decreases with age. The graph below shows the percentage of men and women meeting the physical activity recommendations in Scotland[43].
Benefits of Physical Activity in Frail Older Adults[edit | edit source]
Strength, endurance, balance and bone density is lost at a rate of 10% per decade, while muscle power reduces at around 30% per decade[44]. Sarcopenia is highly prevalent among older adults and has been identified as a risk factor for frailty[45]. Being physically active slows down these physiological changes associated with ageing. Physical activity can also reduce the risk of falls, promote cognitive health and self-management of chronic diseases. It can also slow down the deterioration in ability to perform ADLs and maintain quality of life in older adults[46][47]. A meta-analysis[46] found that exercise is beneficial to improve balance, gait speed and abilities to carry out ADLs in the frail older adult population. See Physical Activity in Older Adults
Factors Influencing Participation in Physical Activity in Older Adults[edit | edit source]
Older peoples’ participation in physical activity can be effected by biological, demographic, physiological and social factors. These factors are important to be aware of when attempting to motivate older people to increase their activity levels.[48]
- Men are more active than women
- A decline in physical activity with age is higher among: minority ethnic groups, those from lower socio-economic backgrounds, those with lower education and those living alone
- Older people might be less able due to pain, reduced mobility and the need of assistance to mobilise[47]
- Physical activity can be influenced by trusted others such as health care professionals, care givers, family and friends
- Lack of transport often affects older people's abilities to part take in activity
Physiotherapists Role in Promoting Physical Activity in Frail Older Adults[edit | edit source]
Due to their training and experience, physiotherapists are in a good position to promote health and well-being of individuals and the community through education on physical activity and exercise prescription[49]. Recently there has been a shift in the general public's health agenda towards the prevention of chronic conditions and enabling the ageing population to stay active and manage conditions in the community. This has required a change in the role of the physiotherapist towards addressing these issues through promotion of physical activity and other lifestyle changes[50]. When encouraging physical activity, physiotherapists should also aim to[51]:
- Identify fears and barriers to being physically active and provide solutions to overcome these
- Provide ongoing support and encouragement
Exercises for Frail Older Adults[edit | edit source]
These are the recommended activities and intensity for frail older adults to increase physical activity. These aim to improve general health and well being, as well as reduce the risk of falls and manage chronic lifestyle conditions:
- Sessions as short as 10 minutes can provide health benefits[44]
- Frail older adults should aim to accumulate numerous 10 minute sessions to achieve the recommended activity guides[52]
Suggested activities:
- Take the stairs[42]
- Walking[42]
- Do housework or gardening[42]
- Tai Chi[52]
- Dance[52]
- Swimming[42]
- Home-based or group exercise classes[44]
- Breaking up time spent sitting with short regular periods of standing or walking[52]
- Encourage to move for longer. E.g. Going from moving 5 minutes to 10 minutes may increase the intensity[52]
A Systematic Review of Randomized Controlled Trials[53] suggested that a low dose of creatine monohydrate along with resisted exercises may improve upper and lower extremities strength in healthy older adults.
Motivation [edit | edit source]
Without goals, adherence to exercise is limited. The literature reinforces the fundamentals of effective goal setting:
- Patient-centred goals
- Small goals incrementally increasing to large goals e.g. short term and long term
- Should adhere to SMART principles
Despite the need to motivate it is also important to listen to the patient and their needs. One of the ways we can encourage motivation is by arranging a group exercise class, as this not only promotes the physical benefits of exercise, but allows participation in a social gathering[54]. Furthermore, research suggests that people are more likely to exercise if they have a companion[55].
Conclusion[edit | edit source]
The average age of the population is increasing and it is suggested that the prevalence of frailty will multiply[56]. Subsequently, there has been a shift of care from reactive to preventative strategies and a focus on providing early interventions to reduce costly unplanned admissions to hospital[57]. Several guidelines are available, but none specifically detail the physiotherapist's role.
References[edit | edit source]
- ↑ Introduction to Frailty
- ↑ British Geriatrics Society. Fit For Frailty: Part 1: Recognition and management of frailty in individuals in community and outpatient settings. http://www.bgs.org.uk/index.php/fit-for-frailty (accessed 12 Oct 2015)
- ↑ Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A-Biol Sci Med Sci 2001; 56; 146-56
- ↑ Xue QL. The Frailty Syndrome: Definition and Natural History. Clin Geriatr Med 2011; 27: 1-15
- ↑ Clegg A, Young J, Iliffe S, Rikkert M, Rockwood K. Frailty in elderly people. Lancet (London, England). 2013 Feb 12 [cited 2016 Jan 27];9868(381). Available from: http://www.ncbi.nlm.nih.gov/pubmed/23395245.
- ↑ The King’s Fund. Making our health and care systems fit for an ageing population. http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/making-health-care-systems-fit-ageing-population-oliver-foot-humphries-mar14.pdf (accessed 28 Jan 2016)
- ↑ WHO Ageing and health Available:https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed 13.11.2022)
- ↑ Tabata K. Population aging, the costs of health care for the elderly and growth. Journal of Macroeconomics. 2005 Sep 1;27(3):472-93. Available:https://www.sciencedirect.com/science/article/abs/pii/S0164070405000303 (accessed 13.11.2022)
- ↑ Organisation for Economic Co-operation and Development. Health at a Glance, 2013. http://www.oecdilibrary.org/docserver/download/8113161e.pdf?expires=1444911042checksum=AAD68253A0B959E184ACCEE3FFE37481 (accessed 16 Oct 2015).
- ↑ Australia Institute of Health and Welfare. Australia’s hospitals 2013-14: at a glance http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129551482 (accessed 20 Dec 2015).
- ↑ Weiss, A. J., And Elixhauser, A., 2014. Overview of Hospital Stays in the United States, 2012. Online from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.jsp (accessed 4 Jan 2016).
- ↑ Kidd T, Mold F, Jones C, Ream E, Grosvenor W, Sund-Levander M, Tingström P, Carey N. What are the most effective interventions to improve physical performance in pre-frail and frail adults? A systematic review of randomised control trials. BMC geriatrics. 2019 Dec;19(1):1-1.Available:https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-019-1196-x (accessed 13.11.2022)
- ↑ NHS Choices. Physiotherapy. http://www.nhs.uk/conditions/Physiotherapy/Pages/Introduction.aspx (accessed 20 Jan 2016).
- ↑ Anaf S, Sheppard LA. Describing physiotherapy interventions in an emergency department setting: an observational pilot study. Accident and emergency nursing 2007; 15:1:34-9
- ↑ Arendts G, Fitzhardinge S, Pronk K, Donaldson M, Hutton M, Nagree Y. The impact of early emergency department allied health intervention on admission rates in older people: a non-randomized clinical study. BMC Geriatrics 2012; 12:8
- ↑ Comprehensive Geriatric Assessment
- ↑ Hsieh TJ, Su SC, Chen CW, Kang YW, Hu MH, Hsu LL, Wu SY, Chen L, Chang HY, Chuang SY, Pan WH. Individualized home-based exercise and nutrition interventions improve frailty in older adults: a randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2019 Dec 1;16(1):119.
- ↑ Albert M, McCaig LF, Ashman JJ. Emergency department visits by person aged 65 and over: United States, 2009-2010. Hyattsville, MD: National Center for Health Statistics, 2013
- ↑ Rothschild JM, Bates DW, Leape LL. Preventable medical injuries in older patients. Archives of Internal Medicine 2000; 160; 2717-28
- ↑ Age UK. Stop Falling: Start Saving Lives and Money. London: Age UK, 2010.
- ↑ 21.0 21.1 CSP. Physiotherapy works: Falls and frailty. http://www.csp.org.uk/professional-union/practice/evidence-base/physiotherapy-works/falls-and-frailty (accessed 8 Jan 2016)
- ↑ Sousa AS, Guerra RS, Fonseca I, et al. Sarcopenia and length of hospital stay. Eur J Clin Nutr 2015.
- ↑ Azeem K, Al Almeer A. Effect of weight training programme on body composition, muscular endurance, and muscular strength of males. Annals of Biological Research 2013; 4; 154-6
- ↑ Burton LA, Sumakadas D. Optimal management of sarcopenia. Clin Interv Aging 2010; 5; 217-28
- ↑ Liu CJ, Latham NK. Progressive resistance training for improving physical function in older adults (Cochrane review). Cochrane Database Syst Rev 2009; (3); CD002759
- ↑ Seynnes O, Fiatarone Singh MA, Hue O. Physiological and functional responses to low-moderate versus high-intensity progressive resistance training in frail elders. J Gerontol Ser A-Biol Sci Med Sci 2004; 59A; 503-9
- ↑ Rubenstein, LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing 2006; 35.
- ↑ NHS Choices. A guide to tai chi. http://www.nhs.uk/Livewell/fitness/Pages/taichi.aspx (accessed 8 Jan 2016)
- ↑ Skelton D, Dinan SM, Campbell M, et al. Tailored group exercise (Falls Management Exercise – FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005; 34; 636-639
- ↑ 30.0 30.1 Tinetti ME, Liu WL, Claus EB, et al. Predictors and prognosis of inability to get up after falls among elderly persons. JAMA 1993; 269; 65-70
- ↑ Zak M, Skalska A, Szczerbinska K. Instructional programmes on how to rise unassisted effectively after sustaining an incidental fall, designed specifically for the elderly: a randomized, controlled trial. Ortop Traumatol Rehabil 2008; 10; 496-507
- ↑ NHS Sutton and Merton Community Services. Getting on and off the floor safely. London: Staying Steady Falls Prevention Service, 2012
- ↑ Legters K. Fear of falling. Phys Ther 2002; 82; 264-272
- ↑ Zijlstra GAR, van Haastregt JCM, van Rossum E. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007; 55; 603-15
- ↑ Rand D, Miller WC, Yiu J, et al. Interventions for addressing low balance confidence in older adults: a systematic review and meta-analysis. Age Ageing 2011; 40; 297-206
- ↑ Hausdorff JM, Nelson ME, Kaliton D, et al. Etiology and modification of gait instability in older adults: a randomised controlled trial of exercise. J Appl Phys 2001; 90; 2117-29
- ↑ Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community (Cochrane review). Cochrane Database Syst Rev 2012; (2): CD007146
- ↑ Sherrington C, Tiedemann A, Fairhall N, et al. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. New South Wales Public Health Bulletin 2011; 22; 78-83
- ↑ Healthcare Improvement Scotland. Improving the identification and management of frailty. http://www.healthcareimprovementscotland.org/our_work/person-centred_care/opac_improvement_programme/frailty_report.aspx (accessed 19 Nov 2015)
- ↑ Cramm JM, Hartgerink JM, Steyerberg EW, Bakker TJ, Mackenbach JP, Nieboer AP. Understanding older patients’ self-management abilities: Functional loss, self-management, and well-being. Qual Life Res, 2013;22:85–92. http://www.ncbi.nlm.nih.gov/pubmed/22350532 (accessed 11 Jan 2016)
- ↑ 41.0 41.1 Cramm JM, Twisk J, Nieboer AP. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMC Geriatrics 2014;14:28. http://bmcgeriatr.biomedcentral.com/articles/10.1186/1471-2318-14-28 (accessed 11 Jan 2016)
- ↑ 42.0 42.1 42.2 42.3 42.4 Department of Health. Start active, stay active: report on physical activity in the UK. https://www.gov.uk/government/publications/start-active-stay-active-a-report-on-physical-activity-from-the-four-home-countries-chief-medical-officers (accessed 28 Oct 2015)
- ↑ The Scottish Government. The Scottish Health Survey 2012. Volume 1 – Main report. http://www.gov.scot/Publications/2013/09/3684 (accessed 28 Oct 2015)
- ↑ 44.0 44.1 44.2 The British Heart Foundation National Centre for Physical Activity and Health. Interpreting the UK physical activity guidelines for older adults in transition. http://www.bhfactive.org.uk/older-adults-resources-and-publications-item/39/429/index.html (accessed 17 Oct 2015)
- ↑ Jansen FM, Prins RG, Etman A, van der Ploeg HP, de Vries SI, van Lenthe FJ, Pierik, FH. Physical Activity in Non-Frail and Frail Older Adults. PLoS One 2015;10:1-15. http://www.ncbi.nlm.nih.gov/pubmed/25910249 (accessed 27 Oct 2015)
- ↑ 46.0 46.1 Chou CH, Hwang CL, Wu YT. Effect of Exercise on Physical Function, Daily Living Activities and Quality of Life in the Frail Older Adults: A Meta Analysis. Arch Phys Med Rehabil 2012;93:237-44.http://www.sciencedirect.com/science/article/pii/S0003999311008173 (accessed 16 Oct 2015)
- ↑ 47.0 47.1 Weeks LE, Profit S, Campbell B, Graham H, Chircop A, Sheppard-LeMoine D. Participation in Physical Activity: Influences Reported by Seniors in the Community and in Long-Term Care Facilities. Journal of Gerontological Nursing 2008;34:36–43. http://www.healio.com/nursing/journals/jgn/2008-7-34-7/%7Bf65345f8-58ac-4381-a607-f663b5d57d53%7D/participation-in-physical-activity-influences-reported-by-seniors-in-the-community-and-in-long-term-care-facilities (accessed 7 Jan 2016)
- ↑ The British Heart Foundation National Centre for Physical Activity and Health. Factors influencing physical activity in older adults. http://www.bhfactive.org.uk/resources-and-publications-item/18/404/index.html (accessed 11 Jan 2016)
- ↑ Verhagen E, Engbers L. The physical therapist’s role in physical activity promotion. Br J Sports Med 2009;43:99–101. http://bjsm.bmj.com/content/43/2/99.abstract (accessed 28 Oct 2015)
- ↑ Spijker J, MacInnes J. Population ageing: the timebomb that isn’t? BMJ 2013;347:1-5. http://www.bmj.com/content/347/bmj.f6598.full.pdf+html (accessed 11 Jan 2016)
- ↑ The British Heart Foundation National Centre for Physical Activity and Health. Physical activity interventions for older adults. http://www.bhfactive.org.uk/older-adults-resources-and-publications-item/18/405/index.html (accessed 13 Jan 2016)
- ↑ 52.0 52.1 52.2 52.3 52.4 The British Heart Foundation National Centre for Physical Activity and Health. Interpreting the UK physical activity guidelines for frailer older adults. http://www.bhfactive.org.uk/resources-and-publications-item/39/430/index.html (accessed 17 Oct 2015)
- ↑ Stares A, Bains M. The Additive Effects of Creatine Supplementation and Exercise Training in an Aging Population: A Systematic Review of Randomized Controlled Trials. Journal of geriatric physical therapy (2001). 2019 Feb.
- ↑ Thomas B, Storey E. [place unknown: publisher unknown]. Motivating the elderly client in long-term care; 2015 Dec 28 [cited 2016 Jan 8]. Available from: http://physical-therapy.advanceweb.com/Article/Motivating-the-Elderly-Client-in-Long-Term-Care.aspx.
- ↑ Rosenfeld M. Motivational Strategies in Geriatric Rehabilitation. Bethseda, MD: American Occupational Therapy Association; 1997.
- ↑ Karunananthan S, Wolfson C, Bergman H, Beland F, Hogan DB. A multidisciplinary systematic literature review on frailty: overview of the methodology used by the Canadian Initiative on Frailty and Aging. BMC Med Res Methodol 2009;9:68.
- ↑ Edwards N. Community services - how they can transform care. London: The King's Fund, 2014.