Foot Orthotics Assessment: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 8: | Line 8: | ||
== What do foot orthoses do? == | == What do foot orthoses do? == | ||
A foot orthosis is an externally applied apparatus that can be inserted in a shoe to help support or improve the function of the foot and/or ankle. The goal is either to reduce pressure across a specific region of the foot or ankle by offloading this area, or to accommodate deformities resulting from a disease process. The target effect of the orthotic can be achieved by applying controlled force on the foot to achieve either pressure transfer and redistribution, or motion restriction. The ultimate goal is maintaining neutral or near neutral subtalar joint alignment through the gait cycle.<ref>Elattar O, Smith T, Ferguson A, Farber D, Wapner K. [https://journals.sagepub.com/doi/full/10.1177/2473011418780700 Uses of braces and orthotics for conservative management of foot and ankle disorders.] Foot & Ankle Orthopaedics. 2018 Aug 3;3(3):2473011418780700.</ref> | |||
# Support | # Support | ||
# Correct, if mobile | # Correct, if mobile | ||
| Line 26: | Line 26: | ||
== Plantar Fascia == | == Plantar Fascia == | ||
* The plantar fascia is not a nerve, tendon or muscle, but a strong fibrous tissue. This stiff and relatively impermeable covering helps to protect the muscles of the sole of the foot.<ref>Welte L, Kelly LA, Kessler SE, Lieberman DE, D'Andrea SE, Lichtwark GA, Rainbow MJ. [https://royalsocietypublishing.org/doi/abs/10.1098/rspb.2020.2095 The extensibility of the plantar fascia influences the windlass mechanism during human running.] Proceedings of the Royal Society B. 2021 Jan 27;288(1943):20202095.</ref> | |||
* This tissue originates deep within the plantar surface of the calcaneus fanning out across the met heads, it divides and attaches to the base of the phalanges of each toe. | |||
* During walking, as the toes dorsiflex at push off the plantar fascia wraps around the metatarsal heads and tightens. This pulls the calcaneus towards the metatarsal heads and in turn maintains the shape of the longitudinal arch and supports the foot to enable propulsion. This is a phenomenon known as the windlass mechanism.<ref>Sichting F, Holowka NB, Ebrecht F, Lieberman DE. [https://onlinelibrary.wiley.com/doi/full/10.1111/joa.13173 Evolutionary anatomy of the plantar aponeurosis in primates, including humans.] Journal of anatomy. 2020 Jul;237(1):85-104.</ref> | |||
== Windlass Mechanism == | == Windlass Mechanism == | ||
Hicks first described the windlass mechanism in 1954 as a one-to-one coupling between metatarsal joint dorsiflexion and medial longitudinal arch rise. Based on an engineering concept of lifting weights via a pulley system. He proposed that dorsiflexion of the toes tightens the plantar aponeurosis and pulls the metatarsal heads towards the calcaneus thereby increasing the structural height of the longitudinal arch. This action occurs naturally at push off in gait cycle as toes dorsiflex and the foot becomes stiffer to aid propulsion. During loading and mid stance the arch will stretch. The human foot is flexible by its nature of many articulations and requires to be flexible at times and rigid at other times to promote normal gait. Important to remember that the plantar fascia will stretch and recoil at different stages of the gait cycle. | Hicks first described the windlass mechanism in 1954 as a one-to-one coupling between metatarsal joint dorsiflexion and medial longitudinal arch rise. Based on an engineering concept of lifting weights via a pulley system. He proposed that dorsiflexion of the toes tightens the plantar aponeurosis and pulls the metatarsal heads towards the calcaneus thereby increasing the structural height of the longitudinal arch. This action occurs naturally at push off in gait cycle as toes dorsiflex and the foot becomes stiffer to aid propulsion. During loading and mid stance the arch will stretch. The human foot is flexible by its nature of many articulations and requires to be flexible at times and rigid at other times to promote normal gait. Important to remember that the plantar fascia will stretch and recoil at different stages of the gait cycle.<ref>Sichting F, Ebrecht F. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0249965 The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism]. PloS one. 2021 Apr 8;16(4):e0249965.</ref> | ||
== Important Joints with regards to Foot Orthosis for ROM in the Foot/Ankle == | == Important Joints with regards to Foot Orthosis for ROM in the Foot/Ankle == | ||
| Line 78: | Line 77: | ||
* Gait pattern and biomechanical analysis on entrance | * Gait pattern and biomechanical analysis on entrance | ||
* Type of shoes | * Type of shoes<ref>Gegen ME, Plummer T, Darr N. [https://nsuworks.nova.edu/ijahsp/vol18/iss4/8/ An Exploratory Study of The Perceptions of Footwear for Individuals who use Lower Limb Orthotics.] Internet Journal of Allied Health Sciences and Practice. 2020;18(4):8.</ref> | ||
* Assistive devices | * Assistive devices | ||
* History of underlying conditions, foot problems and the primary problem affecting the individual on consultation. | * History of underlying conditions, foot problems and the primary problem affecting the individual on consultation. | ||
| Line 90: | Line 89: | ||
# Non weightbearing | # Non weightbearing | ||
'''<u>Active and Passive Movements in the Foot and Ankle</u>''' | '''<u>Active and Passive Movements in the Foot and Ankle</u>'''<ref name=":0">Alazzawi S, Sukeik M, King D, Vemulapalli K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241541/ Foot and ankle history and clinical examination: A guide to everyday practice.] World journal of orthopedics. 2017 Jan 18;8(1):21.</ref> | ||
* Dorsiflexion/ Plantarflexion - Quick test for the Ankle Joint | * Dorsiflexion/ Plantarflexion - Quick test for the Ankle Joint | ||
| Line 98: | Line 97: | ||
* Toe flexion/ extension – Quick test for the Metatarsal Phalangeal joints | * Toe flexion/ extension – Quick test for the Metatarsal Phalangeal joints | ||
'''<u>Non weight bearing assessment</u>''' | '''<u>Non weight bearing assessment</u>'''<ref name=":0" /> | ||
* [[Windlass Test]] - can be effective in examining dysfunction of the plantar fascia although specificity has not been proved. | * [[Windlass Test]] - can be effective in examining dysfunction of the plantar fascia although specificity has not been proved. | ||
| Line 110: | Line 109: | ||
* '''<u>Hallux Limitus/rigidus</u>''' | * '''<u>Hallux Limitus/rigidus</u>''' | ||
* Both affect the windlass mechanism and gait pattern and normal functioning of the foot. | * Both affect the windlass mechanism and gait pattern and normal functioning of the foot. | ||
** Hallux Rigidus | ** Hallux Rigidus<ref>Colò G, Fusini F, Samaila EM, Rava A, Felli L, Alessio-Mazzola M, Magnan B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7944704/ The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature.] Acta Bio Medica: Atenei Parmensis. 2020;91(Suppl 14).</ref> | ||
*** Very limited dorsiflexion mobility or no mvt. there is crepitation with joint mobilization and pain associated with any movement of the first MTP joint. | *** Very limited dorsiflexion mobility or no mvt. there is crepitation with joint mobilization and pain associated with any movement of the first MTP joint. | ||
** Hallux | ** Hallux Limitus<ref>Graydon M. [https://pedorthic.ca/wp-content/uploads/2021/10/Clinical-Practice-Guidelines-Second-Edition-PDF.pdf#page=153 Hallux Limitus/Rigidus. Clinical Practice Guidelines.] 2018:140.</ref> (FnHL) | ||
*** Reduced dorsiflexion movement, resulting in reduced range of dorsiflexion of the first MTP joint. | *** Reduced dorsiflexion movement, resulting in reduced range of dorsiflexion of the first MTP joint. | ||
*** In gait, loss of metatarsophalangeal joint extension during the second half of the single-support phase, when the weightbearing foot is in maximal dorsiflexion. | *** In gait, loss of metatarsophalangeal joint extension during the second half of the single-support phase, when the weightbearing foot is in maximal dorsiflexion. | ||
==== 3. Muscles | ==== 3. Muscles of the Foot and Ankle ==== | ||
There are four muscle compartments in the lower leg. These muscles are all tested using the standardized Oxford Scale. | There are four muscle compartments in the lower leg. These muscles are all tested using the standardized Oxford Scale. | ||
[[File:Posterior superficial muscle compartment.jpg|left|frameless|600x600px]] | [[File:Posterior superficial muscle compartment.jpg|left|frameless|600x600px]] | ||
| Line 160: | Line 159: | ||
'''Muscles''': [[Tibialis Anterior]], Extensor Hallicus Longus and Extensor Digitorum Longus | '''Muscles''': [[Tibialis Anterior]], Extensor Hallicus Longus and Extensor Digitorum Longus | ||
| Line 212: | Line 210: | ||
* Kirby 2001 | * Kirby 2001 | ||
'''<u>Dynamic Normal Walking</u>''' | '''<u>Dynamic Normal Walking</u>'''<ref name=":0" /> | ||
* o IC heel strike, | * o IC heel strike, | ||
| Line 236: | Line 234: | ||
# Scoliosis | # Scoliosis | ||
# Apparent leg length | # Apparent leg length | ||
# Actual leg length | # Actual leg length<ref>Menez C, L'Hermette M, Coquart J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7750876/ Orthotic insoles improve gait symmetry and reduce immediate pain in subjects with mild leg length discrepancy.] Frontiers in sports and active living. 2020;2.</ref> | ||
[[File:Leg Length.jpg|center|frameless|800x800px]] | [[File:Leg Length.jpg|center|frameless|800x800px]] | ||
<references /> | <references /> | ||
Revision as of 20:39, 30 December 2021
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Lucinda hampton, Ewa Jaraczewska and Tarina van der Stockt
Orthotics is a branch of medicine dealing with the making and fitting of orthotic devices. There are many interchangeable terms for this, a few being foot orthotic/orthosis/insole/shoe insert.
Three Main Types of Foot Orthoses[edit | edit source]
- Off the shelf (OTS) Insoles
- Functional Foot Orthoses (FFO)
- Custom Molded Total Contact Insoles (TCI)
What do foot orthoses do?[edit | edit source]
A foot orthosis is an externally applied apparatus that can be inserted in a shoe to help support or improve the function of the foot and/or ankle. The goal is either to reduce pressure across a specific region of the foot or ankle by offloading this area, or to accommodate deformities resulting from a disease process. The target effect of the orthotic can be achieved by applying controlled force on the foot to achieve either pressure transfer and redistribution, or motion restriction. The ultimate goal is maintaining neutral or near neutral subtalar joint alignment through the gait cycle.[1]
- Support
- Correct, if mobile
- Accommodate if not
- Shock absorption
- Re-distribute pressure
Basic Foot Anatomy[edit | edit source]
- 28 Bones
- 33 Joints
- Ligaments
- Tendons
- Muscles
- Joints
- Plantar Fascia
Plantar Fascia[edit | edit source]
- The plantar fascia is not a nerve, tendon or muscle, but a strong fibrous tissue. This stiff and relatively impermeable covering helps to protect the muscles of the sole of the foot.[2]
- This tissue originates deep within the plantar surface of the calcaneus fanning out across the met heads, it divides and attaches to the base of the phalanges of each toe.
- During walking, as the toes dorsiflex at push off the plantar fascia wraps around the metatarsal heads and tightens. This pulls the calcaneus towards the metatarsal heads and in turn maintains the shape of the longitudinal arch and supports the foot to enable propulsion. This is a phenomenon known as the windlass mechanism.[3]
Windlass Mechanism[edit | edit source]
Hicks first described the windlass mechanism in 1954 as a one-to-one coupling between metatarsal joint dorsiflexion and medial longitudinal arch rise. Based on an engineering concept of lifting weights via a pulley system. He proposed that dorsiflexion of the toes tightens the plantar aponeurosis and pulls the metatarsal heads towards the calcaneus thereby increasing the structural height of the longitudinal arch. This action occurs naturally at push off in gait cycle as toes dorsiflex and the foot becomes stiffer to aid propulsion. During loading and mid stance the arch will stretch. The human foot is flexible by its nature of many articulations and requires to be flexible at times and rigid at other times to promote normal gait. Important to remember that the plantar fascia will stretch and recoil at different stages of the gait cycle.[4]
Important Joints with regards to Foot Orthosis for ROM in the Foot/Ankle[edit | edit source]
- Hindfoot
- Talocrural Joint
- Sub Talar joint
- Mid Foot
- Tarsometatarsal Joint
- Calcaneocuboid Joint
- Talonavicular Joint
- Fore Foot
- 1st Metatarsal Phalangeal Joint
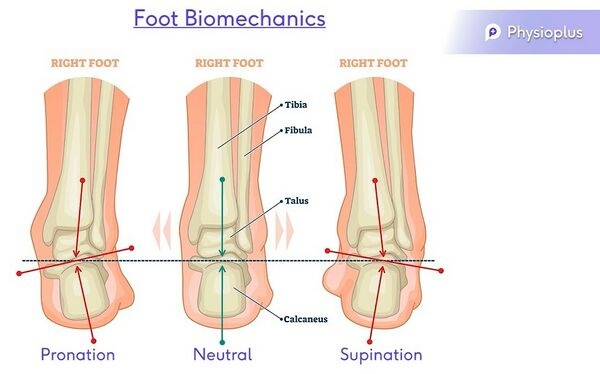
Terminology used in Orthotics[edit | edit source]
Valgus = Everted
Neutral
Varus = Inverted
Pronation – Eversion, abduction, dorsiflexion & medially rotated subtalar joint
Supination- Inversion, adduction, plantarflexion & laterally rotated subtalar joint
Purpose of human foot[edit | edit source]
“[The human foot] enables propulsion through space, adaptation to uneven terrain, absorption of shock, and support of body weight.”[5]
The human foot is a complex mechanism with a number of theories of biomechanics. The structure, function and position leave the foot exposed to risk of injury. When understanding the foot biomechanics, it is key to assess in non weight bearing, weight bearing and during gait.
Orthotic Foot Ankle Assessment[edit | edit source]
- Patient History
- ROM
- Muscle Power
- Sensation/Pain
- Proprioception
- Biomechanical Analysis
- Leg length
1. Patient History[edit | edit source]
- Gait pattern and biomechanical analysis on entrance
- Type of shoes[6]
- Assistive devices
- History of underlying conditions, foot problems and the primary problem affecting the individual on consultation.
2. Range of Motion[edit | edit source]
When testing range of motion to create a foot orthosis, testing should be done a
- Active
- Passive
- Weightbearing
- Non weightbearing
Active and Passive Movements in the Foot and Ankle[7]
- Dorsiflexion/ Plantarflexion - Quick test for the Ankle Joint
- Pronation/ Supination – Quick test for the Subtalar joint
- Eversion/ Inversion
- Abduction/ Adduction
- Toe flexion/ extension – Quick test for the Metatarsal Phalangeal joints
Non weight bearing assessment[7]
- Windlass Test - can be effective in examining dysfunction of the plantar fascia although specificity has not been proved.
- Passively extend hallux at MTP joint
- Plantar aponeurosis should tighten and reduces dist between calcaneus and Metatarsals.
- Note angle of extension to initiate arch, can vary
- Increase MLA
- Positive Test = A positive test is considered if passive extension is continued to end range or until the patient's pain is reproduced in Plantarfascitis
- Passively extend hallux at MTP joint
- Pain in medial calcaneus and plantarfascia on palpation
- Hallux Limitus/rigidus
- Both affect the windlass mechanism and gait pattern and normal functioning of the foot.
- Hallux Rigidus[8]
- Very limited dorsiflexion mobility or no mvt. there is crepitation with joint mobilization and pain associated with any movement of the first MTP joint.
- Hallux Limitus[9] (FnHL)
- Reduced dorsiflexion movement, resulting in reduced range of dorsiflexion of the first MTP joint.
- In gait, loss of metatarsophalangeal joint extension during the second half of the single-support phase, when the weightbearing foot is in maximal dorsiflexion.
- Hallux Rigidus[8]
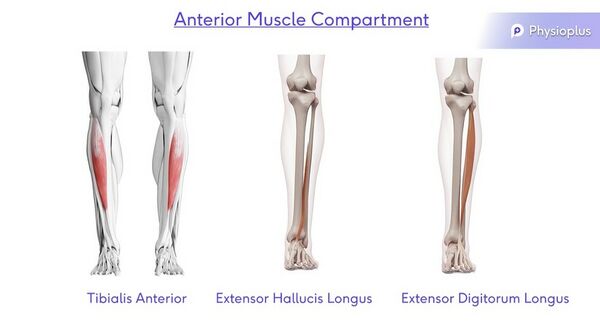
3. Muscles of the Foot and Ankle[edit | edit source]
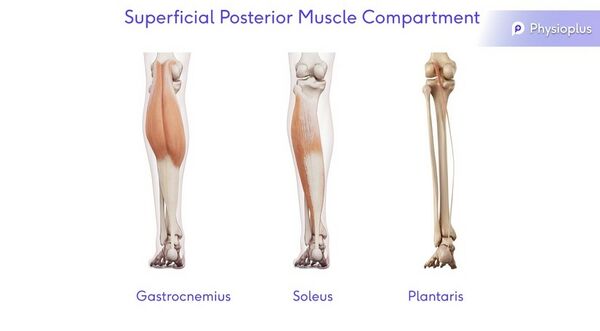
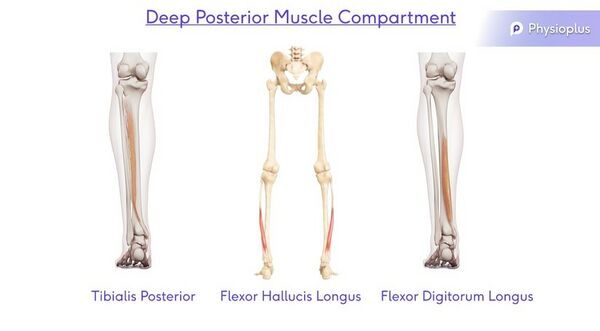
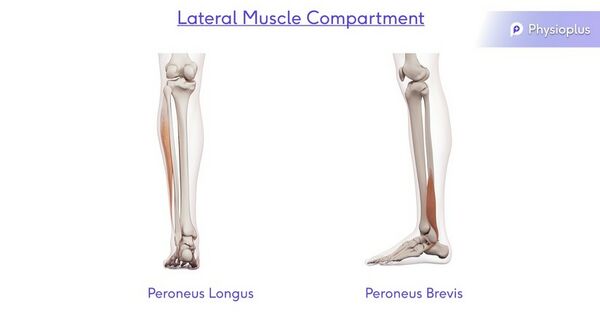
There are four muscle compartments in the lower leg. These muscles are all tested using the standardized Oxford Scale.
Superficial Posterior Muscle Compartment
Action: Plantarflexion
Muscles: Gastrocnemius, Soleus and Plantaris
Deep Posterior Muscle Compartment
Action: Plantarflexion, Adduction and Inversion
Muscles: Tibialis Posterior, Flexor Hallicus Longus and Flexor Digitorum Longus
Lateral Muscle Compartment
Action: Dorsiflexion, Abduction and Eversion
Muscles: Peroneus Longus and Peroneus Brevis
Anterior Muscle Compartment
Action: Dorsiflexion, Abduction and Inversion
Muscles: Tibialis Anterior, Extensor Hallicus Longus and Extensor Digitorum Longus
See the following pages for more information on the muscle testing of:
4. Sensation/Pain[edit | edit source]
5. Proprioception[edit | edit source]
6. Biomechanical Analysis[edit | edit source]
Static
- Overall biomechanics of standing, knees hips pelvis
- STJt alignment – medial/lateral devn- supination
- resistance test
- Too many toes, 1 & 4/5, more lateral more pronated
- Rear foot/forefoot
- Hallux extension – Jacks, Windlass test
- Root V STJt equilibrium
- Sub Talar Joint Equilibrium -K. Kirby
- (2001)
- Spatial location of the subtalar joint
- axis in relation to the weightbearing
- structures of the plantar foot
- • concept of subtalar joint rotational
- equilibrium
- • externally generated forces, such as
- GRF and internally generated forces,
- such as ligamentous and tendon
- tensile forces and joint compression
- forces, affect the mechanical
- behavior of the foot and lower
- extremity
- • Root Theory Model -Root (1954 – 1966)
- • Basis was to classify normal & abnormal foot
- types (osseous alignment). › “
- • Normal/ideal foot alignment occurs when:
- • Distal 1/3 of leg vertical
- • Calcaneus vertical to supporting surface
- • Plantar forefoot parallel to plantar rearfoot
- • Variations from this “normal’ foot alignment
- (‘intrinsic foot deformities’) lead to abnormal
- foot function
- Sub Talar Joint Equilibruim
- Kirby 2001
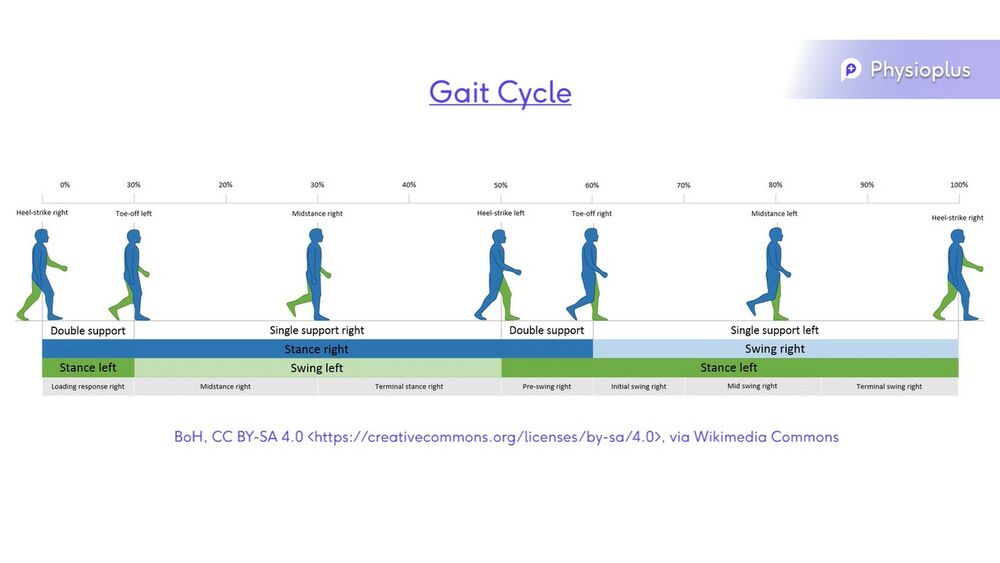
Dynamic Normal Walking[7]
- o IC heel strike,
- o Loading response
- o MS mid stance, single
- o Terminal stance, single
- o Pre swing
- o Swing Phase
- o ground clearance,
- o Single 40% /
- double support
- 60%
- o Timing- load rate=
- stress
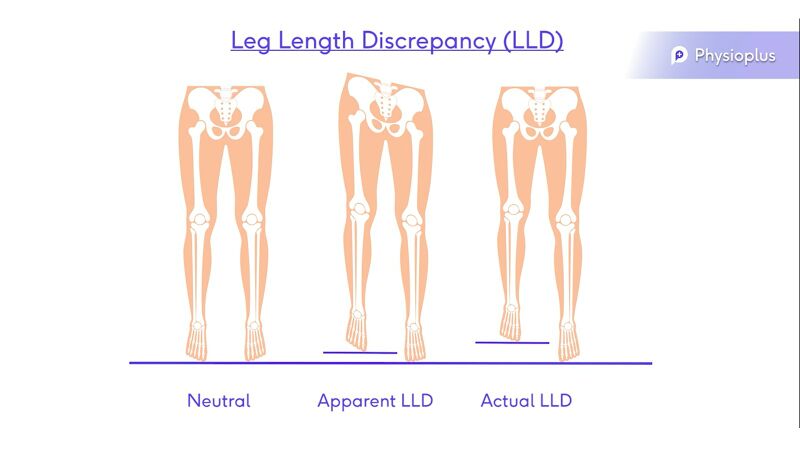
7. Leg Length Discrepancy (LLD)[edit | edit source]
- Dipping
- Pelvic Obliquity
- Retraction
- Scoliosis
- Apparent leg length
- Actual leg length[10]
- ↑ Elattar O, Smith T, Ferguson A, Farber D, Wapner K. Uses of braces and orthotics for conservative management of foot and ankle disorders. Foot & Ankle Orthopaedics. 2018 Aug 3;3(3):2473011418780700.
- ↑ Welte L, Kelly LA, Kessler SE, Lieberman DE, D'Andrea SE, Lichtwark GA, Rainbow MJ. The extensibility of the plantar fascia influences the windlass mechanism during human running. Proceedings of the Royal Society B. 2021 Jan 27;288(1943):20202095.
- ↑ Sichting F, Holowka NB, Ebrecht F, Lieberman DE. Evolutionary anatomy of the plantar aponeurosis in primates, including humans. Journal of anatomy. 2020 Jul;237(1):85-104.
- ↑ Sichting F, Ebrecht F. The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism. PloS one. 2021 Apr 8;16(4):e0249965.
- ↑ Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan;39(1):77.
- ↑ Gegen ME, Plummer T, Darr N. An Exploratory Study of The Perceptions of Footwear for Individuals who use Lower Limb Orthotics. Internet Journal of Allied Health Sciences and Practice. 2020;18(4):8.
- ↑ 7.0 7.1 7.2 Alazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World journal of orthopedics. 2017 Jan 18;8(1):21.
- ↑ Colò G, Fusini F, Samaila EM, Rava A, Felli L, Alessio-Mazzola M, Magnan B. The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature. Acta Bio Medica: Atenei Parmensis. 2020;91(Suppl 14).
- ↑ Graydon M. Hallux Limitus/Rigidus. Clinical Practice Guidelines. 2018:140.
- ↑ Menez C, L'Hermette M, Coquart J. Orthotic insoles improve gait symmetry and reduce immediate pain in subjects with mild leg length discrepancy. Frontiers in sports and active living. 2020;2.