Feeding and Eating Considerations in Cerebral Palsy: Difference between revisions
No edit summary |
No edit summary |
||
| (30 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: | '''Original Editor '''- [[User:Teona Darchia|Teona Darchia]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Feeding is a | Feeding is a vital part of everyday life. Healthy and nutritious foods are essential for brain development, so feeding plays an essential role in the development of motor and cognitive functions.<ref name=":0">Ferluga ED, Archer KR, Sathe NA, Krishnaswami S, Klint A, Lindegren, McPheeters ML. Interventions for Feeding and Nutrition in Cerebral Palsy [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Mar. (Comparative Effectiveness Reviews, No. 94.) Introduction. Available from https://www.ncbi.nlm.nih.gov/books/NBK132442/ [last access 25.01.2024]</ref> Poor nutritional status is common in children with [[Cerebral Palsy Aetiology and Pathology|cerebral palsy]] because of [[Feeding the Child with Cerebral Palsy|feeding]] and swallowing problems. Untreated feeding issues may lead to growth failure, chronic aspiration, oesophagitis, and [[Aspiration Pneumonia|respiratory infections]].<ref name=":0" /> They can also impact a child's social, emotional, and cognitive function and significantly increase caregiver stress.<ref>Greer AJ, Gulotta CS, Masler EA, Laud RB. Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. J Pediatr Psychol. 2008 Jul;33(6):612-20. </ref> This article overviews problems and potential solutions for children with cerebral palsy who experience eating and swallowing difficulties. | ||
== Feeding and Swallowing Disorders == | == Feeding and Swallowing Disorders == | ||
<blockquote>Paediatric '''Feeding Disorder''' is "an impaired oral intake that is not age-appropriate, and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction."<ref name=":1">Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Feuling MB, Noel RJ, Gisel E, Kenzer A, Kessler DB, Kraus de Camargo O, Browne J, Phalen JA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6314510/pdf/jpga-68-124.pdf Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework.] J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):124-129.</ref></blockquote>Dysphagia is a '''swallowing problem''' that places the child at risk for aspiration with oral feeding. Aspiration may | <blockquote>Paediatric '''Feeding Disorder''' is "an impaired oral intake that is not age-appropriate, and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction."<ref name=":1">Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Feuling MB, Noel RJ, Gisel E, Kenzer A, Kessler DB, Kraus de Camargo O, Browne J, Phalen JA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6314510/pdf/jpga-68-124.pdf Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework.] J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):124-129.</ref></blockquote><blockquote>[[Dysphagia]] is a '''swallowing problem''' that places the child at risk for aspiration with oral feeding. Aspiration may have life-threatening pulmonary consequences.<ref>Arvedson JC. [https://www.nature.com/articles/ejcn2013224 Feeding children with cerebral palsy and swallowing difficulties.] Eur J Clin Nutr. 2013 Dec;67 Suppl 2:S9-12. </ref></blockquote> | ||
== Mechanics of Feeding and Swallowing == | == Mechanics of Feeding and Swallowing == | ||
=== Feeding === | === Feeding === | ||
The feeding | The feeding / eating process has four phases: | ||
Phase 1: Opening the mouth | * Phase 1: Opening the mouth | ||
* Phase 2: Using utensils and placing the food or liquid in the mouth | |||
* Phase 3: Closing the mouth to prevent food or liquid from spilling out | |||
* Phase 4: Chewing the food and moving it around to prepare to swallow | |||
[[File:Shutterstock -Swallowing ID 119134822.jpg|thumb|400x400px|Swallowing phases]] | |||
=== Swallowing === | === Swallowing === | ||
Swallowing (deglutition) is the process by which food passes from the mouth through the pharynx and into the oesophagus.<ref>Panara K, Ramezanpour Ahangar E, Padalia D. Physiology, Swallowing. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from https://www.ncbi.nlm.nih.gov/books/NBK541071/ [last access 28.01.2023]</ref> It | Swallowing (deglutition) is the process by which food passes from the mouth through the pharynx and into the oesophagus.<ref>Panara K, Ramezanpour Ahangar E, Padalia D. Physiology, Swallowing. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from https://www.ncbi.nlm.nih.gov/books/NBK541071/ [last access 28.01.2023]</ref> It must be coordinated with breathing because both processes share the same entrance to the pharynx. Failure of coordination between breathing and swallowing can result in choking or pulmonary aspiration. | ||
Swallowing occurs in three phases: | Swallowing occurs in three phases: | ||
Phase 1: Oral phase | * Phase 1: Oral phase | ||
* Phase 2: Pharyngeal phase | |||
Phase 2: Pharyngeal | * Phase 3: Oesophageal phase | ||
Phase 3: Oesophageal | |||
Learn about each | Learn about each swallowing phase [[Feeding and the Swallow Mechanism#Swallowing Mechanism|here]]. | ||
== | == Feeding and Swallowing Challenges in Cerebral Palsy == | ||
=== | === Feeding Challenges === | ||
A child's feeding and eating skills may be affected by motor or sensory challenges.<ref name=":2">Darchia T. Considerations for Feeding in Cerebral Palsy Course. Plus, 2024.</ref> | |||
==== Motor Challenges ==== | ==== Motor Challenges ==== | ||
* Poor head and/or trunk alignment in midline | * [[The Relationship Between Posture and Swallowing|Poor head and / or trunk alignment]] in midline; the posture can be either too flexed or hyperextended | ||
* Increased muscle tone and involuntary body movements | * Increased muscle tone and involuntary body movements | ||
* | * Unable to close the mouth due to increased or decreased resting tone of the jaw muscles | ||
* | * Unable to open the mouth due to jaw-muscle tension | ||
* Uncoordinated, non graded, or limited movements of the jaw leading to lack of jaw rotation movement and limited or lack of ability to chew | * Uncoordinated, non-graded, or limited movements of the jaw, leading to a lack of jaw rotation movement and a limited, or lack of, ability to chew | ||
* Passive lips, lack of lip closure and spoon clearance | * Passive lips, lack of lip closure and spoon clearance | ||
* Difficulty forming | * Difficulty forming a bolus in the mouth | ||
* Food accumulating in the mouth | |||
* Poor saliva control | * Poor saliva control | ||
==== Sensory Challenges ==== | ==== Sensory Challenges ==== | ||
* Hypersensitivity to certain textures or stimuli ( taste, smell, temperature, visual aspect of food) | * Hypersensitivity to certain textures or stimuli (taste, smell, temperature, visual aspect of food) | ||
* Difficulty discriminating tactile sensations (preference for crunchy, chewy foods) | * Difficulty discriminating tactile sensations (preference for crunchy, chewy foods) | ||
* Difficulty in the perception of gustatory and olfactory stimuli (preference for sour and spicy food and refusal to eat balanced or mild tastes) | * Difficulty in the perception of gustatory (taste) and olfactory (smell) stimuli (preference for sour and spicy food and refusal to eat balanced or mild tastes) | ||
* Difficulty accepting new food experiences | * Difficulty accepting new food experiences | ||
* Avoiding behaviour towards a primary caregiver | |||
=== | === Swallowing Challenges === | ||
* Lack of stability in the lower jaw, so there isn't an adequate base of support for selective tongue movements in all directions | |||
** poor tongue control affects bolus transport, delays the initiation of swallowing, and reduces pharyngeal motility<ref>Wahyuni LK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9868261/pdf/fneur-13-1076316.pdf Multisystem compensations and consequences in spastic quadriplegic cerebral palsy children.] Front Neurol. 2023 Jan 9;13:1076316</ref> | |||
* Lack of stability | |||
* Irregular swallow | * Irregular swallow | ||
* Needing extra work or time to chew or swallow | |||
* Needing extra work or time to chew or swallow | |||
* Having food or liquid leak from the mouth | * Having food or liquid leak from the mouth | ||
* | * Getting food stuck in the mouth<ref name=":2" /> | ||
* | |||
* | == Clinical Signs of Feeding and Swallowing Problems in Children == | ||
A child may display the following signs of feeding and swallowing difficulties:<ref name=":2" /> | |||
* difficulty breastfeeding or bottle feeding | |||
* cries or gets worried, excited or agitated during feeding | |||
* does not follow feeding developmental milestones | |||
*coughs during or right after eating or drinking | |||
* often clears throat | |||
* often vomits or shows signs of vomiting while eating | |||
* food flows from the mouth or nose during feeding | |||
* poor food ration | |||
* long duration of feeding | |||
* has a wet or gurgly voice during or after eating or drinking | |||
* feels like something is stuck in the throat or chest | |||
* has difficulty drinking from a cup | |||
* has problems with breathing after meals | |||
* has difficulty gaining weight or is experiencing weight loss | |||
* behavioural challenges | |||
== Factors Influencing Child's Feeding and Eating Skills == | == Factors Influencing a Child's Feeding and Eating Skills == | ||
'''Environmental factors:''' | '''Environmental factors:''' Environmental distractions can decrease a child's ability to concentrate on feeding and eating. Distractions include watching television, looking at a computer, bringing toys to mealtime, and having meals in chaotic, crowded environments with people having loud conversations.<ref>Sdravou K, Emmanouilidou-Fotoulaki E, Printza A, Andreoulakis E, Evangeliou A, Fotoulaki M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7912501/pdf/children-08-00077.pdf Mealtime Environment and Control of Food Intake in Healthy Children and in Children with Gastrointestinal Diseases.] Children (Basel). 2021 Jan 23;8(2):77.</ref> | ||
'''Physical difficulties''': | '''Physical difficulties''': A child's oral motor difficulties may prevent them from eating independently and increase the time and energy spent on feeding and eating.<ref name=":2" /> | ||
'''Behavioural factors''': | '''Behavioural factors''': Caregiver stress and a child's negative mood affect feeding and eating. Caregivers who remain calm / in control emotionally can positively impact a child's behaviour during feeding.<ref name=":2" /> | ||
== Healthcare Team Responsibilities == | == Healthcare Team Responsibilities == | ||
Feeding difficulties can impact different areas of a child's life, including medical, nutritional and psychosocial aspects. Thus, an interdisciplinary team is needed to treat children with feeding and eating difficulties. | |||
=== Speech | === Speech Language Therapist / Pathologist === | ||
Communication, speech and language pathologist is responsible for the following:<ref>Maggioni L, Araújo CM. [http://pepsic.bvsalud.org/pdf/rbcdh/v30n1/08.pdf Guidelines and practices on feeding children with cerebral palsy.] Journal of Human Growth and Development. 2020 Apr;30(1):65-74.</ref> | A [[Communication and Children with Cerebral Palsy|communication]], speech and language therapist (pathologist) is responsible for the following:<ref>Maggioni L, Araújo CM. [http://pepsic.bvsalud.org/pdf/rbcdh/v30n1/08.pdf Guidelines and practices on feeding children with cerebral palsy.] Journal of Human Growth and Development. 2020 Apr;30(1):65-74.</ref> | ||
* | * assessing the function of feeding | ||
* | * helping to determine the diagnosis and aetiology of dysphagia | ||
* | * assessing the protective capacity of the respiratory system | ||
* | * indicating alternative ways of eating | ||
* | * providing direct and indirect interventions, such as strengthening facial muscles, teaching different strategies to develop sucking, chewing, and drinking skills, tasting new food and drink with rich flavours and aromas, and modifying food liquid to improve swallowing<ref name=":2" /> | ||
* | * guiding staff and caregivers in better management of feeding difficulties<ref name=":2" /> | ||
=== Occupational Therapist === | === Occupational Therapist === | ||
The occupational therapy assessment of | The [[Occupational Therapy for Children|occupational therapy]] assessment of a child with feeding and eating needs should consider their independence and safety, and include the following aspects:<ref name=":1" /> | ||
* | * motor and sensory skills assessment | ||
* | * muscle strength assessment | ||
* | * observation of the child's behaviour and environmental factors around mealtimes | ||
The occupational | The occupational therapy intervention focuses on:<ref name=":2" /> | ||
* | * improving oral motor skills | ||
* | * sensory processing | ||
* | * promoting correct posture | ||
* | * selecting adaptive devices and choosing strategies to use them functionally | ||
* | * adjusting and adapting the environment to promote independent eating | ||
* | * working with parents and caregivers on using different feeding methods or techniques | ||
=== Physical Therapist === | === Physiotherapist / Physical Therapist === | ||
Physiotherapy interventions are part of oral motor therapy (OMT).<ref name=":3">Widman-Valencia ME, Gongora-Meza LF, Rubio-Zapata H, Zapata-Vázquez RE, Lizama EV, Salomón MR, Estrella-Castillo D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8560295/pdf/BN2021-6299462.pdf Oral Motor Treatment Efficacy: Feeding and Swallowing Skills in Children with Cerebral Palsy]. Behav Neurol. 2021 Oct 25;2021:6299462.</ref> OMT can improve a child's functional independence and quality of life.<ref>Sığan SN, Uzunhan TA, Aydınlı N, Eraslan E, Ekici B, Calışkan M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3788277/pdf/AIAN-16-342.pdf Effects of oral motor therapy in children with cerebral palsy.] Ann Indian Acad Neurol. 2013 Jul;16(3):342-6. </ref> Protocols for OMT vary and may include the following: | |||
* | * passive range of motion exercises <ref name=":3" /> | ||
* | * active-assistive range of motion exercises<ref name=":3" /> | ||
* | * oral motor facilitation technique (OMFT)<ref name=":4">Min KC, Seo SM, Woo HS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9632014/pdf/12887_2022_Article_3674.pdf Effect of oral motor facilitation technique on oral motor and feeding skills in children with cerebral palsy: a case study.] BMC Pediatr. 2022 Nov 3;22(1):626.</ref> | ||
* | * passive sensory stimulation of the muscles of the face and mouth with different textures and therapeutic devices<ref name=":4" /> | ||
* Relaxation techniques for muscles responsible for sucking, swallowing, and chewing | * [[Relaxation Techniques|relaxation techniques]] for the muscles responsible for sucking, swallowing, and chewing<ref name=":5">Szuflak K, Malak R, Fechner B, Sikorska D, Samborski W, Mojs E, Gerreth K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10094554/pdf/healthcare-11-01029.pdf The Masticatory Structure and Function in Children with Cerebral Palsy-A Pilot Study.] Healthcare (Basel). 2023 Apr 4;11(7):1029. </ref> | ||
* | * strain-counter strain technique may be used to help relax tensed muscles, including the masseter and sternocleidomastoid muscles<ref name=":5" /> | ||
== Feeding and Eating Management Strategies == | == Feeding and Eating Management Strategies == | ||
=== Goals and Outcomes === | === Goals and Outcomes === | ||
'''General goal''': "to improve the quality of life for both the child and family, through interventions that maximise independence in activities of daily living, mobility, and nutrition". <ref name=":0" /> | '''General goal''': "to improve the quality of life for both the child and family, through interventions that maximise independence in activities of daily living, mobility, and nutrition".<ref name=":0" /> | ||
The '''outcomes''' will vary and depend on the following:<ref name=":0" /> | |||
* type of cerebral palsy: spastic vs nonspastic | |||
* location of motor involvement: diplegia, quadriplegia, etc. | |||
* the child's functional status, including their ability to walk or sit and the degree of head and trunk control | |||
=== Treatment Strategies === | |||
* | * Establish a '''feeding routine''' | ||
* | * Promote '''correct posture''' during meal times and beyond (see images below) | ||
* the child' | ** use appropriate seating equipment and / or handling techniques to ensure the child's head / trunk are aligned and upright | ||
** facilitate chin tuck and elongation of the back of the neck in a midline neutral position | |||
** provide adequate postural stability | |||
*** stable base of support for the trunk, hips, knees and feet | |||
***hips symmetrically flexed at around 90° | |||
*** use a tray to support arms | |||
*** use a headrest to support the head and the neck | |||
** maintain the child's correct posture outside of mealtime | |||
** use oral appliances to help stabilise the jaw, improve sucking, tongue coordination, lip control, and chewing<ref name=":0" /> | |||
<gallery widths="250" heights="350"> | |||
File:Correct wc position.jpeg|'''Correct''' sitting posture in the wheelchair. | |||
File:Incorrect wc posture.jpeg|'''Incorrect''' sitting posture in the wheelchair. | |||
</gallery> | |||
This video suggests various parenting / caregiver strategies to promote correct posture for children during meal time:{{#ev:youtube|v=yRrO80gIOTY|300}}<ref>Special Education Professionals. Best Feeding Position for Children with Feeding Disorders. Available from: https://www.youtube.com/watch?v=yRrO80gIOTY [last accessed 29/01/2024]</ref> | |||
=== | * Promote '''independence with eating''' | ||
** the quantity of food on the spoon or fork should be manageable for the child | |||
** provide hand-over-hand assistance and gradually decrease the assistance provided as the child's motor control improves<ref name=":6">Feeding the Child with Cerebral Palsy. Available from [[Feeding the Child with Cerebral Palsy]] [last access 29.01.2024]</ref> | |||
** introduce assisted eating for part of the meal or snack<ref name=":6" /> | |||
Please watch this video if you would like to learn about general strategies to promote independence with eating: | |||
{{#ev:youtube|v=SDrjTYk1cgw|300}}<ref>Children's Health Queensland. Responsive feeding: Developing Independence. Available from: https://www.youtube.com/watch?v=SDrjTYk1cgw [last accessed 29/01/2024]</ref> | |||
* Increase '''food acceptability''' through sensory stimuli | |||
** allow the child to touch the food and smell it before trying to eat it<ref>Warmbrodt R. Cerebral Palsy Eating and Feeding Tips. Available from https://www.cerebralpalsyguidance.com/cerebral-palsy/living/eating-and-feeding-tips/ [last access 29.01.2024]</ref> | |||
* Use '''adaptive equipment''' as needed<ref name=":2" /> | |||
** children with sucking difficulties may benefit from the introduction of a drinking cup | |||
** [[File:U-shaped cup.png|thumb|U-shaped cup]]using a U-shaped cut-out cup for drinking means a child doesn't have to pull their neck or head back while drinking | |||
** a shallow-bowled spoon can help a child remove food from the spoon through lip closure | |||
** an angled spoon requires less wrist movement to bring food to the mouth | |||
** using a spoon or fork that is attached to the hand by a Universal cuff helps children with a weak grasp hold utensils | |||
** using scoop plates and plates with a silicone base can help children scoop food off the plate | |||
** using a feeding chair with a tray attached to the front helps with postural alignment | |||
# | Please watch the video below if you would like to see a demonstration of various types of adaptive feeding equipment:{{#ev:youtube|v=oM18pNUixM8|300}}<ref>The Watson Institute Pittsburgh. Adaptive Feeding Equipment. Available from: https://www.youtube.com/watch?v=oM18pNUixM8 [last accessed 29/01/2024]</ref> | ||
* Consider '''play elements''' to support a child's willingness and enjoyment during the feeding process | |||
* Introduce a '''variety of foods''' to play with | |||
** change the viscosity of liquids<ref name=":7">Borowitz KC, Borowitz SM. [https://www.oslo-universitetssykehus.no/49a787/contentassets/eff5346b78e14cc48a6b46781477134d/dokumenter/feeding-problems-in-infants-and-children.pdf Feeding Problems in Infants and Children: Assessment and Etiology.] Pediatr Clin North Am. 2018 Feb;65(1):59-72.</ref> | |||
** increase or decrease the consistency of solids offered<ref name=":7" /> | |||
** add supplemental feeds when needed<ref name=":7" /> | |||
* Organise '''the environment''' | |||
** create a quiet environment | |||
** slowly introduce an element of distraction when the child’s ability progresses (e.g. start with background sounds like a radio) | |||
** the caregiver / person feeding or assisting with eating should be in front of the child, in their midline, to facilitate communication with the child | |||
== Resources == | == Resources == | ||
| Line 177: | Line 194: | ||
<references /> | <references /> | ||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Course Pages]] | |||
[[Category:Rehabilitation]] | |||
[[Category:Cerebral Palsy]] | |||
Latest revision as of 18:34, 29 February 2024
Original Editor - Teona Darchia
Top Contributors - Ewa Jaraczewska, Jess Bell, Tarina van der Stockt and Kim Jackson
Introduction[edit | edit source]
Feeding is a vital part of everyday life. Healthy and nutritious foods are essential for brain development, so feeding plays an essential role in the development of motor and cognitive functions.[1] Poor nutritional status is common in children with cerebral palsy because of feeding and swallowing problems. Untreated feeding issues may lead to growth failure, chronic aspiration, oesophagitis, and respiratory infections.[1] They can also impact a child's social, emotional, and cognitive function and significantly increase caregiver stress.[2] This article overviews problems and potential solutions for children with cerebral palsy who experience eating and swallowing difficulties.
Feeding and Swallowing Disorders[edit | edit source]
Paediatric Feeding Disorder is "an impaired oral intake that is not age-appropriate, and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction."[3]
Dysphagia is a swallowing problem that places the child at risk for aspiration with oral feeding. Aspiration may have life-threatening pulmonary consequences.[4]
Mechanics of Feeding and Swallowing[edit | edit source]
Feeding[edit | edit source]
The feeding / eating process has four phases:
- Phase 1: Opening the mouth
- Phase 2: Using utensils and placing the food or liquid in the mouth
- Phase 3: Closing the mouth to prevent food or liquid from spilling out
- Phase 4: Chewing the food and moving it around to prepare to swallow
Swallowing[edit | edit source]
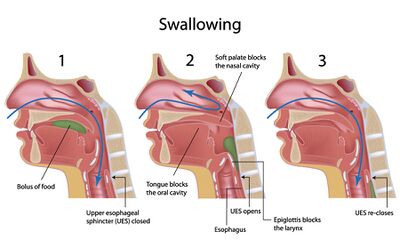
Swallowing (deglutition) is the process by which food passes from the mouth through the pharynx and into the oesophagus.[5] It must be coordinated with breathing because both processes share the same entrance to the pharynx. Failure of coordination between breathing and swallowing can result in choking or pulmonary aspiration.
Swallowing occurs in three phases:
- Phase 1: Oral phase
- Phase 2: Pharyngeal phase
- Phase 3: Oesophageal phase
Learn about each swallowing phase here.
Feeding and Swallowing Challenges in Cerebral Palsy[edit | edit source]
Feeding Challenges[edit | edit source]
A child's feeding and eating skills may be affected by motor or sensory challenges.[6]
Motor Challenges[edit | edit source]
- Poor head and / or trunk alignment in midline; the posture can be either too flexed or hyperextended
- Increased muscle tone and involuntary body movements
- Unable to close the mouth due to increased or decreased resting tone of the jaw muscles
- Unable to open the mouth due to jaw-muscle tension
- Uncoordinated, non-graded, or limited movements of the jaw, leading to a lack of jaw rotation movement and a limited, or lack of, ability to chew
- Passive lips, lack of lip closure and spoon clearance
- Difficulty forming a bolus in the mouth
- Food accumulating in the mouth
- Poor saliva control
Sensory Challenges[edit | edit source]
- Hypersensitivity to certain textures or stimuli (taste, smell, temperature, visual aspect of food)
- Difficulty discriminating tactile sensations (preference for crunchy, chewy foods)
- Difficulty in the perception of gustatory (taste) and olfactory (smell) stimuli (preference for sour and spicy food and refusal to eat balanced or mild tastes)
- Difficulty accepting new food experiences
- Avoiding behaviour towards a primary caregiver
Swallowing Challenges[edit | edit source]
- Lack of stability in the lower jaw, so there isn't an adequate base of support for selective tongue movements in all directions
- poor tongue control affects bolus transport, delays the initiation of swallowing, and reduces pharyngeal motility[7]
- Irregular swallow
- Needing extra work or time to chew or swallow
- Having food or liquid leak from the mouth
- Getting food stuck in the mouth[6]
Clinical Signs of Feeding and Swallowing Problems in Children[edit | edit source]
A child may display the following signs of feeding and swallowing difficulties:[6]
- difficulty breastfeeding or bottle feeding
- cries or gets worried, excited or agitated during feeding
- does not follow feeding developmental milestones
- coughs during or right after eating or drinking
- often clears throat
- often vomits or shows signs of vomiting while eating
- food flows from the mouth or nose during feeding
- poor food ration
- long duration of feeding
- has a wet or gurgly voice during or after eating or drinking
- feels like something is stuck in the throat or chest
- has difficulty drinking from a cup
- has problems with breathing after meals
- has difficulty gaining weight or is experiencing weight loss
- behavioural challenges
Factors Influencing a Child's Feeding and Eating Skills[edit | edit source]
Environmental factors: Environmental distractions can decrease a child's ability to concentrate on feeding and eating. Distractions include watching television, looking at a computer, bringing toys to mealtime, and having meals in chaotic, crowded environments with people having loud conversations.[8]
Physical difficulties: A child's oral motor difficulties may prevent them from eating independently and increase the time and energy spent on feeding and eating.[6]
Behavioural factors: Caregiver stress and a child's negative mood affect feeding and eating. Caregivers who remain calm / in control emotionally can positively impact a child's behaviour during feeding.[6]
Healthcare Team Responsibilities[edit | edit source]
Feeding difficulties can impact different areas of a child's life, including medical, nutritional and psychosocial aspects. Thus, an interdisciplinary team is needed to treat children with feeding and eating difficulties.
Speech Language Therapist / Pathologist[edit | edit source]
A communication, speech and language therapist (pathologist) is responsible for the following:[9]
- assessing the function of feeding
- helping to determine the diagnosis and aetiology of dysphagia
- assessing the protective capacity of the respiratory system
- indicating alternative ways of eating
- providing direct and indirect interventions, such as strengthening facial muscles, teaching different strategies to develop sucking, chewing, and drinking skills, tasting new food and drink with rich flavours and aromas, and modifying food liquid to improve swallowing[6]
- guiding staff and caregivers in better management of feeding difficulties[6]
Occupational Therapist[edit | edit source]
The occupational therapy assessment of a child with feeding and eating needs should consider their independence and safety, and include the following aspects:[3]
- motor and sensory skills assessment
- muscle strength assessment
- observation of the child's behaviour and environmental factors around mealtimes
The occupational therapy intervention focuses on:[6]
- improving oral motor skills
- sensory processing
- promoting correct posture
- selecting adaptive devices and choosing strategies to use them functionally
- adjusting and adapting the environment to promote independent eating
- working with parents and caregivers on using different feeding methods or techniques
Physiotherapist / Physical Therapist[edit | edit source]
Physiotherapy interventions are part of oral motor therapy (OMT).[10] OMT can improve a child's functional independence and quality of life.[11] Protocols for OMT vary and may include the following:
- passive range of motion exercises [10]
- active-assistive range of motion exercises[10]
- oral motor facilitation technique (OMFT)[12]
- passive sensory stimulation of the muscles of the face and mouth with different textures and therapeutic devices[12]
- relaxation techniques for the muscles responsible for sucking, swallowing, and chewing[13]
- strain-counter strain technique may be used to help relax tensed muscles, including the masseter and sternocleidomastoid muscles[13]
Feeding and Eating Management Strategies[edit | edit source]
Goals and Outcomes[edit | edit source]
General goal: "to improve the quality of life for both the child and family, through interventions that maximise independence in activities of daily living, mobility, and nutrition".[1]
The outcomes will vary and depend on the following:[1]
- type of cerebral palsy: spastic vs nonspastic
- location of motor involvement: diplegia, quadriplegia, etc.
- the child's functional status, including their ability to walk or sit and the degree of head and trunk control
Treatment Strategies[edit | edit source]
- Establish a feeding routine
- Promote correct posture during meal times and beyond (see images below)
- use appropriate seating equipment and / or handling techniques to ensure the child's head / trunk are aligned and upright
- facilitate chin tuck and elongation of the back of the neck in a midline neutral position
- provide adequate postural stability
- stable base of support for the trunk, hips, knees and feet
- hips symmetrically flexed at around 90°
- use a tray to support arms
- use a headrest to support the head and the neck
- maintain the child's correct posture outside of mealtime
- use oral appliances to help stabilise the jaw, improve sucking, tongue coordination, lip control, and chewing[1]
This video suggests various parenting / caregiver strategies to promote correct posture for children during meal time:
- Promote independence with eating
Please watch this video if you would like to learn about general strategies to promote independence with eating:
- Increase food acceptability through sensory stimuli
- allow the child to touch the food and smell it before trying to eat it[17]
- Use adaptive equipment as needed[6]
- children with sucking difficulties may benefit from the introduction of a drinking cup
- using a U-shaped cut-out cup for drinking means a child doesn't have to pull their neck or head back while drinking
- a shallow-bowled spoon can help a child remove food from the spoon through lip closure
- an angled spoon requires less wrist movement to bring food to the mouth
- using a spoon or fork that is attached to the hand by a Universal cuff helps children with a weak grasp hold utensils
- using scoop plates and plates with a silicone base can help children scoop food off the plate
- using a feeding chair with a tray attached to the front helps with postural alignment
Please watch the video below if you would like to see a demonstration of various types of adaptive feeding equipment:
- Consider play elements to support a child's willingness and enjoyment during the feeding process
- Introduce a variety of foods to play with
- Organise the environment
- create a quiet environment
- slowly introduce an element of distraction when the child’s ability progresses (e.g. start with background sounds like a radio)
- the caregiver / person feeding or assisting with eating should be in front of the child, in their midline, to facilitate communication with the child
Resources[edit | edit source]
- Module 6. Feeding Your Child. In: GETTING TO KNOW CEREBRAL PALSY
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Ferluga ED, Archer KR, Sathe NA, Krishnaswami S, Klint A, Lindegren, McPheeters ML. Interventions for Feeding and Nutrition in Cerebral Palsy [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Mar. (Comparative Effectiveness Reviews, No. 94.) Introduction. Available from https://www.ncbi.nlm.nih.gov/books/NBK132442/ [last access 25.01.2024]
- ↑ Greer AJ, Gulotta CS, Masler EA, Laud RB. Caregiver stress and outcomes of children with pediatric feeding disorders treated in an intensive interdisciplinary program. J Pediatr Psychol. 2008 Jul;33(6):612-20.
- ↑ 3.0 3.1 Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Feuling MB, Noel RJ, Gisel E, Kenzer A, Kessler DB, Kraus de Camargo O, Browne J, Phalen JA. Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework. J Pediatr Gastroenterol Nutr. 2019 Jan;68(1):124-129.
- ↑ Arvedson JC. Feeding children with cerebral palsy and swallowing difficulties. Eur J Clin Nutr. 2013 Dec;67 Suppl 2:S9-12.
- ↑ Panara K, Ramezanpour Ahangar E, Padalia D. Physiology, Swallowing. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from https://www.ncbi.nlm.nih.gov/books/NBK541071/ [last access 28.01.2023]
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Darchia T. Considerations for Feeding in Cerebral Palsy Course. Plus, 2024.
- ↑ Wahyuni LK. Multisystem compensations and consequences in spastic quadriplegic cerebral palsy children. Front Neurol. 2023 Jan 9;13:1076316
- ↑ Sdravou K, Emmanouilidou-Fotoulaki E, Printza A, Andreoulakis E, Evangeliou A, Fotoulaki M. Mealtime Environment and Control of Food Intake in Healthy Children and in Children with Gastrointestinal Diseases. Children (Basel). 2021 Jan 23;8(2):77.
- ↑ Maggioni L, Araújo CM. Guidelines and practices on feeding children with cerebral palsy. Journal of Human Growth and Development. 2020 Apr;30(1):65-74.
- ↑ 10.0 10.1 10.2 Widman-Valencia ME, Gongora-Meza LF, Rubio-Zapata H, Zapata-Vázquez RE, Lizama EV, Salomón MR, Estrella-Castillo D. Oral Motor Treatment Efficacy: Feeding and Swallowing Skills in Children with Cerebral Palsy. Behav Neurol. 2021 Oct 25;2021:6299462.
- ↑ Sığan SN, Uzunhan TA, Aydınlı N, Eraslan E, Ekici B, Calışkan M. Effects of oral motor therapy in children with cerebral palsy. Ann Indian Acad Neurol. 2013 Jul;16(3):342-6.
- ↑ 12.0 12.1 Min KC, Seo SM, Woo HS. Effect of oral motor facilitation technique on oral motor and feeding skills in children with cerebral palsy: a case study. BMC Pediatr. 2022 Nov 3;22(1):626.
- ↑ 13.0 13.1 Szuflak K, Malak R, Fechner B, Sikorska D, Samborski W, Mojs E, Gerreth K. The Masticatory Structure and Function in Children with Cerebral Palsy-A Pilot Study. Healthcare (Basel). 2023 Apr 4;11(7):1029.
- ↑ Special Education Professionals. Best Feeding Position for Children with Feeding Disorders. Available from: https://www.youtube.com/watch?v=yRrO80gIOTY [last accessed 29/01/2024]
- ↑ 15.0 15.1 Feeding the Child with Cerebral Palsy. Available from Feeding the Child with Cerebral Palsy [last access 29.01.2024]
- ↑ Children's Health Queensland. Responsive feeding: Developing Independence. Available from: https://www.youtube.com/watch?v=SDrjTYk1cgw [last accessed 29/01/2024]
- ↑ Warmbrodt R. Cerebral Palsy Eating and Feeding Tips. Available from https://www.cerebralpalsyguidance.com/cerebral-palsy/living/eating-and-feeding-tips/ [last access 29.01.2024]
- ↑ The Watson Institute Pittsburgh. Adaptive Feeding Equipment. Available from: https://www.youtube.com/watch?v=oM18pNUixM8 [last accessed 29/01/2024]
- ↑ 19.0 19.1 19.2 Borowitz KC, Borowitz SM. Feeding Problems in Infants and Children: Assessment and Etiology. Pediatr Clin North Am. 2018 Feb;65(1):59-72.