Family Centred Intervention and Early Diagnosis: Difference between revisions
(added info from google doc) |
No edit summary |
||
| (42 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> '''Original Editor '''- [[User:Robin Tacchetti|Robin Tacchetti]] based on the course by [https://members.physio-pedia.com/course_tutor/Pam-Versfeld/ Pam Versfeld]<br></div> | ||
'''Original Editor '''- [[User: | |||
</div> | |||
== Early Intervention == | == Early Intervention == | ||
Early intervention services are a | Early intervention services are a set of interventions that support and provide resources for families of special needs infants and toddlers, aged between 0 and 3 years old.<ref name=":3" /><blockquote>Can Child<ref name=":7">CanChild from McMaster University. Available at [https://www.canchild.ca/en/research-in-practice/family-centred-service www.canchild.org]</ref> definition of family centred service: "Family-centred service is made up of a set of values, attitudes, and approaches to services for children with special needs and their families. Family-centred service recognizes that each family is unique; that the family is the constant in the child's life; and that they are the experts on the child's abilities and needs. The family works with service providers to make informed decisions about the services and supports the child and family receive. In family-centred service, the strengths and needs of all family members are considered."<ref name=":7" /> </blockquote>Children with developmental disabilities are entitled to various services. An interdisciplinary early intervention team may include the following disciplines, depending on the family and child’s needs and availability of services:<ref name=":7" /> | ||
* physical therapy / physiotherapy | |||
* | * occupational therapy | ||
* | * speech therapy | ||
* | * vision therapy | ||
* | * nursing | ||
* | * assistive technology | ||
* | * special education | ||
* | Evaluations and follow-up care are provided in the child's least restrictive or natural environment, typically at their home or daycare centre.<ref>Tomasello NM, Manning AR, Dulmus CN. [https://www.tandfonline.com/doi/full/10.1080/10522150903503010 Family-centered early intervention for infants and toddlers with disabilities.] Journal of Family Social Work. 2010 Mar 24;13(2):163-72.</ref> Traditionally, early intervention has worked off an expert model where the therapist created goals and provided follow-up care based on the impairment. Any interventions provided by the family were adjuncts to those provided by the healthcare professional. The overall care and decision making for the child was in the hands of the therapist. This model is referred to as a rehabilitation model.<ref name=":2">Dalmau M, Balcells-Balcells A, Giné C, Cañadas M, Casas O, Salat Y, Farré V, Calaf N. [https://scielo.isciii.es/pdf/ap/v33n3/psicologia_desarrollo2.pdf How to implement the family-centered model in early intervention]. Anales de psicología. 2017;33(3):641-51.</ref> | ||
Evaluations and follow up care | |||
== Family-Centred Care == | == Family-Centred Care == | ||
Over the past decade, there has been a shift from the therapist-driven model to a family education/empowerment model. The family-centred care (FCC) model<ref>McCarthy E, Guerin S. [https://onlinelibrary.wiley.com/doi/epdf/10.1111/cch.12901 Family‐centred care in early intervention: A systematic review of the processes and outcomes of family‐centred care and impacting factors.] Child: Care, Health and Development. 2022 Jan;48(1):1-32.</ref> provides collaboration between the therapist and family where the goals and aspirations of the family are central to the intervention.<ref name=":3">Versfeld, P. Family-Centred Intervention and Early Diagnosis Course. Plus , 2021.</ref> The therapist works as a “coach” helping families identify needs, goals and solutions. FCC, thus, transfers decision-making from just the therapist to the family, who are empowered to create goals and plan intervention strategies.<ref name=":3" /> When families are involved in the care and decisions of their child, the family and the child reap better outcomes.<ref name=":2" /> Additionally, research has shown the FCC model to result in greater parent satisfaction, reduced cost of healthcare, behavioural/emotional support to a child and a faster recovery.<ref>Raghupathy MK, Rao BK, Nayak SR, Spittle AJ, Parsekar SS. [https://link.springer.com/article/10.1186/s13643-021-01612-w Effect of family-centered care interventions on motor and neurobehavior development of very preterm infants: a protocol for systematic review]. Systematic reviews. 2021 Dec;10(1):1-8.</ref> | |||
=== Solution Focused Coaching === | |||
Traditionally, early intervention was problem-oriented with a focus on identifying impairments in the body. Interventions were targeted at fixing the dysfunction and decisions about care were made solely by the therapist. However, with a solution focused coaching (SFC) model, the therapist and family work together to envision possibilities and seek solutions to the family's needs and targeted goals.<ref>Baldwin P, King G, Evans J, McDougall S, Tucker MA, Servais M. [https://www.tandfonline.com/doi/full/10.3109/01942638.2013.784718?scroll=top&needAccess=true Solution-focused coaching in pediatric rehabilitation: an integrated model for practice]. Physical & Occupational Therapy in Pediatrics. 2013 Nov 1;33(4):467-83</ref> <ref name=":3" /> Family empowerment is a priority in FSC. In addition, a solution focused coaching model looks towards the child's strengths and abilities rather than their problems to initiate goal setting and intervention planning.<ref name=":3" /> | |||
== Early Diagnosis and Referral == | |||
=== Cerebral Palsy === | |||
The most common physical disability in childhood is cerebral palsy (CP), occurring in every 1 in 500 births. CP is caused by brain injury early in development and presents with disorders in posture and movement leading to activity limitations.<ref name=":1">Romeo DM, Ricci D, Brogna C, Mercuri E. [https://onlinelibrary.wiley.com/doi/epdf/10.1111/dmcn.12876 Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: a critical review of the literature]. Developmental Medicine & Child Neurology. 2016 Mar;58(3):240-5.</ref> Traditionally, a diagnosis would be concluded between 12 and 24 months of age when symptoms were evident. New research, however, reveals that signs and symptoms of CP appear and develop before 2 years of age. Using a combination of medical history, neuroimaging and standardised motor and neurological assessments for infants under 2, the risk of cerebral palsy can be now be predicted.<ref name=":0">Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC, De Vries LS. [https://jamanetwork.com/journals/jamapediatrics/article-abstract/2636588 Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment]. JAMA pediatrics. 2017 Sep 1;171(9):897-907.</ref> Using diagnostic-specific early assessments can lead to referral of services which will strengthen caregiver well-being, prevent secondary complications and optimise infant cognitive and motor plasticity.<ref>[https://jamanetwork.com/journals/jamapediatrics/article-abstract/2636588 Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy]: Advances in Diagnosis and Treatment. J Novak et al (2017). AMA pediatrics, 2017 171(9), 897–907.</ref> The tools below are commonly used for infants aged under 2 to estimate the risk of a cerebral palsy diagnosis. | |||
( | ==== Hammersmith Infant Neurological Examination ==== | ||
[[File:HINE test.jpg|thumb|500x500px|HINE TEST<ref>De Sanctis R, Coratti G, Pasternak A, Montes J, Pane M, Mazzone ES, Young SD, Salazar R, Quigley J, Pera MC, Antonaci L. [https://www.nmd-journal.com/article/S0960-8966(16)30816-1/fulltext Developmental milestones in type I spinal muscular atrophy]. Neuromuscular Disorders. 2016 Nov 1;26(11):754-9.</ref>|alt=]] | |||
The Hammersmith Infant Neurological Examination (HINE) is a free tool with good interobserver reliability that is typically used on infants aged between 3 and 24 months. It has shown high sensitivity in detecting CP in infants, (98% in infants under 5 months old, 90% in infants over 5 months old).<ref name=":0" /> Neurological function is tested with 26 different criteria based on movements, behaviour, cranial nerve function, protective reactions, reflexes and gross and fine motor function. Symmetry between left and right sides are also scored.<ref name=":3" /> Test results not only identify children at risk, but detail the severity and type of motor impairment. Having this specific information allows early intervention to be targeted to the specific neurological sequelae.<ref name=":1" /> | |||
= | |||
Scores range from 0-73. Romeo et.al<ref name=":1" /> found that infants tested between 3 and 6 months showed the following pattern: | |||
Scores below 40: quadriplegia (IV and V levels of GMFCS), severe diplegia (III level) | |||
Scored 40-60: mild or moderate diplegia (I-II level); hemiplegia (I-II level)<ref name=":1" /> | |||
==== Gross Motor Function Classification System ==== | ==== Gross Motor Function Classification System ==== | ||
The Gross Motor Function Classification System (GMFCS) tool classifies children under 2 into | [https://www.cpqcc.org/sites/default/files/GMFCS-ER.pdf The Gross Motor Function Classification System (GMFCS]) tool classifies children aged under 2 into five distinct levels depending on their self-initiated movement. It specifically focuses on mobility, transfers and sitting. These criteria relate to functional limitations for the child versus quality of movement.<ref name=":6">Palisano R, Rosenbaum P, Bartlett D, Livingston M. [https://www.cpqcc.org/sites/default/files/GMFCS-ER.pdf GMFCS – E & R Gross Motor Function Classification System Expanded and Revised]. Hamilton, ON: CanChild Centre for Childhood Disability Research, McMaster University, 2007.</ref> The GMFC is a way of classifying function severity and not a diagnostic tool. | ||
Gross Motor Function Classification System – Expanded and Revised (GMFCS – E & R) | Gross Motor Function Classification System – Expanded and Revised (GMFCS – E & R) for children aged 2 and under is as follows:<ref name=":6" /> | ||
* LEVEL I: Infants move in and out of sitting and floor sit with both hands free to manipulate objects. Infants crawl on hands and knees, pull to stand and take steps holding on to furniture. Infants walk between 18 months and 2 years of age without the need for any assistive mobility device. | * "LEVEL I: Infants move in and out of sitting and floor sit with both hands free to manipulate objects. Infants crawl on hands and knees, pull to stand and take steps holding on to furniture. Infants walk between 18 months and 2 years of age without the need for any assistive mobility device." | ||
* LEVEL II: Infants maintain floor sitting but may need to use their hands for support to maintain balance. Infants creep on their stomach or crawl on hands and knees. Infants may pull to stand and take steps holding on to furniture. | * LEVEL II: Infants maintain floor sitting but may need to use their hands for support to maintain balance. Infants creep on their stomach or crawl on hands and knees. Infants may pull to stand and take steps holding on to furniture. | ||
* LEVEL III: Infants maintain floor sitting when the low back is supported. Infants roll and creep forward on their stomachs. | * LEVEL III: Infants maintain floor sitting when the low back is supported. Infants roll and creep forward on their stomachs. | ||
* LEVEL IV: Infants have head control but trunk support is required for floor sitting. Infants can roll to supine and may roll to prone. | * LEVEL IV: Infants have head control but trunk support is required for floor sitting. Infants can roll to supine and may roll to prone. | ||
* LEVEL V: Physical impairments limit voluntary control of movement. Infants are unable to maintain antigravity head and trunk postures in prone and sitting. Infants require adult assistance to roll. | * LEVEL V: Physical impairments limit voluntary control of movement. Infants are unable to maintain antigravity head and trunk postures in prone and sitting. Infants require adult assistance to roll." | ||
<br> | |||
<nowiki>***</nowiki> Less | <nowiki>***</nowiki> Less favourable outcomes are noted in low and middle income countries with over 73% of children classified as GMFCS level of III-IV.<ref>Jahan I, Muhit M, Hardianto D, Laryea F, Chhetri AB, Smithers‐Sheedy H, McIntyre S, Badawi N, Khandaker G. [https://onlinelibrary.wiley.com/doi/10.1111/dmcn.14926 Epidemiology of cerebral palsy in low‐and middle‐income countries: preliminary findings from an international multi‐centre cerebral palsy register]. Developmental Medicine & Child Neurology. 2021 May 24.</ref> | ||
==== The Prechtl General Movement Assessment ==== | ==== The Prechtl General Movement Assessment ==== | ||
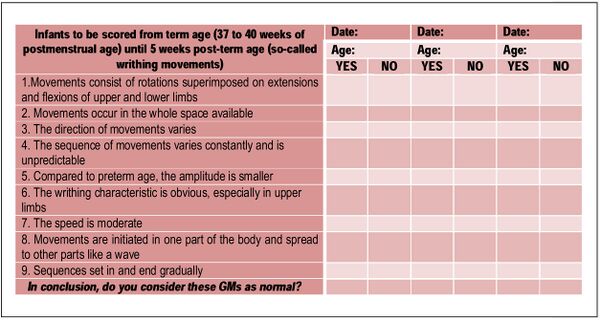
The Prechtl General Movement Assessment | [https://general-movements-trust.info/5/home The Prechtl General Movement Assessment] is a general movement tool where clinicians watch a short video of a supine infant. Quality and type of movements are scored as “normal” or “abnormal” for 26 items. Abnormal movements are further classified into one of three categories below: | ||
# Poor repertoire (sequence of movements is monotonous; different body part movements are not complex) | |||
# Cramped-synchronised (lack of smooth and fluent movement; rigid; trunk and limb muscles relax and contract simultaneously<ref name=":4">Einspieler C, Prechtl HF, Ferrari F, Cioni G, Bos AF. [https://jamanetwork.com/journals/jamapediatrics/fullarticle/191860 The qualitative assessment of general movements in preterm, term and young infants—review of the methodology.] Early human development. 1997 Nov 24;50(1):47-60.</ref> | |||
# Chaotic (no smoothness, chaotic and abrupt movements of large amplitude)<ref name=":5">Aizawa CY, Einspieler C, Genovesi FF, Ibidi SM, Hasue RH. [https://www.sciencedirect.com/science/article/pii/S0021755720302175 The general movement checklist: A guide to the assessment of general movements during preterm and term age]. Jornal de Pediatria. 2021 Aug 18;97:445-52.</ref> <ref name=":4" /><ref name=":3" /> | |||
<br> | |||
Based on scores from this test, the presence, type and severity of CP can be predicted. This tool is reliable and quick, but does require training.<ref name=":3" /> | |||
[[File:Prechtl.jpg|center|thumb|600x600px|Prechtl Exam<ref name=":5" />]] | |||
== Resources == | == Resources == | ||
# [https://www.canchild.ca/en/research-in-practice/family-centred-service CanChild Family Centred Service] | |||
# [[Gross Motor Function Classification System - Expanded and Revised (GMFCS-ER)]] | |||
# [https://www.physio-pedia.com/Early_Intervention_and_the_Importance_of_Early_Identification_of_Cerebral_Palsy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Early Intervention and the Importance of Early Identification of Cerebral Palsy] | |||
# [[Early Intervention in Cerebral Palsy]] | |||
# | # [https://www.physio-pedia.com/Cerebral_Palsy_Introduction?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Cerebral Palsy Introduction] | ||
# | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Cerebral Palsy]] | |||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Assessment and Examination]] | |||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Rehabilitation]] | |||
Latest revision as of 00:20, 2 November 2023
Early Intervention[edit | edit source]
Early intervention services are a set of interventions that support and provide resources for families of special needs infants and toddlers, aged between 0 and 3 years old.[1]
Can Child[2] definition of family centred service: "Family-centred service is made up of a set of values, attitudes, and approaches to services for children with special needs and their families. Family-centred service recognizes that each family is unique; that the family is the constant in the child's life; and that they are the experts on the child's abilities and needs. The family works with service providers to make informed decisions about the services and supports the child and family receive. In family-centred service, the strengths and needs of all family members are considered."[2]
Children with developmental disabilities are entitled to various services. An interdisciplinary early intervention team may include the following disciplines, depending on the family and child’s needs and availability of services:[2]
- physical therapy / physiotherapy
- occupational therapy
- speech therapy
- vision therapy
- nursing
- assistive technology
- special education
Evaluations and follow-up care are provided in the child's least restrictive or natural environment, typically at their home or daycare centre.[3] Traditionally, early intervention has worked off an expert model where the therapist created goals and provided follow-up care based on the impairment. Any interventions provided by the family were adjuncts to those provided by the healthcare professional. The overall care and decision making for the child was in the hands of the therapist. This model is referred to as a rehabilitation model.[4]
Family-Centred Care[edit | edit source]
Over the past decade, there has been a shift from the therapist-driven model to a family education/empowerment model. The family-centred care (FCC) model[5] provides collaboration between the therapist and family where the goals and aspirations of the family are central to the intervention.[1] The therapist works as a “coach” helping families identify needs, goals and solutions. FCC, thus, transfers decision-making from just the therapist to the family, who are empowered to create goals and plan intervention strategies.[1] When families are involved in the care and decisions of their child, the family and the child reap better outcomes.[4] Additionally, research has shown the FCC model to result in greater parent satisfaction, reduced cost of healthcare, behavioural/emotional support to a child and a faster recovery.[6]
Solution Focused Coaching[edit | edit source]
Traditionally, early intervention was problem-oriented with a focus on identifying impairments in the body. Interventions were targeted at fixing the dysfunction and decisions about care were made solely by the therapist. However, with a solution focused coaching (SFC) model, the therapist and family work together to envision possibilities and seek solutions to the family's needs and targeted goals.[7] [1] Family empowerment is a priority in FSC. In addition, a solution focused coaching model looks towards the child's strengths and abilities rather than their problems to initiate goal setting and intervention planning.[1]
Early Diagnosis and Referral[edit | edit source]
Cerebral Palsy[edit | edit source]
The most common physical disability in childhood is cerebral palsy (CP), occurring in every 1 in 500 births. CP is caused by brain injury early in development and presents with disorders in posture and movement leading to activity limitations.[8] Traditionally, a diagnosis would be concluded between 12 and 24 months of age when symptoms were evident. New research, however, reveals that signs and symptoms of CP appear and develop before 2 years of age. Using a combination of medical history, neuroimaging and standardised motor and neurological assessments for infants under 2, the risk of cerebral palsy can be now be predicted.[9] Using diagnostic-specific early assessments can lead to referral of services which will strengthen caregiver well-being, prevent secondary complications and optimise infant cognitive and motor plasticity.[10] The tools below are commonly used for infants aged under 2 to estimate the risk of a cerebral palsy diagnosis.
Hammersmith Infant Neurological Examination[edit | edit source]
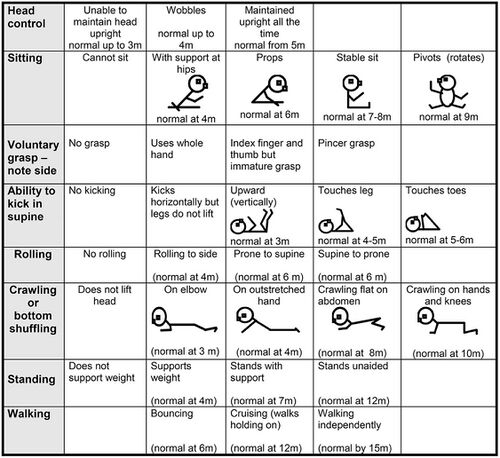
The Hammersmith Infant Neurological Examination (HINE) is a free tool with good interobserver reliability that is typically used on infants aged between 3 and 24 months. It has shown high sensitivity in detecting CP in infants, (98% in infants under 5 months old, 90% in infants over 5 months old).[9] Neurological function is tested with 26 different criteria based on movements, behaviour, cranial nerve function, protective reactions, reflexes and gross and fine motor function. Symmetry between left and right sides are also scored.[1] Test results not only identify children at risk, but detail the severity and type of motor impairment. Having this specific information allows early intervention to be targeted to the specific neurological sequelae.[8]
Scores range from 0-73. Romeo et.al[8] found that infants tested between 3 and 6 months showed the following pattern:
Scores below 40: quadriplegia (IV and V levels of GMFCS), severe diplegia (III level)
Scored 40-60: mild or moderate diplegia (I-II level); hemiplegia (I-II level)[8]
Gross Motor Function Classification System[edit | edit source]
The Gross Motor Function Classification System (GMFCS) tool classifies children aged under 2 into five distinct levels depending on their self-initiated movement. It specifically focuses on mobility, transfers and sitting. These criteria relate to functional limitations for the child versus quality of movement.[12] The GMFC is a way of classifying function severity and not a diagnostic tool.
Gross Motor Function Classification System – Expanded and Revised (GMFCS – E & R) for children aged 2 and under is as follows:[12]
- "LEVEL I: Infants move in and out of sitting and floor sit with both hands free to manipulate objects. Infants crawl on hands and knees, pull to stand and take steps holding on to furniture. Infants walk between 18 months and 2 years of age without the need for any assistive mobility device."
- LEVEL II: Infants maintain floor sitting but may need to use their hands for support to maintain balance. Infants creep on their stomach or crawl on hands and knees. Infants may pull to stand and take steps holding on to furniture.
- LEVEL III: Infants maintain floor sitting when the low back is supported. Infants roll and creep forward on their stomachs.
- LEVEL IV: Infants have head control but trunk support is required for floor sitting. Infants can roll to supine and may roll to prone.
- LEVEL V: Physical impairments limit voluntary control of movement. Infants are unable to maintain antigravity head and trunk postures in prone and sitting. Infants require adult assistance to roll."
*** Less favourable outcomes are noted in low and middle income countries with over 73% of children classified as GMFCS level of III-IV.[13]
The Prechtl General Movement Assessment[edit | edit source]
The Prechtl General Movement Assessment is a general movement tool where clinicians watch a short video of a supine infant. Quality and type of movements are scored as “normal” or “abnormal” for 26 items. Abnormal movements are further classified into one of three categories below:
- Poor repertoire (sequence of movements is monotonous; different body part movements are not complex)
- Cramped-synchronised (lack of smooth and fluent movement; rigid; trunk and limb muscles relax and contract simultaneously[14]
- Chaotic (no smoothness, chaotic and abrupt movements of large amplitude)[15] [14][1]
Based on scores from this test, the presence, type and severity of CP can be predicted. This tool is reliable and quick, but does require training.[1]
Resources[edit | edit source]
- CanChild Family Centred Service
- Gross Motor Function Classification System - Expanded and Revised (GMFCS-ER)
- Early Intervention and the Importance of Early Identification of Cerebral Palsy
- Early Intervention in Cerebral Palsy
- Cerebral Palsy Introduction
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Versfeld, P. Family-Centred Intervention and Early Diagnosis Course. Plus , 2021.
- ↑ 2.0 2.1 2.2 CanChild from McMaster University. Available at www.canchild.org
- ↑ Tomasello NM, Manning AR, Dulmus CN. Family-centered early intervention for infants and toddlers with disabilities. Journal of Family Social Work. 2010 Mar 24;13(2):163-72.
- ↑ 4.0 4.1 Dalmau M, Balcells-Balcells A, Giné C, Cañadas M, Casas O, Salat Y, Farré V, Calaf N. How to implement the family-centered model in early intervention. Anales de psicología. 2017;33(3):641-51.
- ↑ McCarthy E, Guerin S. Family‐centred care in early intervention: A systematic review of the processes and outcomes of family‐centred care and impacting factors. Child: Care, Health and Development. 2022 Jan;48(1):1-32.
- ↑ Raghupathy MK, Rao BK, Nayak SR, Spittle AJ, Parsekar SS. Effect of family-centered care interventions on motor and neurobehavior development of very preterm infants: a protocol for systematic review. Systematic reviews. 2021 Dec;10(1):1-8.
- ↑ Baldwin P, King G, Evans J, McDougall S, Tucker MA, Servais M. Solution-focused coaching in pediatric rehabilitation: an integrated model for practice. Physical & Occupational Therapy in Pediatrics. 2013 Nov 1;33(4):467-83
- ↑ 8.0 8.1 8.2 8.3 Romeo DM, Ricci D, Brogna C, Mercuri E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: a critical review of the literature. Developmental Medicine & Child Neurology. 2016 Mar;58(3):240-5.
- ↑ 9.0 9.1 Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC, De Vries LS. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA pediatrics. 2017 Sep 1;171(9):897-907.
- ↑ Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. J Novak et al (2017). AMA pediatrics, 2017 171(9), 897–907.
- ↑ De Sanctis R, Coratti G, Pasternak A, Montes J, Pane M, Mazzone ES, Young SD, Salazar R, Quigley J, Pera MC, Antonaci L. Developmental milestones in type I spinal muscular atrophy. Neuromuscular Disorders. 2016 Nov 1;26(11):754-9.
- ↑ 12.0 12.1 Palisano R, Rosenbaum P, Bartlett D, Livingston M. GMFCS – E & R Gross Motor Function Classification System Expanded and Revised. Hamilton, ON: CanChild Centre for Childhood Disability Research, McMaster University, 2007.
- ↑ Jahan I, Muhit M, Hardianto D, Laryea F, Chhetri AB, Smithers‐Sheedy H, McIntyre S, Badawi N, Khandaker G. Epidemiology of cerebral palsy in low‐and middle‐income countries: preliminary findings from an international multi‐centre cerebral palsy register. Developmental Medicine & Child Neurology. 2021 May 24.
- ↑ 14.0 14.1 Einspieler C, Prechtl HF, Ferrari F, Cioni G, Bos AF. The qualitative assessment of general movements in preterm, term and young infants—review of the methodology. Early human development. 1997 Nov 24;50(1):47-60.
- ↑ 15.0 15.1 Aizawa CY, Einspieler C, Genovesi FF, Ibidi SM, Hasue RH. The general movement checklist: A guide to the assessment of general movements during preterm and term age. Jornal de Pediatria. 2021 Aug 18;97:445-52.






