Facial Trauma: Difference between revisions
Wendy Walker (talk | contribs) No edit summary |
Wendy Walker (talk | contribs) No edit summary |
||
| Line 71: | Line 71: | ||
Surgical repair is often required for bony injury, which may involve wiring or plating, or more substantial surgical techniques to rebuild the damaged bone, such as bone grafting.<ref name=":0" /> | Surgical repair is often required for bony injury, which may involve wiring or plating, or more substantial surgical techniques to rebuild the damaged bone, such as bone grafting.<ref name=":0" /> | ||
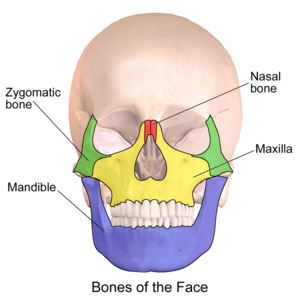
[[File:Blausen 0393 FacialBones 01.png|thumb|Illustration of bones of the face: maxilla, mandible, nasal and zygomatic.]] | |||
=== Surgical Interventions === | === Surgical Interventions === | ||
==== Maxillary Repair ==== | ==== Maxillary Repair ==== | ||
Revision as of 23:28, 27 October 2020
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (27/10/2020)
Original Editor - User: Wendy Walker
Top Contributors - Wendy Walker, Jess Bell, Tarina van der Stockt, Kim Jackson, Ewa Jaraczewska, Lucinda hampton, Wanda van Niekerk, Aminat Abolade, Nupur Smit Shah and Rishika Babburu
One Page Owner - Wendy Walker as part of the One Page Project
Introduction[edit | edit source]
Trauma to the face and head can be caused by a number of events: explosions, gunshot, road traffic accidents, falling masonry, flying glass, sports injuries, and blunt force trauma.
Soft tissue injury comprises lacerations, abrasions and avulsions.
There can be bony damage - fractures can occur in any of the bones of the head and face, but are particularly common in the mandible and nose - and also soft tissue injury. CT scanning is essential for diagnosis as this shows fractures of facial bones more reliably than plain X-ray, and also shows soft tissue injury[1]. Facial and head trauma can also cause damage to the Facial Nerve or the Trigeminal Nerve.
In addition there may be direct damage to the eye.
It is important to be aware that a number of patients who suffer trauma to the upper regions of the face also suffer from brain injury[2], and some have co-existing cervical spine injury[2].
Initial repair following serious facial trauma is performed by surgeons; fractured bones will be plated or wired, skin and soft tissue lacerations will be stitched, large areas of severe soft tissue damage may require grafting[3][3][4].
The physiotherapy rehabilitation of these patients is thus largely post operative rehabilitation.
Epidemiology[edit | edit source]
The main causes of facial trauma is road traffic accidents (RTAs), followed by falls, assaults and sports injuries[5]. Many studies from different countries show that world-wide the prevalence of facial trauma is considerably higher in men than women[6][7][8], It is clear that the causes of maxillofacial injuries vary from one country to another, and even within the same country as a result of environmental, socioeconomic and cultural factors[9].
Developing Countries[edit | edit source]
In developing countries which have a high usage of motorised vehicles, RTAs account for up to 93% of facial injuries[6], with a high proportion of these involving motorcycles. One study reports that as many as 50 to 70% of RTA survivors suffer from facial trauma. In countries where motorcycles are a major form of transport, such as Malaysia, RTAs involving motorcycles biggest single cause of facial trauma[10].
Developed Countries[edit | edit source]
One large study in Austria[7] found that the causes of maxillofacial injury were: in 38% of cases, an activity of daily life, in 31% sports, in 12% violence, 12% RTA, 5% work accidents, 2% other causes.
Initial Stages[edit | edit source]
The face has a very rich blood supply, so healing is usually rapid.
Soft Tissue Injury[edit | edit source]
In areas of thin skin (eg. the eyelids) sutures can normally be removed after just 3-4 days, and elsewhere on the face they are often removed after 6 days[11]. Sutures in cartilage, for example the ear or the nose, are often left in situ for 10-14 days.
Bony Injury[edit | edit source]
For more information on the bones of the face, see the Facial Skeleton page.
Surgical repair is often required for bony injury, which may involve wiring or plating, or more substantial surgical techniques to rebuild the damaged bone, such as bone grafting.[2]
Surgical Interventions[edit | edit source]
Maxillary Repair[edit | edit source]
The maxilla bone forms the upper jaw, and houses the upper teeth. It forms the hard palate, as well as the floor of the eye socket. Fractures of the maxilla may require surgical intervention, plating or wiring.
Mandibular Repair[edit | edit source]
The mandible, AKA jaw bone, is frequently injured in facial trauma.
In some cases, Mandibular Maxilla Fixation, MMF, may be required - this involves wiring the jaws closed while the bony healing occurs.
Later Stages[edit | edit source]
Once the surgical repair techniques have been completed, the body continues the healing, producing scar tissue.
The proliferation phase (AKA fibroblastic phase) of scar tissue lasts for 2-3 weeks, and it is in this phase that the majority of the scar tissue, collagen, is laid down; after this time there is a slowing of proliferation for the next 4-6 months.
This is followed by the remodelling (AKA maturation) phase, when the scar tissue continues to rebuild and remodel, becoming more organised and functional, and more similar to the tissue it is repairing. This process continues for up to a year.
Please see the Soft Tissue Healing page for more details on scar tissue formation.
Physiotherapy following Facial Trauma[edit | edit source]
Rehabilitation should begin as soon as the surgeons permit it.
The aim of physiotherapy is to restore as much facial range of movement as possible, which will result in restoration of facial function.
Clinical Presentation[edit | edit source]
Any of the following may occur, often several in combination:
- Reduced facial range of movement
- Inability or reduced ability to close the eye
- Inability or reduced ability to move the lips eg. into a smile, pucker
- Inability to bite or chew
- Asymmetry of the facial structures
- Difficulties keeping food in the mouth when eating
- Difficulties forming a lip seal on a vessel when drinking
- Dry eye
- Dry mouth
- Reduction in non-verbal communication through facial expression
Rehabilitation[edit | edit source]
Manual Techniques[edit | edit source]
Manual techniques to the soft tissues are frequently utilised, with the aim of restoring the flexibility of the soft tissues. The nature of scar tissue means that as it heals there is a tendency for loss of both elasticity and length, and this can result in reduced range of movement.
Gentle passive stretching techniques can be used to lengthen the tissues.
Injury to the eye and the surrounding area can be problematic: if the eyelid is injured, as it heals and shortens, it may result in insufficient passive length resulting in incomplete eye closure. This in turn means that the eye itself. is at risk of being damaged. The tissues of the eyelid are extremely thin, and with careful, gentle stretching techniques the length can be restored.
Active Exercises[edit | edit source]
Once tissue length is established, the patient should be encouraged to move the affected area of the face actively through the newly gained range.
Electrotherapy[edit | edit source]
While several electrotherapeutic techniques are known to improve soft tissue healing, the face is such a vascular area that in the majority of cases these are not required as the tissue spontaneously heals swiftly and well.
Temporomandibular Joint [TMJ] Rehabilitation[edit | edit source]
- Active exercises to increase TMJ range of movement. These should include all TMJ movements: depression of the mandible = mouth opening; elevation of the mandible = mouth closing; lateral movement of the mandible - these actions are used in chewing; protraction of the mandible.
- There are 4 muscles of mastication which act on the TMJ: Masseter, Temporalis, Lateral Pterygoid and Medial Pterygoid.
- Of the 4 muscles which act on the TMJ, the masseter is the strongest, its action being to close the mouth. If the temporomandibular joint and/or the masseter is injured, the patient will initially have marked weakness of the chewing action.
- There is only one muscle which produces opening of the mouth/mandible depression: Lateral Pterygoid. Injuries to this muscle produce difficulty in closing the mouth.
Rehabilitation for Facial Lacerations[edit | edit source]
Nerve Injury Rehabilitation - Trigeminal Nerve[edit | edit source]
Nerve Injury Rehabilitation - Facial Nerve[edit | edit source]
Trauma to the cheek region can easily result in damage to the facial nerve[12]. Surgical exploration is required to evaluate the condition of the nerve: if it is completely transected, surgical repair or even nerve graft will be performed, and the recovery of active movement will be delayed as the axons grow through the repaired nerve at a rate of approx 1mm per day.
There are a series of pages on this topic; the main one to consult is the Facial Palsy page.
References[edit | edit source]
- ↑ Jordan JR, Calhoun KH (2006). "Management of soft tissue trauma and auricular trauma". In Bailey BJ, Johnson JT, Newlands SD, et al. (eds.). Head & Neck Surgery: Otolaryngology. Hagerstwon, MD: Lippincott Williams & Wilkins. pp. 935–36.
- ↑ 2.0 2.1 2.2 Perry M (March 2008). "Advanced Trauma Life Support (ATLS) and facial trauma: can one size fit all? Part 1: dilemmas in the management of the multiply injured patient with coexisting facial injuries". International Journal of Oral and Maxillofacial Surgery. 37 (3): 209–14
- ↑ 3.0 3.1 Aveta A, Casati P. Soft tissue injuries of the face: early aesthetic reconstruction in polytrauma patients. Ann Ital Chir. 2008;79:415–417
- ↑ James D. Kretlow, Aisha J. McKnight, Shayan A. Izaddoost. "Facial Soft Tissue Trauma" Semin Plast Surg. 2010 Nov; 24(4): 348–356
- ↑ Wood E, Freer T. Incidence and Aetiology of Facial Injuries Resulting from Motor Vehicle Accidents in Queensland for a Three‐year Period. Aus Dental J. 2001;46:284–8
- ↑ 6.0 6.1 Mohanavalli Singaram, Sree Vijayabala G, Rajesh Kumar Udhayakumar. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. J Korean Assoc Oral Maxillofac Surg. 2016 Aug; 42(4): 174–181.
- ↑ 7.0 7.1 Robert Gassner 1, Tarkan Tuli, Oliver Hächl, Ansgar Rudisch, Hanno Ulmer. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. . 2003 Feb;31(1):51-61.
- ↑ Schneider D, Kämmerer PW, Schon G, Dinu C, Radloff S, Bschorer R (2015) Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: a retrospective study of 409 patients. J Craniomaxillofac Surg 43:1948–1951.
- ↑ Einy S, Abdel Rahman N, Siman-Tov M, Aizenbud D, Peleg K (2016) Maxillofacial trauma following road accidents and falls. J Craniofac Surg 27:857–861.
- ↑ Maher M. Abosadegh, Norkhafizah Saddki, Badr Al-Tayar, and Shaifulizan Ab. Rahman. Epidemiology of Maxillofacial Fractures at a Teaching Hospital in Malaysia: A Retrospective Study BioMed Research International / 2019 / Research Article | Open Access Volume 2019 |Article ID 9024763
- ↑ Ardeshirpour F, Shaye DA, Hilger PA. Improving posttraumatic facial scars. Otolaryngol Clin North Am. 2013 Oct. 46(5):867-8
- ↑ V. Bhattacharya Management of soft tissue wounds of the face Indian J Plast Surg. 2012 Sep-Dec; 45(3): 436–443.