Facial Trauma: Difference between revisions
(added recent references) |
No edit summary |
||
| (11 intermediate revisions by 5 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Trauma to the face and head can be caused by a number of events: explosions, gunshot, road traffic accidents, falling masonry, flying glass, sports injuries, and blunt force trauma. Soft tissue injury comprises lacerations, abrasions and avulsions. | [[Trauma-Informed Care|Trauma]] to the face and head can be caused by a number of events: explosions, gunshot, road traffic accidents (RTAs), falling masonry, flying glass, sports injuries, and blunt force trauma. Soft tissue injury comprises lacerations, abrasions and avulsions. | ||
There can be: | There can be: | ||
* Bony damage - [[Fracture|fractures]] can occur in any of the [[Skull|bones of the head and face]], but are particularly common in the mandible and nose - and also [[Soft Tissue Injuries|soft tissue injury]]. [[CT Scans|CT scanning]] is essential for diagnosis as this shows fractures of facial bones more reliably than plain [[X-Rays|X-ray]], and also shows soft tissue injury<ref>Jordan JR, Calhoun KH | * Bony damage - [[Fracture|fractures]] can occur in any of the [[Skull|bones of the head and face]], but are particularly common in the mandible and nose - and also [[Soft Tissue Injuries|soft tissue injury]]. [[CT Scans|CT scanning]] is essential for diagnosis as this shows fractures of facial bones more reliably than plain [[X-Rays|X-ray]], and also shows soft tissue injury<ref>Jordan JR, Calhoun KH. [https://books.google.com/books?id=u5o3illp9CUC&pg=RA1-PA935&dq=facial+trauma Management of soft tissue trauma and auricular trauma]. In Bailey BJ, Johnson JT, Newlands SD, et al. editors. Head & Neck Surgery: Otolaryngology. Hagerstwon, MD: Lippincott Williams & Wilkins.2006. p. 935–36.</ref>. | ||
* [[Facial Nerve]] or the [[Trigeminal Nerve]] | * [[Facial Nerve]] or the [[Trigeminal Nerve]] damage may occur with facial and head trauma. | ||
* Direct damage to the eye. | * Direct damage to the eye. | ||
* It is important to be aware that a number of patients who suffer trauma to the face also suffer from [[Overview of Traumatic Brain Injury|brain injury]]<ref name=":0">Perry M | * It is important to be aware that a number of patients who suffer trauma to the face also suffer from [[Overview of Traumatic Brain Injury|brain injury]]<ref name=":0">Perry M. Advanced Trauma Life Support (ATLS) and facial trauma: can one size fit all? Part 1: dilemmas in the management of the multiply injured patient with coexisting facial injuries. Int J Oral Maxillofac Surg. 2008 Mar;37(3):209-14.</ref>, and some have co-existing [[Spinal Cord Injury|cervical spine injury]]<ref name=":0" />[[Spinal Cord Injury|.]] | ||
Initial repair following serious facial trauma is performed by surgeons: fractured bones will be plated or wired; [[skin]] and soft tissue lacerations will be stitched; large areas of severe soft tissue damage may require grafting<ref name=":1">Aveta A, Casati P. | Initial repair following serious facial trauma is performed by surgeons: fractured bones will be plated or wired; [[skin]] and soft tissue lacerations will be stitched; large areas of severe soft tissue damage may require grafting<ref name=":1">Aveta A, Casati P. Soft tissue injuries of the face: early aesthetic reconstruction in polytrauma patients. Ann Ital Chir. 2008 Nov-Dec;79(6):415-7. | ||
Soft tissue injuries of the face: early aesthetic reconstruction in polytrauma patients. | </ref><ref>Kretlow JD, McKnight AJ, Izaddoost SA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3324223/pdf/sps24348.pdf Facial soft tissue trauma]. Semin Plast Surg. 2010 Nov;24(4):348-56. | ||
Ann Ital Chir. | |||
</ref | |||
Semin Plast Surg. 2010 Nov; 24(4): | |||
</ref>. | </ref>. | ||
| Line 25: | Line 19: | ||
== Epidemiology == | == Epidemiology == | ||
The main causes of facial trauma are road traffic accidents | The main causes of facial trauma are road traffic accidents, [[falls]], assaults and [[Sport Injury Classification|sports injuries]].<ref name=":5">Wusiman P, Maimaitituerxun B, Saimaiti A, Moming A. Epidemiology and pattern of oral and maxillofacial trauma. Journal of Craniofacial Surgery. 2020 Jul 1;31(5):e517-20.</ref><ref>Wood EB, Freer TJ. I[https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1834-7819.2001.tb00293.x ncidence and aetiology of facial injuries resulting from motor vehicle accidents in Queensland for a three-year period]. Aust Dent J. 2001 Dec;46(4):284-8. | ||
</ref><ref>Lalloo R, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT et al. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020; 26(Supp 1): i27-i35. </ref> Many studies from different countries show that world-wide the prevalence of facial trauma is considerably higher in men than women<ref name=":2" /><ref name=":3" /><ref>Schneider D, Kämmerer PW, Schön G, Dinu C, Radloff S, Bschorer R. Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: A retrospective study of 409 patients. J Craniomaxillofac Surg. 2015 Dec;43(10):1948-51. | |||
</ref>, It is clear that the causes of maxillofacial injuries vary from one country to another, and even within the same country as a result of environmental, socioeconomic and cultural factors<ref>Einy S, Abdel Rahman N, Siman-Tov M, Aizenbud D, Peleg K. Maxillofacial Trauma Following Road Accidents and Falls. J Craniofac Surg. 2016 Jun;27(4):857-61. | |||
</ref><ref>Lalloo R, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT et al. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020; 26(Supp 1): i27-i35. </ref> Many studies from different countries show that world-wide the prevalence of facial trauma is considerably higher in men than women | |||
Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: | |||
J Craniomaxillofac Surg 43: | |||
</ref>, It is clear that the causes of maxillofacial injuries vary from one country to another, and even within the same country as a result of environmental, socioeconomic and cultural factors<ref>Einy S, Abdel Rahman N, Siman-Tov M, Aizenbud D, Peleg K | |||
Maxillofacial | |||
J Craniofac Surg 27: | |||
</ref>. | </ref>. | ||
| Line 40: | Line 28: | ||
Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. | Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. | ||
J Korean Assoc Oral Maxillofac Surg. 2016 Aug; 42(4): 174–181. | J Korean Assoc Oral Maxillofac Surg. 2016 Aug; 42(4): 174–181. | ||
</ref>, with a high proportion of these involving motorcycles. One study reports that as many as 50 to 70% of RTA survivors suffer from facial trauma. In countries where motorcycles are a major form of transport, such as Malaysia, RTAs involving motorcycles, are the biggest single cause of facial trauma<ref> | </ref>, with a high proportion of these involving motorcycles. One study reports that as many as 50 to 70% of RTA survivors suffer from facial trauma. In countries where motorcycles are a major form of transport, such as Malaysia, RTAs involving motorcycles, are the biggest single cause of facial trauma<ref>Abosadegh MM, Saddki N, Al-Tayar B, Rahman SA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6393910/pdf/BMRI2019-9024763.pdf Epidemiology of Maxillofacial Fractures at a Teaching Hospital in Malaysia: A Retrospective Study]. Biomed Res Int. 2019 Feb 13;2019:9024763. | ||
</ref>. | </ref>. | ||
==== Developed Countries ==== | ==== Developed Countries ==== | ||
One large study in Austria<ref name=":3"> | One large study in Austria<ref name=":3">Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003 Feb;31(1):51-61. | ||
Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. | </ref> found that the causes of maxillofacial injury were: in 38% of cases, an [[Activities of Daily Living|activity of daily life]], in 31% sports, in 12% violence, 12% RTA, 5% [[Work-Related Musculoskeletal Injuries and Prevention|work accident]]<nowiki/>s, 2% other causes. | ||
. | |||
</ref> found that the causes of maxillofacial injury were: in 38% of cases, an [[ | |||
== Initial Stages == | == Initial Stages == | ||
| Line 53: | Line 39: | ||
=== Soft Tissue Injury === | === Soft Tissue Injury === | ||
In areas of thin skin (eg. the eyelids) sutures can normally be removed after just 3-4 days, and elsewhere on the face, they are often removed after 6 days<ref>Ardeshirpour F, Shaye DA, Hilger PA. | In areas of thin [[skin]] (eg. the eyelids) sutures can normally be removed after just 3-4 days, and elsewhere on the face, they are often removed after 6 days<ref>Ardeshirpour F, Shaye DA, Hilger PA. Improving posttraumatic facial scars. Otolaryngol Clin North Am. 2013 Oct;46(5):867-81. | ||
Improving posttraumatic facial scars. | |||
</ref>. Sutures in [[cartilage]], for example, the ear or the nose, are often left in situ for 10-14 days. | </ref>. Sutures in [[cartilage]], for example, the ear or the nose, are often left in situ for 10-14 days. | ||
| Line 71: | Line 56: | ||
==== Mandibular Repair ==== | ==== Mandibular Repair ==== | ||
The mandible, AKA jaw bone, is frequently injured in facial trauma. It is the only moving bone in the face, and it houses the lower teeth. | The [[mandible]], AKA jaw bone, is frequently injured in facial trauma. It is the only moving bone in the face, and it houses the lower teeth. | ||
In some cases, Mandibular Maxilla Fixation, MMF, may be required - this involves wiring the jaws closed while the bony healing occurs. | In some cases, Mandibular Maxilla Fixation, MMF, may be required - this involves wiring the jaws closed while the bony healing occurs. | ||
| Line 77: | Line 62: | ||
== Later Stages == | == Later Stages == | ||
Once the surgical repair techniques have been completed, the body continues the [[Wound Healing|healing]], producing scar tissue. | Once the surgical repair techniques have been completed, the body continues the [[Wound Healing|healing]], producing scar tissue. | ||
* The proliferation phase (AKA fibroblastic phase) of scar tissue lasts for 2-3 weeks, and it is in this phase that the majority of the scar tissue, collagen, is laid down; after this time there is a slowing of proliferation for the next 4-6 months. | * The [[Soft Tissue Healing|proliferation phase]] (AKA fibroblastic phase) of scar tissue lasts for 2-3 weeks, and it is in this phase that the majority of the scar tissue, collagen, is laid down; after this time there is a slowing of proliferation for the next 4-6 months. | ||
* This is followed by the remodelling (AKA maturation) phase, when the scar tissue continues to rebuild and remodel, becoming more organised and functional, and more similar to the tissue it is repairing. This process continues for up to a year. | * This is followed by the remodelling (AKA maturation) phase, when the scar tissue continues to rebuild and remodel, becoming more organised and functional, and more similar to the tissue it is repairing. This process continues for up to a year. | ||
Please see the [[Soft Tissue Healing]] page for more details on scar tissue formation. | Please see the [[Soft Tissue Healing]] page for more details on scar tissue formation. | ||
| Line 90: | Line 75: | ||
{{#ev:youtube|EUVD8cwKfFQ}}<ref>Neural Academy. Muscles of Facial Expression and Mastication. Available from: https://www.youtube.com/watch?v=EUVD8cwKfFQ [last accessed 10/11/2020]</ref> | {{#ev:youtube|EUVD8cwKfFQ}}<ref>Neural Academy. Muscles of Facial Expression and Mastication. Available from: https://www.youtube.com/watch?v=EUVD8cwKfFQ [last accessed 10/11/2020]</ref> | ||
== Physiotherapy | == Physiotherapy Following Facial Trauma == | ||
Rehabilitation should begin as soon as the surgeons permit it. | Rehabilitation should begin as soon as the surgeons permit it. | ||
| Line 113: | Line 98: | ||
Manual techniques to the soft tissues are frequently utilised, with the aim of restoring the flexibility of the soft tissues. The nature of scar tissue means that as it heals there is a tendency for loss of both elasticity and length, and this can result in a reduced range of movement. | Manual techniques to the soft tissues are frequently utilised, with the aim of restoring the flexibility of the soft tissues. The nature of scar tissue means that as it heals there is a tendency for loss of both elasticity and length, and this can result in a reduced range of movement. | ||
Gentle passive stretching techniques can be used to lengthen the tissues. | Gentle [[Stretching|passive stretching]] techniques can be used to lengthen the tissues. | ||
Injury to the eye and the surrounding area can be problematic: if the eyelid is injured, as it heals and shortens, it may result in insufficient passive length resulting in incomplete eye closure. This in turn means that the eye itself is at risk of being damaged. The tissues of the eyelid are extremely thin, and with careful, gentle stretching techniques the length can be restored. | Injury to the eye and the surrounding area can be problematic: if the eyelid is injured, as it heals and shortens, it may result in insufficient passive length resulting in incomplete eye closure. This in turn means that the eye itself is at risk of being damaged. The tissues of the eyelid are extremely thin, and with careful, gentle stretching techniques the length can be restored. | ||
| Line 121: | Line 106: | ||
===== Electrotherapy ===== | ===== Electrotherapy ===== | ||
While several electrotherapeutic techniques are known to improve soft tissue healing, the face is such a vascular area that in the majority of cases these are not required as the tissue spontaneously heals swiftly and well. | While several [[Electrotherapy Contraindications|electrotherapeutic techniques]] are known to improve soft tissue healing, the face is such a vascular area that in the majority of cases these are not required as the tissue spontaneously heals swiftly and well. | ||
===== [[TMJ Anatomy|Temporomandibular Joint]] [TMJ] Rehabilitation ===== | ===== [[TMJ Anatomy|Temporomandibular Joint]] [TMJ] Rehabilitation ===== | ||
* Active and passive joint movements are considered to be an important part of post-operative exercise rehabilitation<ref> | * Active and passive joint movements are considered to be an important part of post-operative exercise rehabilitation and long term follow up is recommended<ref>Stelea CG, Agop-Forna D, Dragomir R, Ancuţa C, Törok R, Forna NC, Iordache C. [https://www.mdpi.com/2076-3417/11/21/10239/htm Recovery of Post-Traumatic Temporomandibular Joint after Mandibular Fracture Immobilization: A Literature Review]. Applied Sciences. 2021 Nov 1;11(21):10239.</ref> | ||
* Active exercises to increase TMJ range of movement. These should include all TMJ movements: depression of the mandible = mouth opening | * Active exercises to increase TMJ range of movement. These should include all TMJ movements: | ||
* There are 4 [[Muscles of Mastication|muscles of mastication]] which act on the TMJ: Masseter, Temporalis, Lateral Pterygoid and Medial Pterygoid<ref name=":4" /> | ** depression of the mandible = mouth opening | ||
** elevation of the mandible = mouth closing | |||
** lateral movement of the mandible - these actions are used in chewing | |||
** protraction of the mandible | |||
* There are 4 [[Muscles of Mastication|muscles of mastication]] which act on the TMJ: | |||
* Masseter, Temporalis, Lateral Pterygoid and Medial Pterygoid<ref name=":4" /> | |||
* Of the 4 muscles which act on the TMJ, the masseter is the strongest, its action is to close the mouth. If the temporomandibular joint and/or the masseter is injured, the patient will initially have marked weakness of the chewing action. | * Of the 4 muscles which act on the TMJ, the masseter is the strongest, its action is to close the mouth. If the temporomandibular joint and/or the masseter is injured, the patient will initially have marked weakness of the chewing action. | ||
* There is only one muscle which produces opening of the mouth/mandible depression: Lateral Pterygoid. Injuries to this muscle produce difficulty and weakness in closing the mouth | * There is only one muscle which produces opening of the mouth/mandible depression: Lateral Pterygoid. Injuries to this muscle produce difficulty and weakness in closing the mouth | ||
| Line 133: | Line 123: | ||
{{#ev:youtube|SCS4MiHJ5Xw}}<ref>Functional Anatomy TMJ. Movements of the TMJ. Available from https://www.youtube.com/watch?v=SCS4MiHJ5Xw&feature=emb_logo [last accessed 4/11/2020]</ref> | {{#ev:youtube|SCS4MiHJ5Xw}}<ref>Functional Anatomy TMJ. Movements of the TMJ. Available from https://www.youtube.com/watch?v=SCS4MiHJ5Xw&feature=emb_logo [last accessed 4/11/2020]</ref> | ||
===== Rehabilitation for | ===== Rehabilitation for Injured Facial Muscles ===== | ||
Injury to the [[Facial Muscles - Upper Group|muscles of the upper face]] can result in difficulties closing the eye; protection of the eye is of paramount importance. The sphincter muscle of which closes the eye is called orbicularis oculi, so if this muscle is damaged they eye may remain open and be unable to close. | Injury to the [[Facial Muscles - Upper Group|muscles of the upper face]] can result in difficulties closing the eye; protection of the eye is of paramount importance. The sphincter muscle of which closes the eye is called orbicularis oculi, so if this muscle is damaged they eye may remain open and be unable to close. | ||
| Line 139: | Line 129: | ||
===== Nerve Injury Rehabilitation - [[Trigeminal Nerve]] ===== | ===== Nerve Injury Rehabilitation - [[Trigeminal Nerve]] ===== | ||
Damage to the Trigeminal Nerve results in loss of sensation to the skin of the face. Of the three branches of the Trigeminal Nerve, the 3rd branch, V3 known as the Mandibular nerve, is the only one which carries motor fibres; the other two branches, V1 | Damage to the [[Trigeminal Nerve]] results in loss of [[sensation]] to the skin of the face. Of the three branches of the Trigeminal Nerve, the 3rd branch, V3 known as the Mandibular nerve, is the only one which carries motor fibres; the other two branches, V1 Ophthalmic Nerve and V2 Ophthalmic Nerve, carry only sensory fibres. Thus if the Mandibular nerve is damaged, the power of the chewing function is affected. | ||
Active exercises, and in some cases even Trophic Electrical Stimulation, will be required to restore function and improve ease of eating. | Active exercises, and in some cases even Trophic [[Electrical Stimulation - Its role in upper limb recovery post-stroke|Electrical Stimulation]], will be required to restore function and improve ease of eating. | ||
===== Nerve Injury Rehabilitation - [[Facial Nerve]] ===== | ===== Nerve Injury Rehabilitation - [[Facial Nerve]] ===== | ||
| Line 147: | Line 137: | ||
Management of soft tissue wounds of the face | Management of soft tissue wounds of the face | ||
Indian J Plast Surg. 2012 Sep-Dec; 45(3): 436–443. | Indian J Plast Surg. 2012 Sep-Dec; 45(3): 436–443. | ||
</ref>. Surgical exploration is required to evaluate the condition of the nerve: if it is completely transected, surgical repair or even nerve graft will be performed, and the recovery of active movement will be delayed as the axons grow through the repaired nerve at a rate of | </ref>. Surgical exploration is required to evaluate the condition of the nerve: if it is completely transected, surgical repair or even nerve graft will be performed, and the recovery of active movement will be delayed as the axons grow through the repaired nerve at a rate of approximately 1mm per day.<ref>Martins RS, Bastos D, Siqueira MG, Heise CO, Teixeira MJ. Traumatic injuries of peripheral nerves: a review with emphasis on surgical indication. Arq. Neuro-Psiquiatr. 2013; 71( 10 ): 811-814. </ref> | ||
There are a series of pages on this topic; the main one to consult is the [[Facial Palsy]] page. | There are a series of pages on this topic; the main one to consult is the [[Facial Palsy]] page. | ||
Very often, if the facial nerve is damaged, the orbicularis oculi muscle is unable to contract, which results in the patient being unable to close the eye,<ref name=":4" /> and the eye will not produce tears as this function is also supplied by the facial nerve.<ref> | Very often, if the facial nerve is damaged, the orbicularis oculi muscle is unable to contract, which results in the patient being unable to close the eye,<ref name=":4" /> and the eye will not produce tears as this function is also supplied by the facial nerve.<ref>Ho J, Markowsky A. [https://reader.elsevier.com/reader/sd/pii/S1555415521004748?token=28C68F1D5A3647FC9A14FCBDB3B960B050936A12E811C68FA95F48C4C5961EB5F9C9C7F372FEA5FBA39080CB11F14152&originRegion=eu-west-1&originCreation=20221019195451 Diagnosis and Management of Bell’s Palsy in Primary Care]. The Journal for Nurse Practitioners 2022; 18(2):159-163.</ref> The person will need to be taught appropriate eye care (see the [[Dry Eye]] page for more detail) including use of artificial lubrication products and how to tape the eye closed at night. | ||
{{#ev:youtube|VuuXqdbhQ6g}}<ref>FacialPalsyUK. Introduction to Paresis. Available from: https://www.youtube.com/watch?v=VuuXqdbhQ6g [last accessed 10/11/2020]</ref> | {{#ev:youtube|VuuXqdbhQ6g}}<ref>FacialPalsyUK. Introduction to Paresis. Available from: https://www.youtube.com/watch?v=VuuXqdbhQ6g [last accessed 10/11/2020]</ref> | ||
== Psychological Effects of Facial Trauma Injury == | == Psychological Effects of Facial Trauma Injury == | ||
The disfigurement caused by facial injuries can lead to psychological difficulties, ranging from [[depression]], anxiety, a tendency to become socially isolated and in some cases increased hostility<ref>Bisson JI, Shepherd JP, Dhutia M | The disfigurement caused by facial injuries can lead to psychological difficulties, ranging from [[depression]], anxiety, a tendency to become socially isolated and in some cases increased hostility<ref>Bisson JI, Shepherd JP, Dhutia M. Psychological sequelae of facial trauma. J Trauma. 1997 Sep;43(3):496-500. | ||
</ref>. A number of patients report they experience social stigma<ref>Newell R, Marks I. [https://www.cambridge.org/core/services/aop-cambridge-core/content/view/9FC8C70BC1DC6D57AE2FDA5886544A7B/S0007125000264155a.pdf/phobic-nature-of-social-difficulty-in-facially-disfigured-people.pdf Phobic nature of social difficulty in facially disfigured people]. Br J Psychiatry. 2000 Feb;176:177-81. | |||
Psychological sequelae of facial trauma. | |||
J Trauma. 1997 Sep; 43(3):496-500. | |||
</ref>. A number of patients report they experience social stigma<ref>Newell R, Marks I | |||
Phobic nature of social difficulty in facially disfigured people. | |||
Br J Psychiatry. 2000 Feb; 176 | |||
</ref>. | </ref>. | ||
[[Post-traumatic Stress Disorder|Post-traumatic stress | [[Post-traumatic Stress Disorder|Post-traumatic stress disorder]]<nowiki/> PTSD, can occur following facial trauma. One study found that 23% of patients continued to suffer from PTSD one year after the incident<ref>Glynn SM, Shetty V, Elliot-Brown K, Leathers R, Belin TR, Wang J. Chronic posttraumatic stress disorder after facial injury: a 1-year prospective cohort study. J Trauma. 2007 Feb;62(2):410-8; discussion 418. | ||
Chronic posttraumatic stress disorder after facial injury: a 1-year prospective cohort study. | |||
. | |||
</ref>. | </ref>. | ||
| Line 174: | Line 157: | ||
<references /><br> | <references /><br> | ||
[[Category:Facial_Palsy]] | [[Category:Facial_Palsy]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
Latest revision as of 18:55, 17 January 2023
Original Editor - User: Wendy Walker
Top Contributors - Wendy Walker, Jess Bell, Tarina van der Stockt, Kim Jackson, Ewa Jaraczewska, Lucinda hampton, Wanda van Niekerk, Aminat Abolade, Nupur Smit Shah and Rishika Babburu
Introduction[edit | edit source]
Trauma to the face and head can be caused by a number of events: explosions, gunshot, road traffic accidents (RTAs), falling masonry, flying glass, sports injuries, and blunt force trauma. Soft tissue injury comprises lacerations, abrasions and avulsions.
There can be:
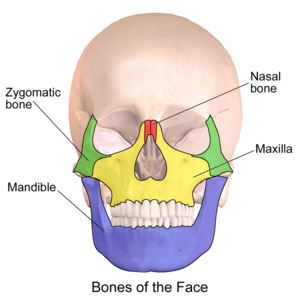
- Bony damage - fractures can occur in any of the bones of the head and face, but are particularly common in the mandible and nose - and also soft tissue injury. CT scanning is essential for diagnosis as this shows fractures of facial bones more reliably than plain X-ray, and also shows soft tissue injury[1].
- Facial Nerve or the Trigeminal Nerve damage may occur with facial and head trauma.
- Direct damage to the eye.
- It is important to be aware that a number of patients who suffer trauma to the face also suffer from brain injury[2], and some have co-existing cervical spine injury[2].
Initial repair following serious facial trauma is performed by surgeons: fractured bones will be plated or wired; skin and soft tissue lacerations will be stitched; large areas of severe soft tissue damage may require grafting[3][4].
The physiotherapy rehabilitation of these patients is thus largely post-operative rehabilitation.
Epidemiology[edit | edit source]
The main causes of facial trauma are road traffic accidents, falls, assaults and sports injuries.[5][6][7] Many studies from different countries show that world-wide the prevalence of facial trauma is considerably higher in men than women[8][9][10], It is clear that the causes of maxillofacial injuries vary from one country to another, and even within the same country as a result of environmental, socioeconomic and cultural factors[11].
Developing Countries[edit | edit source]
In developing countries which have a high usage of motorised vehicles, RTAs account for up to 93% of facial injuries[8], with a high proportion of these involving motorcycles. One study reports that as many as 50 to 70% of RTA survivors suffer from facial trauma. In countries where motorcycles are a major form of transport, such as Malaysia, RTAs involving motorcycles, are the biggest single cause of facial trauma[12].
Developed Countries[edit | edit source]
One large study in Austria[9] found that the causes of maxillofacial injury were: in 38% of cases, an activity of daily life, in 31% sports, in 12% violence, 12% RTA, 5% work accidents, 2% other causes.
Initial Stages[edit | edit source]
The face has a very rich blood supply, so healing is usually rapid.
Soft Tissue Injury[edit | edit source]
In areas of thin skin (eg. the eyelids) sutures can normally be removed after just 3-4 days, and elsewhere on the face, they are often removed after 6 days[13]. Sutures in cartilage, for example, the ear or the nose, are often left in situ for 10-14 days.
Lacerations are frequently treated with sutures, but if large areas of skin and muscle have been severely damaged, skin graft surgery will be required.
Bony Injury[edit | edit source]
For more information on the bones of the face, see the Facial Skeleton page.
Surgical repair is often required for a bony injury, which may involve wiring or plating, or more substantial surgical techniques to rebuild the damaged bone, such as bone grafting.[2]
Surgical Interventions[edit | edit source]
Maxillary Repair[edit | edit source]
The maxilla bone forms the upper jaw and houses the upper teeth. It forms the hard palate, as well as the floor of the eye socket. Fractures of the maxilla may require surgical intervention, plating or wiring.
Mandibular Repair[edit | edit source]
The mandible, AKA jaw bone, is frequently injured in facial trauma. It is the only moving bone in the face, and it houses the lower teeth.
In some cases, Mandibular Maxilla Fixation, MMF, may be required - this involves wiring the jaws closed while the bony healing occurs.
Later Stages[edit | edit source]
Once the surgical repair techniques have been completed, the body continues the healing, producing scar tissue.
- The proliferation phase (AKA fibroblastic phase) of scar tissue lasts for 2-3 weeks, and it is in this phase that the majority of the scar tissue, collagen, is laid down; after this time there is a slowing of proliferation for the next 4-6 months.
- This is followed by the remodelling (AKA maturation) phase, when the scar tissue continues to rebuild and remodel, becoming more organised and functional, and more similar to the tissue it is repairing. This process continues for up to a year.
Please see the Soft Tissue Healing page for more details on scar tissue formation.
Characteristics of Facial Muscles[edit | edit source]
The facial muscles have different characteristics compared to muscles in the trunk and limbs:
- They have a more complex pattern of innervation of extrafusal fibres[14]
- They have a larger percentage of slow-type nerve fibres[14]
- Many facial muscles insert not into bone or fascia, but into the skin
- Many facial muscles are very thin in structure and are poorly differentiated, merging with other facial muscles
Physiotherapy Following Facial Trauma[edit | edit source]
Rehabilitation should begin as soon as the surgeons permit it.
The aim of physiotherapy is to restore as much facial range of movement as possible, which will result in the restoration of facial function.
Clinical Presentation[edit | edit source]
Any of the following may occur, often several in combination:
- Reduced facial range of movement
- Inability or reduced ability to close the eye
- Inability or reduced ability to move the lips eg. into a smile, pucker
- Inability to bite or chew
- Asymmetry of the facial structures
- Difficulties keeping food in the mouth when eating
- Difficulties forming a lip seal on a vessel when drinking
- Dry eye
- Dry mouth
- Reduction in non-verbal communication through facial expression
Rehabilitation[edit | edit source]
Manual Techniques[edit | edit source]
Manual techniques to the soft tissues are frequently utilised, with the aim of restoring the flexibility of the soft tissues. The nature of scar tissue means that as it heals there is a tendency for loss of both elasticity and length, and this can result in a reduced range of movement.
Gentle passive stretching techniques can be used to lengthen the tissues.
Injury to the eye and the surrounding area can be problematic: if the eyelid is injured, as it heals and shortens, it may result in insufficient passive length resulting in incomplete eye closure. This in turn means that the eye itself is at risk of being damaged. The tissues of the eyelid are extremely thin, and with careful, gentle stretching techniques the length can be restored.
Active Exercises[edit | edit source]
Once tissue length is established, the patient should be encouraged to move the affected area of the face actively through the newly gained range.
Electrotherapy[edit | edit source]
While several electrotherapeutic techniques are known to improve soft tissue healing, the face is such a vascular area that in the majority of cases these are not required as the tissue spontaneously heals swiftly and well.
Temporomandibular Joint [TMJ] Rehabilitation[edit | edit source]
- Active and passive joint movements are considered to be an important part of post-operative exercise rehabilitation and long term follow up is recommended[16]
- Active exercises to increase TMJ range of movement. These should include all TMJ movements:
- depression of the mandible = mouth opening
- elevation of the mandible = mouth closing
- lateral movement of the mandible - these actions are used in chewing
- protraction of the mandible
- There are 4 muscles of mastication which act on the TMJ:
- Masseter, Temporalis, Lateral Pterygoid and Medial Pterygoid[14]
- Of the 4 muscles which act on the TMJ, the masseter is the strongest, its action is to close the mouth. If the temporomandibular joint and/or the masseter is injured, the patient will initially have marked weakness of the chewing action.
- There is only one muscle which produces opening of the mouth/mandible depression: Lateral Pterygoid. Injuries to this muscle produce difficulty and weakness in closing the mouth
- Learn more about TMJ Disorders, assessment, and management
Rehabilitation for Injured Facial Muscles[edit | edit source]
Injury to the muscles of the upper face can result in difficulties closing the eye; protection of the eye is of paramount importance. The sphincter muscle of which closes the eye is called orbicularis oculi, so if this muscle is damaged they eye may remain open and be unable to close.
Trauma to the lower facial muscles frequently causes difficulties in eating and drinking. The orbicularis oris muscle controls the movement of the lips, and if injured the person may struggle to drink out of a cup or glass without spilling the fluid, as well as having problems with keeping food in the mouth when eating.
Nerve Injury Rehabilitation - Trigeminal Nerve[edit | edit source]
Damage to the Trigeminal Nerve results in loss of sensation to the skin of the face. Of the three branches of the Trigeminal Nerve, the 3rd branch, V3 known as the Mandibular nerve, is the only one which carries motor fibres; the other two branches, V1 Ophthalmic Nerve and V2 Ophthalmic Nerve, carry only sensory fibres. Thus if the Mandibular nerve is damaged, the power of the chewing function is affected.
Active exercises, and in some cases even Trophic Electrical Stimulation, will be required to restore function and improve ease of eating.
Nerve Injury Rehabilitation - Facial Nerve[edit | edit source]
Trauma to the cheek region can easily result in damage to the facial nerve[18]. Surgical exploration is required to evaluate the condition of the nerve: if it is completely transected, surgical repair or even nerve graft will be performed, and the recovery of active movement will be delayed as the axons grow through the repaired nerve at a rate of approximately 1mm per day.[19]
There are a series of pages on this topic; the main one to consult is the Facial Palsy page.
Very often, if the facial nerve is damaged, the orbicularis oculi muscle is unable to contract, which results in the patient being unable to close the eye,[14] and the eye will not produce tears as this function is also supplied by the facial nerve.[20] The person will need to be taught appropriate eye care (see the Dry Eye page for more detail) including use of artificial lubrication products and how to tape the eye closed at night.
Psychological Effects of Facial Trauma Injury[edit | edit source]
The disfigurement caused by facial injuries can lead to psychological difficulties, ranging from depression, anxiety, a tendency to become socially isolated and in some cases increased hostility[22]. A number of patients report they experience social stigma[23].
Post-traumatic stress disorder PTSD, can occur following facial trauma. One study found that 23% of patients continued to suffer from PTSD one year after the incident[24].
References[edit | edit source]
- ↑ Jordan JR, Calhoun KH. Management of soft tissue trauma and auricular trauma. In Bailey BJ, Johnson JT, Newlands SD, et al. editors. Head & Neck Surgery: Otolaryngology. Hagerstwon, MD: Lippincott Williams & Wilkins.2006. p. 935–36.
- ↑ 2.0 2.1 2.2 Perry M. Advanced Trauma Life Support (ATLS) and facial trauma: can one size fit all? Part 1: dilemmas in the management of the multiply injured patient with coexisting facial injuries. Int J Oral Maxillofac Surg. 2008 Mar;37(3):209-14.
- ↑ Aveta A, Casati P. Soft tissue injuries of the face: early aesthetic reconstruction in polytrauma patients. Ann Ital Chir. 2008 Nov-Dec;79(6):415-7.
- ↑ Kretlow JD, McKnight AJ, Izaddoost SA. Facial soft tissue trauma. Semin Plast Surg. 2010 Nov;24(4):348-56.
- ↑ Wusiman P, Maimaitituerxun B, Saimaiti A, Moming A. Epidemiology and pattern of oral and maxillofacial trauma. Journal of Craniofacial Surgery. 2020 Jul 1;31(5):e517-20.
- ↑ Wood EB, Freer TJ. Incidence and aetiology of facial injuries resulting from motor vehicle accidents in Queensland for a three-year period. Aust Dent J. 2001 Dec;46(4):284-8.
- ↑ Lalloo R, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT et al. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020; 26(Supp 1): i27-i35.
- ↑ 8.0 8.1 Mohanavalli Singaram, Sree Vijayabala G, Rajesh Kumar Udhayakumar. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. J Korean Assoc Oral Maxillofac Surg. 2016 Aug; 42(4): 174–181.
- ↑ 9.0 9.1 Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003 Feb;31(1):51-61.
- ↑ Schneider D, Kämmerer PW, Schön G, Dinu C, Radloff S, Bschorer R. Etiology and injury patterns of maxillofacial fractures from the years 2010 to 2013 in Mecklenburg-Western Pomerania, Germany: A retrospective study of 409 patients. J Craniomaxillofac Surg. 2015 Dec;43(10):1948-51.
- ↑ Einy S, Abdel Rahman N, Siman-Tov M, Aizenbud D, Peleg K. Maxillofacial Trauma Following Road Accidents and Falls. J Craniofac Surg. 2016 Jun;27(4):857-61.
- ↑ Abosadegh MM, Saddki N, Al-Tayar B, Rahman SA. Epidemiology of Maxillofacial Fractures at a Teaching Hospital in Malaysia: A Retrospective Study. Biomed Res Int. 2019 Feb 13;2019:9024763.
- ↑ Ardeshirpour F, Shaye DA, Hilger PA. Improving posttraumatic facial scars. Otolaryngol Clin North Am. 2013 Oct;46(5):867-81.
- ↑ 14.0 14.1 14.2 14.3 Westbrook KE, Nessel TA, Varacallo M. Anatomy, Head and Neck, Facial Muscles. [Updated 2020 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493209/
- ↑ Neural Academy. Muscles of Facial Expression and Mastication. Available from: https://www.youtube.com/watch?v=EUVD8cwKfFQ [last accessed 10/11/2020]
- ↑ Stelea CG, Agop-Forna D, Dragomir R, Ancuţa C, Törok R, Forna NC, Iordache C. Recovery of Post-Traumatic Temporomandibular Joint after Mandibular Fracture Immobilization: A Literature Review. Applied Sciences. 2021 Nov 1;11(21):10239.
- ↑ Functional Anatomy TMJ. Movements of the TMJ. Available from https://www.youtube.com/watch?v=SCS4MiHJ5Xw&feature=emb_logo [last accessed 4/11/2020]
- ↑ V. Bhattacharya Management of soft tissue wounds of the face Indian J Plast Surg. 2012 Sep-Dec; 45(3): 436–443.
- ↑ Martins RS, Bastos D, Siqueira MG, Heise CO, Teixeira MJ. Traumatic injuries of peripheral nerves: a review with emphasis on surgical indication. Arq. Neuro-Psiquiatr. 2013; 71( 10 ): 811-814.
- ↑ Ho J, Markowsky A. Diagnosis and Management of Bell’s Palsy in Primary Care. The Journal for Nurse Practitioners 2022; 18(2):159-163.
- ↑ FacialPalsyUK. Introduction to Paresis. Available from: https://www.youtube.com/watch?v=VuuXqdbhQ6g [last accessed 10/11/2020]
- ↑ Bisson JI, Shepherd JP, Dhutia M. Psychological sequelae of facial trauma. J Trauma. 1997 Sep;43(3):496-500.
- ↑ Newell R, Marks I. Phobic nature of social difficulty in facially disfigured people. Br J Psychiatry. 2000 Feb;176:177-81.
- ↑ Glynn SM, Shetty V, Elliot-Brown K, Leathers R, Belin TR, Wang J. Chronic posttraumatic stress disorder after facial injury: a 1-year prospective cohort study. J Trauma. 2007 Feb;62(2):410-8; discussion 418.