End-Feel: Difference between revisions
Anas Mohamed (talk | contribs) No edit summary |
Anas Mohamed (talk | contribs) No edit summary |
||
| Line 57: | Line 57: | ||
|} | |} | ||
7iouioouippoi[o[i[ | 7iouioouippoi[o[i[ | ||
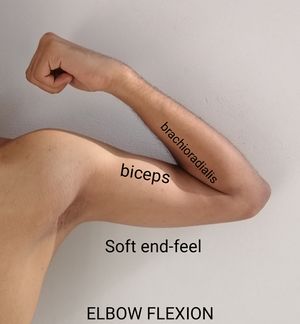
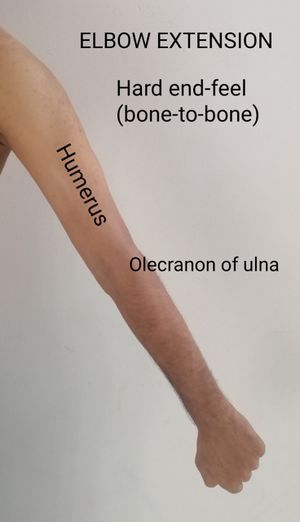
[[File:Elbow flextion end-feel.jpg|alt=Soft end-feel| | [[File:Elbow flextion end-feel.jpg|alt=Soft end-feel|left|thumb|'''Soft end-feel''']] [[File:Elbow extension.jpg|center|thumb]] | ||
[[File:Elbow extension.jpg|center|thumb]] | |||
=== Abnormal end feels (pathological) === | === Abnormal end feels (pathological) === | ||
Revision as of 14:56, 16 February 2020
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Anas Mohamed, Naomi O'Reilly, Lucinda hampton, Ahmed M Diab, Kim Jackson and Shaimaa Eldib
End-Feel[edit | edit source]
An end feel is a type of sensation or feeling which the examiner experienced when the joint is at the end of its available passive range of motion.
The end of each motion at each joint is limited from further movement by particular anatomical structures. The type of structure that limits a joint has a characteristic feel, which may be detected by the therapist performing the passive ROM. This feeling, which is experienced by the therapist as resistance, or a barrier to further motion, is called the end-feel[1]
Purpose[edit | edit source]
An appropriate assessment of end feel can support the examiner
- To assess the type of pathology present[2]
- To identify the limiting structures and choose a focused and effective treatment[2]
- Determine a prognosis for the condition[2]
- And learn the severity or stage of the problem[2]
- By determining if the pain or restriction is the main problem, the examiner can determine if a more gentle treatment should be given (pain predominating) or a more vigorous treatment (restriction predominantly).[2]
Classification[edit | edit source]
The most widely recognized classification developed by cyriax, kaltenborn, and paris[2][1] have described a variety of normal (physiological) and the abnormal (pathological) end feels.
Normal end feels (physiological)[edit | edit source]
The normal end feels are generally described as[edit | edit source]
- Hard: Type of "Bone-to-Bone" stiff sensation that is painless. An example elbow extension
- Soft: There is a yielding compression (mushy feel) that stops further movement or gradual increase in resistance as muscle, skin and subcutaneous tissues are compressed between the body parts. Examples are elbow and knee flexion, which movement stopped by compression of the soft tissues, primarily the muscles[2]
- Firm: There is a hard or firm (springy) type of movement with a slight give. Toward the end of ROM, there is a feeling of springy or elastic resistance. Tissue stretch is the most common type of normal end feel; it is found when the capsule and ligaments are the primary restraints to movement. Examples are lateral rotation of the shoulder, and knee and metacarpophalangeal joint extension.[2]
| End-Feel | Structure | Examples |
|---|---|---|
| Soft | Soft tissue approximation | Knee flexion (contact between soft tissue of posterior leg and posterior thigh) |
| Firm | Muscular stretch | Hip flexion with the knee straight (passive elastic tension of hamstring muscles |
| Capsular stretch | Extension of metacarpophalangeal joints of fingers (tension in the anterior
capsule) | |
| Ligamentous stretch | Forearm supination (tension in the palmar radioulnar ligament of the inferior
radioulnar joint, interosseous membrane, oblique cord) | |
| Hard | Bone contacting bone | Elbow extension (contact between the olecranon process of the ulna and the
olecranon fossa of the humerus |
7iouioouippoi[o[i[
Abnormal end feels (pathological)[edit | edit source]
The Abnormal end feels are generally described as[edit | edit source]
- Soft: Occurs sooner or later in the ROM than is usual or in a joint that Soft tissue edema normally has a firm or hard end. Feels boggy, with a fluid shift.[1]
- Firm: Occurs sooner or later in the ROM than is usual, or in a joint that normally has a soft or hard end.[1]
- Hard: Occurs sooner or later in the ROM than is usual, or in a joint that normally has a soft or firm end. A grating or bony block is felt.[1]
- Empty: No real end because pain prevents reaching the end of ROM.No resistance is felt except for the patient’s protective muscle splinting or muscle spasm.[1]
| End feel | Examples |
|---|---|
| Soft | Soft tissue edema
Synovitis |
| Firm | Increased muscular tonus
Capsular, muscular, ligamentous shortening |
| Hard | Chondromalacia
Osteoarthritis Myositis ossificans Fracture Loose bodies in joint |
| Empty | Acute joint inflammation
Bursitis Abscess Fracture Psychogenic disorder |
Examination[edit | edit source]
Building up the capacity to decide the kind of end feel takes practice and sensitivity.[edit | edit source]
- When assessing passive movement, the examiner should apply overpressure at the end of the ROM to determine the quality of end feel ( the sensation the examiner "feels" in the joint as it reaches the end of the ROM ) of each passive movement.[2]
- Passive ROM, particularly towards the end of the motion, must be performed slowly and carefully when testing end feel.[1]
- Secure stabilization of the bone proximal to the joint being tested is critical in preventing multiple joints and structure from moving and interfering with the determination of the end feel[1]
- To be sure that severe symptoms are not provoked. If the patient is able to hold a position at the end of the physiological ROM (end range of active movement) without provoking symptoms or if the symptoms ease quickly after returning to the resting position, then the end feel can be tested. Pain with pathological end feel is common ( if the patient has severe pain at the end range, end feel should only be tested with extreme care).[2]
| [3] | [4] |
References[edit | edit source]
- Susan B.O'Sullivan, Thomas J. Schmitz, George D. Fulk. Physical Rehabilitation. 6th edition. F. A. Davis Company (2014).
- David J. Magee. Orthopedic Physical Assessment. 6th edition. Elsevier (2014).
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Susan B.O'Sullivan, Thomas J. Schmitz, George D. Fulk. Physical Rehabilitation. 6th edition. F. A. Davis Company (2014).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 David J. Magee. Orthopedic Physical Assessment. 6th edition. Elsevier (2014).
- ↑ Physiotutors. Passive Range of Motion. Available from: https://youtu.be/mspxpap3_gs
- ↑ Physiotutors. Passive Range of Motion (Hip Joint). Available from https://youtu.be/3lTv4gpRWxg